Abstract
Introduction:
Pre-clinical murine experiments and clinical data from allogeneic bone marrow transplantation (allo-BMT) have shown that increased numbers of plasmacytoid dendritic cells (pDC) in the bone marrow graft results in better clinical outcomes with less severe graft-versus-host disease (GvHD) and improved survival. The mechanism by which donor pDC modulate GvHD is unknown. Knowing that vasoactive intestinal polypeptide (VIP) is an immunosuppressive peptide , we reasoned that VIP signaling might play a role in regulating T-cell activation and expansion, and the VIP pathway may be a potential therapeutic target for regulating GvHD in allo-BMT. We have tested the hypothesis that VIP synthesis by donor pDCs can modulate T cell alloreactivity.
Methods:
To explore the mechanisms by which pDC and VIP signaling regulate T cell activation in murine allo-BMT, we prepared B6-background donor cell grafts and transplanted them into lethally irradiated B10.BR recipients. In experiment 1, recipients were transplanted with grafts containing the combination of 5 x 103 VIP-GFP hematopoietic stem cells (HSC) and 3 x 106 VIP-wild type (VIP-WT) or VIP-knock out (VIP-KO) splenocytes. At day 7, splenocytes were isolated for flow cytometric analysis looking for GFP signal, which represents VIP-promotor activity. Experiment 2 used combinations of 5 x 103 VIP-WT HSC, 1 x 106 luciferase+ T cells, and 50 x 103 VIP-WT or VIP-KO pDC from B6 as donor grafts. Recipients were monitored for survival and GvHD based on fur texture, posture, activity, skin integrity and weight loss. T cell expansion was measured by bioluminescent imaging (BLI). Serum cytokines from bleeds at day 3 and day 8 post-transplant were analyzed using a Luminex 38 plex panel. Some recipients were euthanized on day 3 for intracellular cytokine analysis of splenic T cells.
Results:
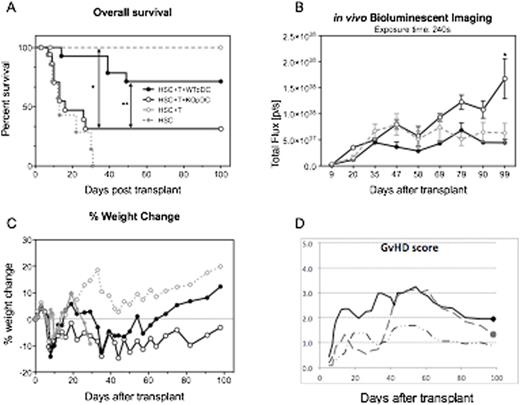
In experiment 1, 7 days post-transplant, analysis of splenocytes from all mice showed increased activity of the VIP gene promoter in donor pDC that were derived from HSC, compared to other cell types. The VIP promoter signal was also stronger in donor HSC-derived pDCs, if originally transplanted with VIP-KO splenocytes. In experiment 2 over 70% of mice receiving HSC+T+VIP-WT pDC in the BM graft survived to day 100 post-transplant, while those getting VIP-KO pDC instead only had 30% survival (Fig 1A). All surviving recipients were fully engrafted by day 30. BLI revealed greater total T-cell proliferation (measured as radiance) in recipients of VIP-KO pDC (Fig 1B). Furthermore, recipients of VIP-KO pDC had more severe acute GvHD, with increased weight loss and GvHD clinical scores (Fig 1C, 1D). Some recipients were euthanized and their serum were collected for cytokine analysis on day 8 post-transplant, which showed up-regulation of pro-inflammatory or chemotactic cytokines MCP1, IL-1, IL-12, IL-17 in T cells co-transplanted with VIP-KO pDC compared to WT pDC.
Conclusion:
The present findings show that: 1) VIP is produced by donor pDC early after allo-BMT; 2) absence of VIP production by donor pDC leads to increased T-cell expansion in a murine allo-BMT model. Thus the pDC-T cell VIP signaling pathway is a critical element in controlling donor T cell alloreactivity after allo-BMT. Future studies will include VIP qPCR to confirm VIP production in donor pDC post-transplant, and determine the mechanism by which VIP production by pDC regulates T cell activity and modulates GvHD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal