Abstract

Background
Ibrutinib (IB) is Food and Drug Administration approved for chronic lymphocytic leukemia (CLL), mantle cell lymphoma (MCL), and Waldenström's macroglobulinemia (WM). High overall response rates, extended progression free survival, and an acceptable adverse event profile make IB an impactful therapy for these malignancies. Atrial fibrillation (AF) has been identified as a less common but serious adverse effect of IB with reported incidence ranging from 2-16% in clinical trials and post-marketing experience. AF can be associated with significant morbidity and mortality, including congestive heart failure and embolic events such as stroke. Data regarding the management of AF in this patient population is thus far limited. Embolic stroke prevention poses a particular clinical challenge as IB carries an inherent bleeding risk that may be increased by antiplatelet therapy and therapeutic anticoagulation. We report the management and outcomes of a large cohort of patients who developed AF while on IB therapy.
Methods
Patients with hematological malignancies and incident or recurrent AF while on IB therapy at the Ohio State University were identified retrospectively. Incident AF was defined as new onset AF in patients without a history AF and recurrent AF as an AF event requiring new intervention in patients with a prior history of AF. Data pertaining to patient demographics, comorbid conditions, AF events, AF management, stroke prevention strategies, and complications of AF therapy were collected. AF events were graded according to Common Terminology Criteria for Adverse Events (CTCAE) v4.0 andcongestive heart failure, hypertension, age, diabetes mellitus, stroke (CHADs2) scores were calculated. Major bleeding was defined as a decrease in hemoglobin of 2g/dL or more, requiring a transfusion of 2 or more units of packed red blood cells or whole blood, occurring in a critical site, or contributing to death. Clinically relevant non-major bleeding events were graded according to CTCAE criteria. Management strategies and outcomes are summarized.
Results
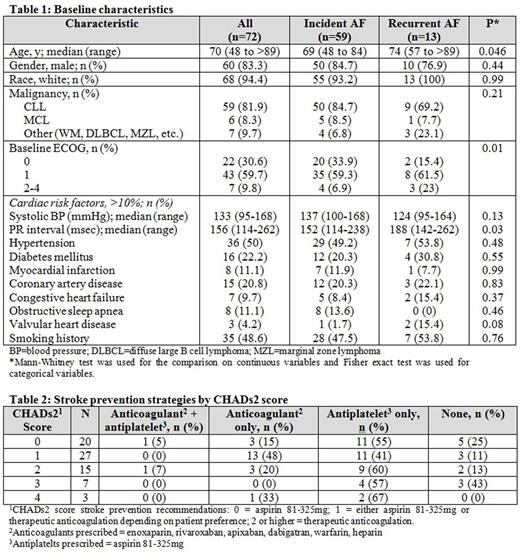
Seventy-two patients with incident or recurrent AF were identified. Fifty-nine patients developed incident AF while 13 patients developed recurrent AF while on IB. Baseline characteristics are presented in Table 1.Patients with recurrent AF were older, had worse baseline ECOG performance status, and longer baseline PR interval on electrocardiogram assessment.Patients were followed for a median of 4.3 years from the start of ibrutinib and 1.7 years from AF event.Ninety-three percent of the AF events were grade 1-2 and 7% were grade 3. First-line therapy forAF included rate-control for 54 (75%) patients, interventional procedural strategies for 8 (11.1%), and rhythm-control for 3 (4.2%). Seven (9.7%) patients required no intervention. Twenty-two patients (30.5%) required a second and 4 (5.5%) required third-line AF management intervention. Among those with a secondary AF management strategy, rhythm control was the most frequently utilized (n=10, 45.5%). During the AF events, 31 (43.1%) patients continued IB, 35 (48.6%) temporarily held IB, 5 (6.9%) discontinued IB, and one patient had the dose reduced. Stroke prevention strategies are described in Table 2. Patients with recurrent AF were less likely to be treated with anticoagulation when compared to patients with incident AF. Six (8.3%) patients had a major bleeding event and 2 of these patients went on to have a second major bleed. Of the 8 major bleeding events, 3 occurred with concomitant antiplatelet therapy and no patients were on anticoagulation therapy at the time of bleeding. Eighteen (25%) patients developed a total of 25 clinically relevant non-major bleeding events (9 grade 1 events, 13 grade 2 events, 2 grade 3 events, and 1 could not be graded). Only one potential embolic event occurred in a patient with a CHADs2 score of 1 on aspirin 325mg who developed symptoms consistent with stroke.
Conclusions
AF events in patients being treated with IB are generally manageable and in the majority of cases did not result in IB discontinuation. Clinically relevant bleeding events are common, and caution must be exercised when initiating routine antiplatelet therapy and/or anticoagulation in patients with IB. Risk of ischemic stroke was low in our patient population, though follow up was limited. The optimum strategy for stroke prophylaxis in patients with concurrent IB is unclear.
Christian:Pharmacyclics: Research Funding; Janssen: Research Funding. Porcu:miRagen: Other: Investigator in a clinical trial; Innate Pharma: Other: Investigator in a clinical trial; celgene: Other: Investigator in a clinical trial; Millenium: Other: investigator in a clinical trial. Woyach:Morphosys: Research Funding; Karyopharm: Research Funding; Acerta: Research Funding. Jones:AbbVie: Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen: Membership on an entity's Board of Directors or advisory committees, Research Funding; Pharmacyclics, LLC, an AbbVie Company: Membership on an entity's Board of Directors or advisory committees, Research Funding. Awan:Innate Pharma: Research Funding; Novartis Oncology: Consultancy; Pharmacyclics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal