Abstract

RBC-transfusion dependency (RBC-TD) is an independent prognostic factor for poor survival in the WHO classification-based prognostic scoring system (WPSS) for MDS patients. However, WPSS did not include cytopenia, whereas revised International prognostic Scoring System (IPSS-R) includedthree haemoglobincut-offs, which were thought to substitute for RBC-TD. Thus, none of these prognostic scoring systems incorporates both cytopenia and RBC-TD. We aimed to test whether RBC-TD adds prognostic value to the IPSS-R, in addition to that offered by haemoglobin levels at diagnosis. South Australian MDS registry (SA-MDS registry) data were used to derive a prognostic index while Dusseldorf registry (Germany) data was used as a validation cohort.
Inclusion criteria for this study were: primary MDS not treated with disease-modifying therapy, bone marrow blasts ≤30% and peripheral blasts ≤20%. RBC TD was defined as at least one unit of packed red cells transfused every eight weeks for four months (mos), according to WPSS classification. In this study IPSS-R was calculated at the time of diagnosis and the RBC-TD was continuously reassessed after diagnosis.
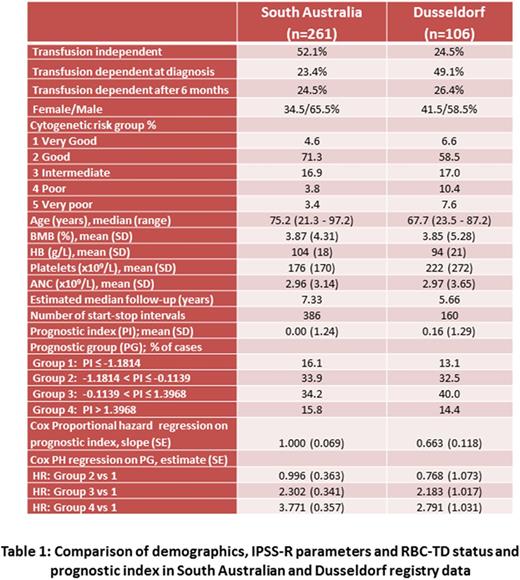
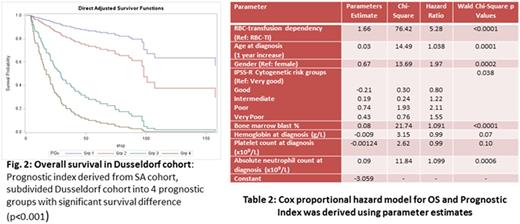
In South Australian Registry, the prevalence of RBC-TD at diagnosis was 61/295 (20.7%), while the incidence of RBC-TD during follow-up was 64/234 (27.4%; Table I). The poor prognosis associated with RBC-TD was demonstrated in a series of landmark analyses. The median overall survival (OS) of RBC-TD patients was significantly inferior to RBC transfusion independent (RBC-TI) patients at 6mos (18 vs. 64 months; n=255; p < 0.0001), 12mos (24 vs. 71 months; n=231; p < 0.0001) and 24mos (40 vs. 87 months; p < 0.0001; n=173; Fig 1A-C). Subgroup analysis of IPSS-R Low and Intermediate risk groups also showed inferior OS in RBC-TD compared to RBC-TI within each risk category. The adverse prognosis of RBC-TD was substantiated in multivariate analysis using a Cox-proportional regression model. We tested 46 models and in each of the three models with least Akaike Information Criterion (AIC) or minimum AIC difference RBC-TD wasan independent adverse prognostic marker in addition to age, sex, and IPSS-R variables(Wald test; P<0.0001). In the best-fitting model, the IPSS-R variables were used as continuous variables (except IPSS-R cytogenetic risk groups).This Cox-proportional regression model (Table 2) was used to derive a prognostic index using cut-off points determined by Cox's method and was validated in the Dusseldorf cohort.
Dusseldorf validation cohort: This cohort consisted of 106 patients (160 start-stop intervals) with a median follow-up of 5.66 years. Cox proportional hazard regression of OS on the prognostic index resulted in a slope coefficient of 0.663 in the validation cohort. This difference in slope could be due to differences between the datasets: e.g. the validation cohort comprised younger patients, more patients with RBC-TD at diagnosis and fewer cases with favourable cytogenetic risk (Table 1).
The validation cohort was divided into four prognostic groups using cut-offs determined by Cox's method (derivation dataset). Cox-proportional hazard regression of OS showed significant OS difference between the four prognostic groups (p<0.001) and significantly higher risk of death in groups 3 (p=0.032) and 4 (p=0.007) relative to group 1 (Table 1).
Conclusion: Multivariate analysis by Cox proportional hazards regression and serial landmark analysisof dataset clearly demonstrates that development of RBC-TD at any time during the disease course is associated with poor OS, independent of IPSS-R. This was confirmed in the Dusseldorf validation cohort. This is the first report demonstrating that inclusion of RBC-TD can refine the IPSS-R. Furthermore, despite inclusion of three haemoglobin cut-off values in the IPSS-R model, the onset of RBC-TD during follow-up provides additional prognostic value and could be included in future prognostic scoring systems and in treatment decision algorithms for MDS patients.
Ross:Novartis Pharmaceuticals: Honoraria, Research Funding; BMS: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal