Abstract

Background
Little is known about racial disparities amongst patients with MDS. The incidence of MDS is higher in Caucasians, who represent the majority of patients included on clinical trials. We explored the differences in disease features and outcomes between Caucasians, African Americans (AA), and Hispanics.
Methods
Using our MDS database, patients with a diagnosis of MDS were identified and categorized into the aforementioned racial groups. We compared baseline characteristics, risk stratification, treatment, and overall survival (OS). Data on recurrent somatic mutations (SM) by next generation sequencing was available for 349 patients and compared between the groups.
Results
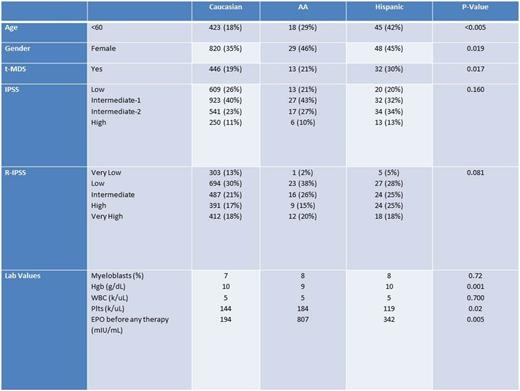
Among 2538 MDS patients, 63 (2%) patients were AA and 107 (4%) were Hispanic. Table-1 summarizes baseline characteristics. In Hispanic patients, 42% were <60 years, 30% had t-MDS, and the mean platelet (plt) count was lower. In AA patients, the mean hemoglobin (hgb) was lower and the serum EPO was higher. More Hispanic and AA females were diagnosed with MDS compared to Caucasians.
A higher percentage of Hispanic patients underwent allogenic stem cell transplant (33% versus 13% in Caucasian and 10% in AA) (p= <.005). There was no difference in treatment with hypomethylating agents or lenalidomide. Only 1 AA and 7 Hispanic patients were enrolled on clinical trials, compared to 113 Caucasians. Among patients evaluable for response, none of the 7 AA patients treated with erythroid stimulating agents (ESA) had a hematologic improvement, compared to 10% among Hispanics and 39% in Caucasians.
The median OS was 37, 30, and 47 months (mo) among Caucasian, AA, Hispanic (p=0.022). Among patients with low/int-1 risk IPSS, the median OS was 55, 45, and 81 mo respectively (p=0.1), and among int-2/high risk IPSS, the median OS was 17, 17, 26 mo respectively (p=0.1). There was no difference in the rate of AML transformation.
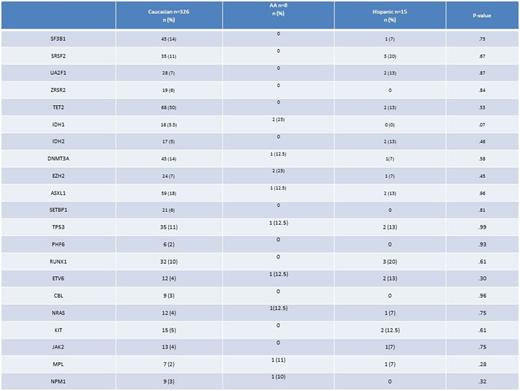
Data on 349 patients who had recurrent somatic mutation (326 Caucasian, 8 AA, and 15 Hispanic) were reviewed. The most common somatic mutations in Caucasian patients were TET-2 30%, ASXL-1 18%, SF3B1 14%, DNMT3A 14%, SRSF2 11% and p53 11%. In AA, the most common SM were IDH1 25%, EZH2 25%, DNMT3A, ASXL-1, TP53, ETV6, NRAS, in13% each. The most common SM in Hispanic patients were SRSF2 20%, RUNX-1 20%, TET-2, IDH-2, UA2F1, ASXL-1 and p53 in 13% for each. No splicing mutation or TET-2 was observed among AA patients. There was a higher trend for IDH-1 mutation among AA (25%) vs 6% in Caucasian and none in Hispanic (p=.07).
Conclusion
We observed differences in several baseline characteristics between races. Hispanic patients were younger, had more therapy related MDS and thrombocytopenia. AA patients had higher serum EPO levels and decreased response to ESAs. Hispanic patients had better overall survival, especially in lower risk disease. Preliminary data suggests potential racial differences in recurrent somatic mutations observed in MDS.
Baseline characteristics
Recurrent somatic mutations
Sweet:Novartis: Consultancy, Speakers Bureau; Pfizer: Speakers Bureau; Ariad: Consultancy, Speakers Bureau; Incyte Corporation: Research Funding; Karyopharm: Honoraria, Research Funding. Komrokji:Novartis: Consultancy, Speakers Bureau; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal