Abstract

Background: Somatic mutations occur frequently in patients with MF and have been shown to correlate with clinical presentation and outcome. Newer prognostic models integrate molecular data to better identify high-risk patient populations. We attempted to characterize the mutational landscape and correlate mutations with clinical presentation, response to treatment and outcomes.
Methods: This was a single institution, retrospective study of patients with a diagnosis of MF seen at our center between 2/2001 and 6/2016. Somatic mutation data was assessed in patients who had undergone next generation sequencing with targeted myeloid panels at the time of referral to our center. Gene classes were defined as previously reported in the literature (Patnaik, Blood Cancer J, 2016).
Results: We identified 104 eligible MF patients (median age at diagnosis 72 years; 60% males). The cohort was comprised of PMF (80%), post-PV MF (14%) and post-ET MF (7%) patients. DIPPS-plus risk score was high in 27% of patients, intermediate-2 in 41%, intermediate-1 in 28%, and low in 4%. Frequencies of driver mutations were 65% for JAK2V617F, 16% for CALR (14/17 type 1 or type 1-like)and 8% for MPL with 11% of patients classified as "triple-negative."
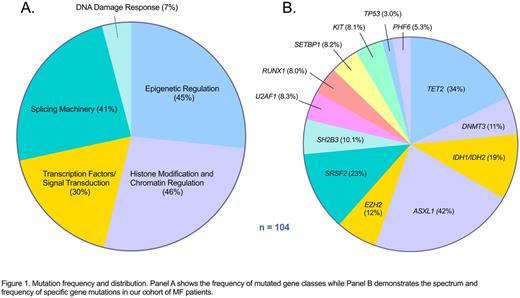
The frequencies of mutations were 34% for TET2, 42% ASXL1, 12% EZH2, 19% IDH1/IDH2, 11% DNMT3, and 23% SRSF2 (figure 1). All other mutational frequencies occurred in less than 10% of patients. No somatic mutations were seen in 12%, 1 mutation in 22%, 2 mutations in 22%, 3 mutations in 20%, and 4+ mutations in 24%. When grouped in terms of gene function, 45% had a mutation in an epigenetic regulation gene (TET2, DNMT3, IDH1/2), 46% in a gene involved in histone modification/chromatin regulation (ASXL1, EZH2), 41% in a splicing gene (SF3B1, SRSF2, U2AF1, ZRSR2), 30% in a signal transduction gene (KRAS, NRAS, CBL, FLT3, RUNX1, SETBP1), and 7% in a DNA damage response gene (TP53 and PHF6). Mutations in a single gene group were seen in 33% of patients, with 27% having mutations in 2 classes, 16% in 3 classes, and 9% involving 4 separate gene classes.
Mutations in epigenetic regulatory genes correlated with increased monocyte count (p = 0.03) and transformation to blast phase (BP) (p = 0.04). Mutations in genes involved in histone modification correlated with increased number of immature myeloid cells (p = 0.001), decreased hemoglobin (p = 0.02), thrombocytopenia (p = 0.009), increased LDH (p = 0.02), increased DIPSS and DIPSS+ (p = 0.002 and 0.001) and were more likely to be transfusion dependent (OR: 3.67 [1.47-9.04]; p = 0.007). Splicing machinery mutations correlated with older age at presentation (p = 0.002). Mutations in signal transduction genes correlated with increased monocyte count (p = 0.006), increased peripheral blasts (p = 0.02) and BP transformation (p = 0.001). ASXL1 was associated with a better response to erythropoiesis-stimulating agents (p = 0.04). The number of individual mutations and affected gene classes correlated with age at diagnosis (p = 0.01 and 0.007).
CALRmut MF was associated with improved overall survival (OS) as compared to JAK2V617F or MPLmut MF (HR 0.38 [0.17-0.85], p = 0.02). Triple-negative MF had inferior 2-yr survival of 65% as compared to 83% in JAK2/MPL mutated MF.
SRSF2 mutations were associated with inferior OS (HR: 2.99 [1.03-8.69]; p = 0.04), whereas ASXL1 had a trend towards inferior OS (HR 2.09 [0.90-4.84]; p = 0.09. In multivariate regression analysis, controlling for DIPSS, SRSF2 remained significantly associated with OS (p = 0.02). An increased number of somatic mutations was associated with worse OS (HR 1.21 [1.03-1.43], p = 0.02) as was an increased number of affected gene classes.
Conclusion: Somatic mutations correlate with clinical features of MF and few carry prognostic significance. SRSF2 mutations have prognostic effects independent of currently utilized risk scores, while the impact of ASXL1 was less clear and potentially captured in standard risk models. Additionally, we showed that mutation burden holds prognostic significance both in terms of quantity of mutations as well as number of affected classes.
Lancet:Amgen: Consultancy; Novartis: Consultancy; Karyopharm: Consultancy; Kalo Bios: Consultancy; Jazz Pharmaceuticals: Consultancy; Biopath Holdings: Consultancy; ERYtech: Consultancy; Pfizer: Research Funding; Quantum First: Consultancy; Boehringer-Ingelheim: Consultancy; Baxalta: Consultancy; Celgene: Consultancy, Research Funding; Seattle Genetics: Consultancy. Sweet:Pfizer: Speakers Bureau; Incyte Corporation: Research Funding; Ariad: Consultancy, Speakers Bureau; Novartis: Consultancy, Speakers Bureau; Karyopharm: Honoraria, Research Funding. Komrokji:Novartis: Consultancy, Speakers Bureau; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal