Abstract
We investigated a cohort of 200 patients diagnosed with essential thrombocythemia (ET, N=115) or prefibrotic primary myelofibrosis (prePMF, N=85). All diagnoses were performed by strictly adhering to the 2016 WHO criteria. Investigations into the molecular genetic markup of these patients were performed using next generation sequencing methods for the main genes involved in myeloproliferative neoplasms, JAK2, CALR and MPL. Additionally, four more genes considered as the most commonly mutations associated with an elevated risk for early death or leukemic transformation in PMF, comprising of ASXL1, EZH1, IDH1/2 and SRSF2 were analyzed.
The median age at diagnosis in the cohort was 58,8 years, 56,4 years for ET patients and 60,7 years for prePMF patients. Median observation time was 8 years, 8,5 years in the ET group and 7,4 years in the prePMF group. 120 (60%) patients were JAK2V617F positive, 75 (65,2%) ET and 45 (52,9%) prePMF. 54 (27%) patients showed CALR positivity, 21 (18,3%) ET and 33 (38,8%) prePMF. Only a few patients were MPL positive, 8 (4%) in the whole cohort, 4 (3,5%9 ET and 4 (4,7%) prePMF. Triple negative patients, showing none of the above three mutations were 18 (9%), 15 ET (13%) and 3 prePMF (3,5%).
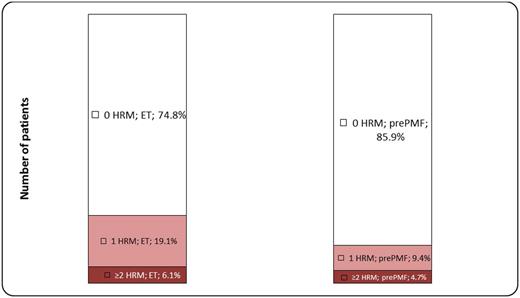
We investigated, whether the presence or number of high molecular risk mutations between the two diagnostic groups had an effect on overall survival. Each group was divided into two categories: patients with no high molecular risk mutation and patients with one or more high molecular risk mutations. Among the ET patients, 86 (74,8%) showed no such mutation, whereas 29 (25,2%) had one or more. In the prePMF group, 73 (85,9%) displayed no mutation and 12 (14,1%) having one or more. The difference between ET and prePMF regarding the number of high molecular risk mutations was not statistically significant (p=0,075678).
Additionally, we examined the difference within each diagnostic group (Figure 1). Here, we divided each portion of the cohort into three categories: patients with no high molecular risk mutation, patients with one high molecular risk mutation and patients with two or more high molecular risk mutations. Of the 29 ET patients with one or more high molecular risk mutations, 7 had two or more, of the 12 prePMF patients 4 respectively.
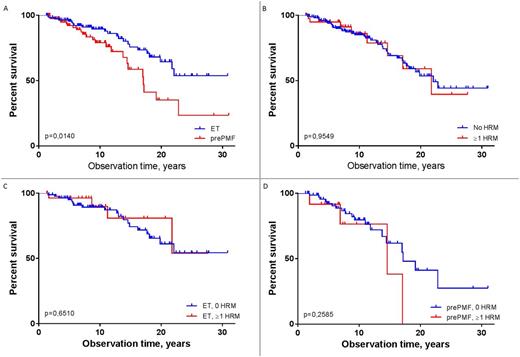
Comparing the overall survival between ET and prePMF patients, a clear significant difference favoring ET patients could be observed (Figure 2A). No significant difference regarding overall survival was detected between patients with or without one or more high molecular risk mutations (Figure 2B). Looking at differences in overall survival within each diagnostic group with regards to the number of high molecular risk mutations, neither in the ET nor in the prePMF cohort a significant difference could be found (Figure 2C, D).
In conclusion, our investigation shows that the most common high molecular risk mutations have no significant impact on overall survival in WHO-defined ET and prePMF patients.
Proportions of high molecular risk mutations (HRM) in ET and prePMF patients
Overall survival of (A) ET versus prePMF patients, (B) patients without versus patients with one or more high molecular risk mutations, (C) ET patients with and without high molecular risk mutations and (D) prePMF patients with and without high molecular risk mutations.
Overall survival of (A) ET versus prePMF patients, (B) patients without versus patients with one or more high molecular risk mutations, (C) ET patients with and without high molecular risk mutations and (D) prePMF patients with and without high molecular risk mutations.
Gisslinger:AOP Orphan: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; Baxalta: Consultancy, Honoraria. Thiele:Novartis: Consultancy, Honoraria; Incyte Corporation: Consultancy, Honoraria. Kralovics:Qiagen: Membership on an entity's Board of Directors or advisory committees; AOP Orphan: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal