Abstract

Introduction. The application of Pediatric-Type Therapy (PTT) programs to adults with ALL can improve outcome significantly despite higher age-related toxicity. Recent series reported survival rates ≥ 50%, but only few combined PTT with Minimal Residual Disease (MRD) study for risk-oriented Hematopoietic Cell Transplantation (HCT) and/or explored the value of specific PTT element such as higher dose, lineage-targeted MTX up to 5 g/m2.
Methods. To improve over prior data, NILG protocol 10/07 (Clinical.Trials.gov NCT-00795756) for unselected adult patients aged 18-65 years combined PTT together with MRD study for risk/MRD-based HCT. The 8-course program consisted of a 5-drug complete remission (CR) induction (cycle no. 1; imatinib added if Ph+) followed by 3 modified BFM blocks (no. 2, 4 and 6), 3 lineage-targeted MTX blocks (no. 3, 5 and 7; MTX 5 g/m2 for T-ALL and 2.5 g/m2 for B-ALL [1.5 g/m2 if age > 55 years or Ph+]; no. 3 and 7 with high-dose Ara-C 2 g/m2 x4, no. 5 with L-Asp 10,000 IU/m2 x2) and reinduction (no. 8). CNS prophylaxis was with triple intrathecals or liposomal cytarabine (Haematologica 2015;100:786). MRD was studied molecularly with sensitive probe(s) (sensitivity 10-4 or greater) on marrow samples obtained at end of induction (week 4, w4) and after cycles 3 (w10), 5 (w16), 7 (w22) i.e. after 1st, 2nd and 3rd lineage-targeted MTX block. Patients were risk-stratified at diagnosis and after MRD analysis for the purpose of allocation to HCT or conventional maintenance. The HCT allocation cohort consisted of predefined very high-risk patients (vHR: WBC >100, highly adverse cytogenetics, pre-T/mature T-ALL) regardless of MRD, of HR patients without MRD study (HR: late CR; B-ALL with WBC >30 or pro-B phenotype), and of HR or standard-risk (SR) patients with MRD ≥ 10-4 at w10/16 or positive at w22. Conversely, the maintenance allocation cohort consisted of SR and HR patients with MRD < 10-4 at w10/16 and negative at w22 and of SR patients without MRD study. A family related/unrelated donor search was activated at diagnosis in order to proceed to HCT soon after cycle no. 3 when needed.
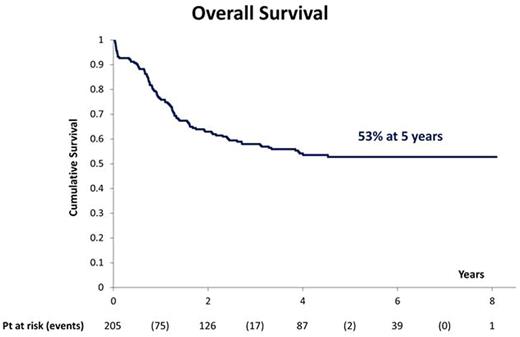
Results. 205 patients were enrolled, with a median age of 41 years (range 17-67 years, 11% > 60 years). 55% were male, 42 had Ph+ ALL, 119 Ph- B-ALL and 44 T-ALL. Of 163 patients with Ph- ALL, 45% were SR, 13% HR and 42% vHR. CR rate was 98% in Ph+ ALL and T-ALL, and 83% in Ph- B-ALL (88% vs 58% in patients ≤ vs > 60 years, P .0013). The MRD study was successful in 109/142 CR patients with Ph- ALL (77%), contributing to the final risk classification in 63 patients, of whom 41 were MRD responsive (65%) and 22 MRD resistant (35%). Altogether, 55 CR patients constituted the maintenance allocation group (39%) and 87 the HCT allocation group (61%), which included mainly vHR patients (n=61, 43%) selected for HCT independently of MRD study results. According to intention-to-treat, median OS is not reached (53% at 5 years, figure) and median DFS is 4.8 years (48% at 5 years). In Ph- ALL, 5-year OS/DFS are 74%/61% in T-ALL (medians not reached) and 48% each in B-ALL (medians 3.9 and 4.7 years). Median OS is not reached in both HCT and maintenance allocation groups (58% and 73% at 5 years, respectively, P .078), with a median DFS of 4.7 years (48% at 5 years) versus not reached (59% at 5 years) (P .19). Treatment adherence was good with some exceptions in maintenance allocation group (6 HCT, 11%) and a transplant realization of 68% (53 allogeneic; 6 autologous) in HCT allocation group. With HCT, 5-year incidence of nonrelapse mortality was 17%. The MRD analysis proved that DFS of patients achieving an MRD response <10-4 at w4 (n=46/90, 51%) or w10 (n=76/107, 71%) was significantly improved compared to those with MRD ≥ 10-4, with median not reached and 5-year rate 67% versus 4.5 years and 41% (w4 MRD; P .041), and 7.2 years and 64% versus 1 year and 23% (w10 MRD; P .0001).
Conclusion. The current PTT and MRD-based risk-oriented strategy was applicable to adults with ALL in a wide age range, with some limitations in patients > 60 years. 5-year OS and DFS of 55% and 52% respectively in Ph- patients aged up to 65 years represent an improvement over prior NILG study (5-year OS and DFS of 36% and 35% respectively). MRD was essential in orientating the HCT choice in SR and HR patients and retained a major prognostic role in all patients. Optimizing the early MRD response with new immunotherapeutics and clarifying the role of HCT in MRD responsive vHR patients are some relevant topics of future research.
Ciceri:MolMed SpA: Consultancy. Vitolo:Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Honoraria; Gilead: Honoraria; Celgene: Honoraria; Roche: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Gallamini:Millenium Takeda: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal