Abstract
Background. About 25-35% of adult patients with acute lymphoblastic leukemia (ALL) show the Philadelphia (Ph) chromosome. Their outcome has improved with the combination of tyrosine kinase inhibitors (TKI) and chemotherapy, generally followed by allogeneic hematopoietic stem cell transplantation (alloHSCT). However, few series have evaluated the prognostic value of the additional cytogenetic alterations (ACA) to the Ph chromosome, with contradictory results. The aim of this study was to analyse the frequency, type and prognostic significance of ACA to the Ph chromosome in young adults with Ph+ ALL treated with the ALL Ph-08 trial from the PETHEMA group.
Patients and methods.Between 2008 and 2016, 95 patients with Ph+ ALL from 30 Spanish hospitals were included in the ALL Ph08 trial. This trial includes concurrent administration of imatinib (600 mg/d) and standard induction and consolidation chemotherapy, followed by alloHSCT (or autologous HSCT if alloHSCT not feasible) and maintenance chemotherapy with imatinib in cases of MRD persistence of reappearance after alloHSCT (Ribera et al, Br J Haematol 2012; 159: 78-81). The cytogenetic reports were centrally reviewed. Major molecular response (MMR) was defined as BCR-ABL/ABL ratio ²0.1% and complete molecular response (CMR) as BCR-ABL/ABL ratio ²0.01% or undetectable.
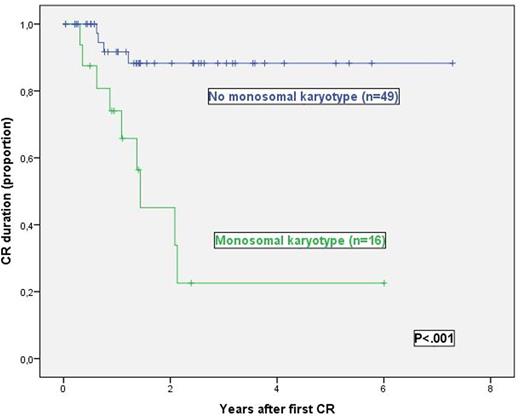
Results. In 74 out of 95 patients the karyotype was evaluable after review (in the remaining 21 cases the diagnosis was carried out by FISH [n=9] or PCR [n=12]). The median age of the 74 patients was 39 years (limits 19-63) and 44 patients (59%) were males. The median WBC count was 17.6x109/L (limits 0.2-390) and 8 out of 66 evaluable patients had CNS involvement at diagnosis. The CR rate was achieved in 72/74 patients (97%) (1 patient did not achieve CR and 1 died during induction therapy). To date, 57 patients underwent to HSCT, of them 46 were in MMR, at least, at the time of HSCT. With a median follow-up of 1.89 years (limits 0.10-7.38) the probabilities of the CR duration, OS and EFS at 4 years were 69% (95%CI: 54%-84%), 39% (23%-55%) and 38% (23%-53%), respectively. Out of 74 patients, 52 (70%) showed at least one ACA and in the remaining 22 (30%) the t(9;22) was the only cytogenetic alteration. No clinical or biologic differences were observed on comparison of the two groups of patients. Twenty (27%) out of 73 evaluable patients showed trisomies and 19 (26%) monosomies. No differences in CR attainment were observed according the presence and type of ACA. The 4-yr. probability of CR duration in patients with t(9;22) and one or more monosomies (monosomal karyotype) vs. those without monosomies was 23% (95%CI: 0%;49%) vs. 88% (77%;99%) (p<0.001) and the 4-yr. EFS probability was 15% (95%CI: 0%;34%) vs. 48% (30%;66%) (p=0.032). Patients with one or more trisomies showed better CR duration probability at 4-years (86% [95%CI: 60%;100%] vs. 60% [42%-78%], p=0.040).The probability of CR duration was higher in patients who achieved MMR before HSCT (79% [63%-95%] vs. 38% [0%-77%], p=0.021). No other clinical or biologic parameter showed prognostic significance. By multivariate analysis the only variable with prognostic impact for CR duration and EFS was the presence of monosomal karyotype (HR [95%CI] 7.95 [2.04-30.95], p=0.003 and 2.18 [1.05-4.51], p=0.036, respectively).
Conclusions. In young patients with Ph+ ALL treated within the ALL Ph08 trial, the frequency of ACA was high, being trisomies and monosomies shown in similar frequency. The monosomal karyotype was the most important unfavourable prognostic factor in this series of patients.
Funded in part by grants PI10/01417 (FIS), RD12-0036-0029 from RTICC, Instituto Carlos III and RD14-SGR225(GRE), Generalitat de Catalunya.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal