Abstract
Background: Acute lymphoblastic leukemia (ALL) represents 20% of adult leukemias. With the optimization of doses and schedules of chemotherapy regimens, and incorporation of targeted agents into adult therapy, over 80% of adults with ALL attain a complete remission. However, the majority will ultimately relapse and the utility of prognostic criteria in predicting long-term survival at the time of 1st relapse has not been fully elucidated. We investigated the prognostic significance of neutrophil and platelet count recovery after salvage therapy in predicting long-term survival after second complete response [complete remission (CR), CR with incomplete platelet count recovery (CRp), or CR with incomplete neutrophil count recovery (CRi)] in adult patients (pts) with ALL.
Methods: ALL pts at Cleveland Clinic, University of Washington, and Stanford treated during the yrs 1997-2015 were included. A total of 87 adult pts with ALL who achieved CR1 after induction treatment but subsequently relapsed and achieved second complete response with salvage therapy were analyzed. Pts refractory to salvage treatment and cases with isolated extramedullary relapse were excluded. Response to salvage treatment was assessed. CR was defined as <5% blasts with an absolute neutrophil count (ANC) of ≥1000/uL and platelets ≥100,000/uL; CRi: same as CR but ANC <1000/uL; CRp: same as CR but platelets <100,000/uL. Cases with both incomplete ANC and platelet recovery were categorized as CRi. Minimal residual disease (MRD) was assessed by ten-color flow cytometry and any abnormal blast population was considered MRD positive. Cytogenetic (CG) risk was ascribed by CALGB criteria.
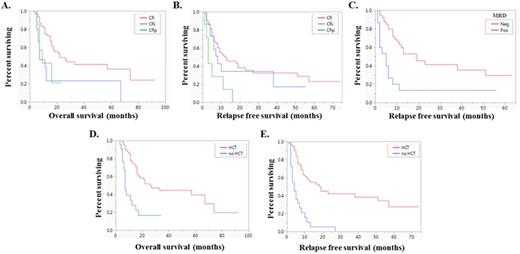
Results: Of 87 pts included, the median age was 37 yrs (range, 18-76) at diagnosis and 38 yrs (range, 20-73) at relapse. Fifty-five percent were males, 69% were Caucasian, 84% had B-ALL, and 23% had extramedullary involvement in addition to bone marrow involvement. Age, sex, race, immunophenotype and extramedullary involvement had no impact on overall survival (OS) or relapse-free survival (RFS) after first relapse. Sixty-eight percent of pts had available CG data at relapse, and of these, 39% had normal CG, while 37% were poor risk and 24% were grouped in "others". Of the poor risk pts, 68% were Ph+. CG risk at relapse had no impact on OS or RFS after first relapse. Relapse therapies included hyper-CVAD: 26%, high dose cytarabine: 17%; BFM-based regimens: 17%; inotuzumab: 13%; nelarabine: 8%; blinatumomab: 5%; and 14% of pts received other regimens. In addition, 70% of Ph+ pts received tyrosine kinase inhibitors in combination with salvage chemotherapy. Best response achieved was CR in 72%, CRp in 19%, and CRi in 9% of pts. Among 55 pts with MRD assessment following response to relapse therapy, 27% were MRD positive. The frequency of MRD positivity was significantly higher in pts with CRi (100%) as compared to CR (26%) and CRp (11%) (p=0.009). Pts with CRp or CRi after salvage treatment had worse OS compared to those with CR (p=0.006) (Figure 1A). Moreover, pts with CRi had worse RFS than those who attained CR or CRp (p=0.008) (Figure 1B). MRD positivity at the time of relapse response did not impact OS (p=0.48), but MRD negative pts had significantly better RFS than pts with MRD positivity (p<0.001) (Figure 1C). Sixty percent of pts received hematopoietic stem cell transplant (HCT) after salvage therapy in CR2, and 14% had HCT before relapse in CR1. Pts receiving HCT after salvage therapy had significantly longer OS (p<0.001) (Figure 1D) and RFS (p<0.001) (Figure 1E) than pts without HCT. Multivariable cox proportional hazard analysis included relapse treatment response (CR vs CRi vs CRp), MRD status at the time of relapse response, and HCT status, and demonstrated that MRD status at relapse response (p=0.002) and HCT (p<0.001) were independent predictors of RFS after first relapse. Type of salvage therapy response (CR vs CRi vs CRp) did not impact OS (p=0.17) or RFS (p=0.16) in multivariable analysis. Only HCT status was an independent predictor of better OS in multivariable analysis (p=0.006).
Conclusion: In adult ALL pts who achieved CR2, CG risk at the time of relapse does not affect long-term survival. MRD positivity at the time of relapse response is an independent predictor of worse RFS, and it is associated with CRi. Ability to get to a successful HCT is the only independent predictor of longer RFS and OS at the time of CR2.
Sekeres:Celgene: Membership on an entity's Board of Directors or advisory committees; Millenium/Takeda: Membership on an entity's Board of Directors or advisory committees. Mukherjee:Novartis: Consultancy, Honoraria, Research Funding; Ariad: Consultancy, Honoraria, Research Funding; Celgene: Consultancy, Honoraria, Research Funding. Carraway:Novartis: Membership on an entity's Board of Directors or advisory committees; Amgen: Membership on an entity's Board of Directors or advisory committees; Celgene: Research Funding, Speakers Bureau; Baxalta: Speakers Bureau; Incyte: Membership on an entity's Board of Directors or advisory committees. Advani:Pfizer Inc.: Consultancy, Research Funding; Blinatumomab: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal