Abstract
Introduction: Proinflammatory cytokines/chemokines have been implicated in the pathogenesis and prognosis of myeloproliferative neoplasms (MPNs) and myelodysplastic syndromes (MDS). Augmenting cytokine levels by JAK2 inhibition or cytokine neutralization are promising therapeutic approaches in these diseases. Chronic Myelomonocytic Leukemia (CMML) is a myeloid neoplasm that has both features of MDS and MPNs for which JAK2 inhibition has yielded reductions in inflammatory cytokines and promising clinical activity. Therefore, we hypothesize that annotation of inflammatory cytokines may uncover cytokine subsets associated with CMML-specific clinical features and identify novel therapeutic targets. To address this, we perform the first comprehensive annotation of inflammatory cytokines in CMML.
Methods: A custom 46-plex Luminex based inflammatory cytokine profiling assay was developed. Cryopreserved peripheral blood plasma was collected from three academic centers after institutional review board approval. Center specific, age-matched plasma controls processed in a similar manner to CMML plasma samples were collected for analytical comparison. All samples were profiled in duplicate and only cytokines above the range of negative controls were reported. CMML cases were also clinically annotated by retrospective chart review and genotyping performed to annotate the frequency of TET2, IDH1/2, DNMT3A, ASXL1, EZH2, SRSF2, SF3B1, U2AF1, ZRSR2, N/K-RAS, CBL, and JAK2 somatic mutations. Descriptive statistics were used to summarize data and the Mann-Whitney test was used to compare cytokine levels among clinically and genetically relevant groups. A Cox proportional hazards model was used to derive likelihood ratios for overall survival using JMP®, Version 12. SAS Institute Inc., Cary, NC.
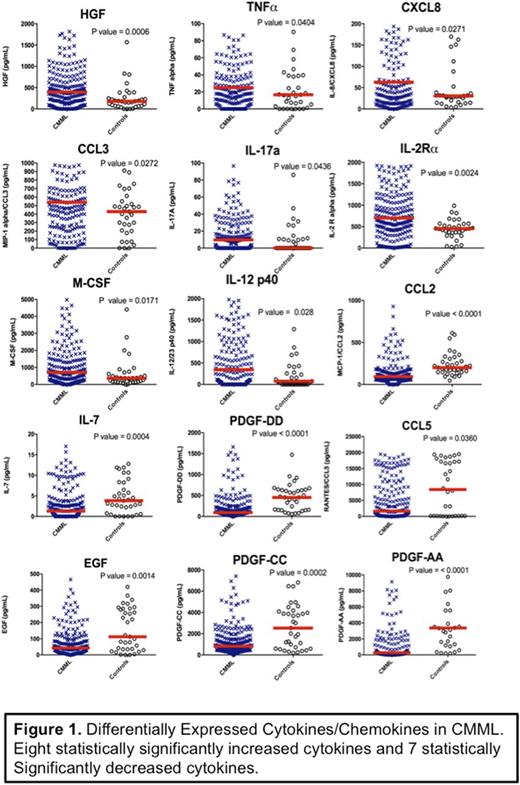
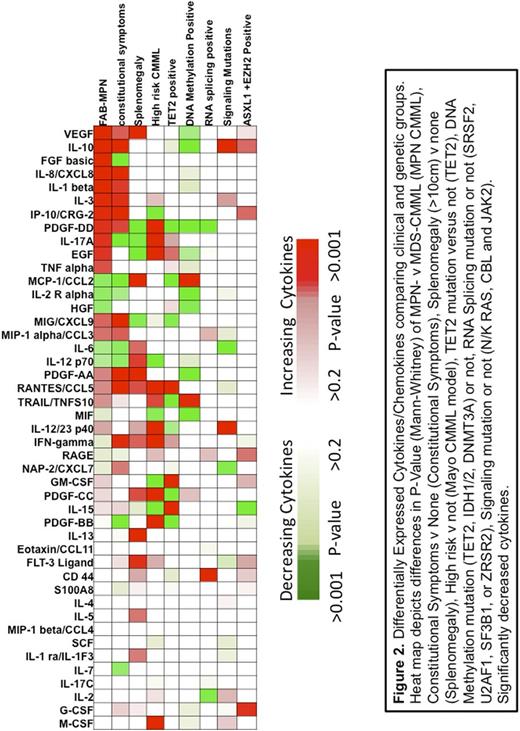
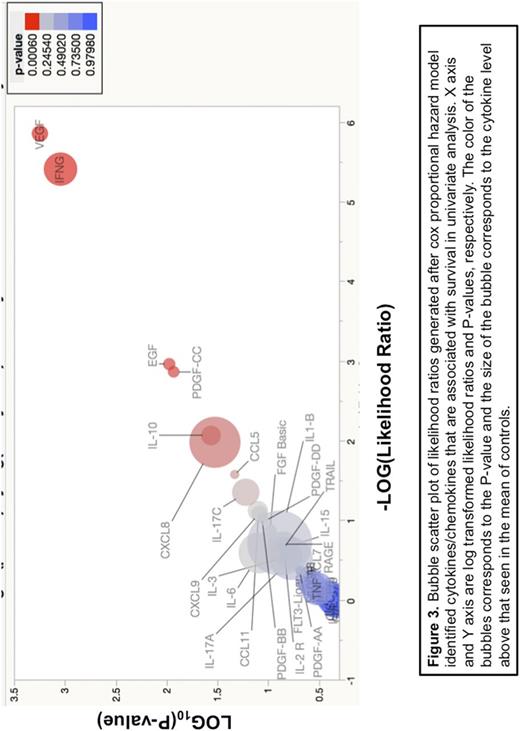
Results: A total of 219 CMML and 35 control plasma samples were profiled. The median age was 73.4 years and 67.1 years in CMML and healthy controls, respectively. Eighty seven percent were CMML-1 by the WHO criteria and 54% were MPN-CMML by FAB criteria. Significantly different levels of cytokines between CMML and controls are summarized in Figure 1 and included TNFa (P=0.0404), IL-8 (P=0.0271), MCP-1 (P<0.0001), IL-1RA (P=0.0174), MIP-1a (P =0.0272), IL-17A (P= 0.0174), HGF (P =0.0006), and IL-12 (P=0.0287). Next, we analyzed differences in cytokine levels among clinically distinct groups to include proliferative versus dysplastic CMML patients reasoning that inflammatory cytokines are likely associated with this clinical phenotype. Indeed, patients with MPN-CMML and those with constitutional symptoms had increased levels of VEGF (P=0.0001), IL-10 (P=0.0002), IL-8 (P=0.0031), IL-1β (p=0.004), and other cytokines summarized in Figure 2 consistent with their clinical symptomatology. Last, we performed a genotype cytokine analysis and identified mutation-specific CMML cytokine signatures summarized in Figure 2. For example, patients with TET2 mutations were found to have significantly increased IFNγ (P=0.0470), GM-CSF (0.0020), and CD44 (P=0.058) while splicing mutations had significantly increased levels of MIP-1a (P=0.049), IL-2 (P=0.017), and CD44 (P=0.0039). To explore whether cytokines can independently influence prognosis, we used a cox proportional hazard model to calculate likelihood ratios of cytokines and overall survival. In univariate analysis, we identified VEGF (P=0.0006), IFNγ (P=0.001), EGF (P=0.0148), PDGF-CC (P=0.0165), and IL-10 (P=0.046) as prognostic in CMML (Figure 3). We next adjusted for age, hemoglobin, FAB and WHO subtype and demonstrate that only CXCL8 (p=0.016), PDGF-CC (P=0.010), and IL-10 (p=0.003) were independently prognostic.
Conclusions: CMML is characterized by specific cytokine signatures that are associated with clinical disease behavior and somatic mutations. IL-8/CXCL8 was the only cytokine/chemokine in our analysis that was statistically elevated, associated with proliferative features, and independently prognostic suggesting a critical role in CMML pathogenesis. The therapeutic candidacy of augmenting differentially expressed cytokines will be the subject of future investigation.
Komrokji:Novartis: Consultancy, Speakers Bureau; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding. Santini:Novartis: Consultancy, Honoraria; Amgen: Other: advisory board; Astex: Other: advisory board; Celgene: Consultancy, Honoraria, Research Funding; Onconova: Other: advisory board; Janssen: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal