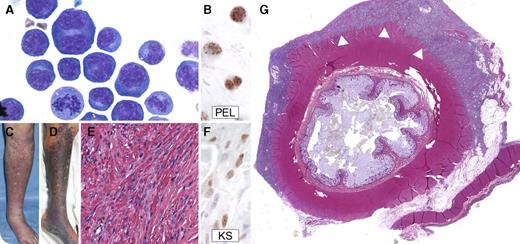
A 59-year-old man was diagnosed with HIV and Kaposi sarcoma (KS) 8 years prior to death; CD4+ count at diagnosis was 538 cells per μL. Despite antiretroviral therapy, KS required several additional therapies. More than 7 years later, the patient developed fever, rapidly progressive KS, effusions, and anasarca. Hemoglobin was 7.8 g/dL; albumin, 2.1 g/dL; and C-reactive protein, >300 mg/L. He met clinical criteria for KS-associated herpesvirus (KSHV)–associated inflammatory cytokine syndrome (KICS). Serum interleukin-6 (IL-6) was 26.2 pg/mL (1 year earlier, IL-6 was 1.4 pg/mL). Effusion cytology showed anaplastic cells with plasmacytoid cytoplasm, Reed-Sternberg–like cells, mitoses (panel A, magnification ×100), and immunopositivity for KSHV latency-associated nuclear antigen (LANA-1) (panel B, magnification ×100), diagnostic of primary effusion lymphoma (PEL).
Despite therapy, he died 2 months later. Immediately prior to death, IL-6 was 430 pg/mL. Compared with KS at PEL diagnosis (panel C), increased violaceous plaques covered extremities (panel D). At autopsy, classic KS pathologic features were noted, including atypical spindle cells in a fascicular growth pattern, extravasated erythrocytes (panel E, magnification ×40), and LANA-1 immunopositivity (panel F, magnification ×100). Diffuse lymphomatous plaques were noted on the pericardial, pleural, and peritoneal serosae, exemplified by PEL sheeting the colon (panel G, magnification ×0.4, arrowheads). Patients with well-controlled HIV remain at an elevated risk of developing KSHV-associated malignancies. PEL and progressive KS may be associated with an IL-6-related KICS.
A 59-year-old man was diagnosed with HIV and Kaposi sarcoma (KS) 8 years prior to death; CD4+ count at diagnosis was 538 cells per μL. Despite antiretroviral therapy, KS required several additional therapies. More than 7 years later, the patient developed fever, rapidly progressive KS, effusions, and anasarca. Hemoglobin was 7.8 g/dL; albumin, 2.1 g/dL; and C-reactive protein, >300 mg/L. He met clinical criteria for KS-associated herpesvirus (KSHV)–associated inflammatory cytokine syndrome (KICS). Serum interleukin-6 (IL-6) was 26.2 pg/mL (1 year earlier, IL-6 was 1.4 pg/mL). Effusion cytology showed anaplastic cells with plasmacytoid cytoplasm, Reed-Sternberg–like cells, mitoses (panel A, magnification ×100), and immunopositivity for KSHV latency-associated nuclear antigen (LANA-1) (panel B, magnification ×100), diagnostic of primary effusion lymphoma (PEL).
Despite therapy, he died 2 months later. Immediately prior to death, IL-6 was 430 pg/mL. Compared with KS at PEL diagnosis (panel C), increased violaceous plaques covered extremities (panel D). At autopsy, classic KS pathologic features were noted, including atypical spindle cells in a fascicular growth pattern, extravasated erythrocytes (panel E, magnification ×40), and LANA-1 immunopositivity (panel F, magnification ×100). Diffuse lymphomatous plaques were noted on the pericardial, pleural, and peritoneal serosae, exemplified by PEL sheeting the colon (panel G, magnification ×0.4, arrowheads). Patients with well-controlled HIV remain at an elevated risk of developing KSHV-associated malignancies. PEL and progressive KS may be associated with an IL-6-related KICS.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal