In this issue of Blood, Kozloski et al identify microRNA (miR)-181a as a novel negative regulator of nuclear factor-κB (NF-κB) signaling in the activated B-cell (ABC)-like subtype of diffuse large B-cell lymphoma (DLBCL).1
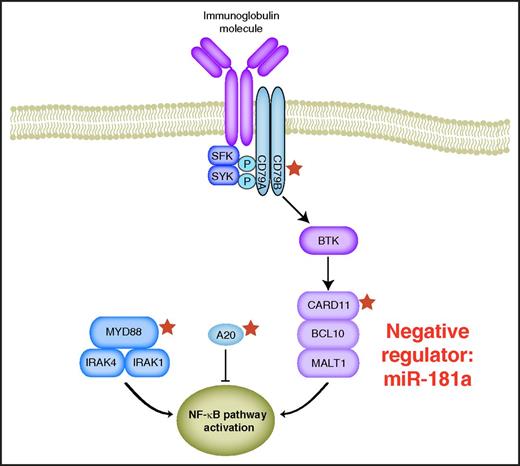
Molecular mechanisms that regulate NF-κB signaling in ABC DLBCL. Stars indicate genes that are targeted by recurrent mutations.
Molecular mechanisms that regulate NF-κB signaling in ABC DLBCL. Stars indicate genes that are targeted by recurrent mutations.
DLBCL represents the most frequent malignant lymphoma subtype that is characterized by striking heterogeneity with respect to biology, clinical presentation, and prognosis.2 Patients with ABC DLBCL are associated with adverse survival following standard therapy with rituximab and cyclophosphamide, doxorubicin, vincristine, and prednisone chemotherapy, indicating that novel therapeutic strategies are urgently warranted.3 Thus, a better understanding of the biology of the molecular DLBCL subtypes is critical to incorporate novel targeted agents in a reasonable manner. ABC DLBCLs are addicted to constitutive NF-κB signaling. This dependency is frequently caused by recurrent, somatically acquired mutations affecting both positive (caspase recruitment domain family member 11 [CARD11], CD79B, and myeloid differentiation primary response 88 [MYD88]) and negative NF-κB regulators (tumor necrosis factor α–induced protein 3 [TNFAIP3; A20]).4-8 Preliminary clinical data from a recently published phase 1/2 study in relapsed or refractory DLBCL patients suggested that inhibition of B-cell receptor (BCR)-mediated NF-κB signaling using the Bruton tyrosine kinase (BTK) inhibitor ibrutinib is preferentially active in ABC DLBCL, as roughly 40% of these patients responded to an ibrutinib monotherapy.9 Collectively, these data implicate that the NF-κB signaling pathway plays an important role in the molecular pathogenesis of ABC DLBCL.
In this issue, Kozloski et al report that miR-181a acts as a negative regulator of NF-κB signaling. miRs are short noncoding RNA molecules that regulate gene expression at the translational level. Interestingly, miR-181a is significantly lower expressed in ABC compared with germinal center B-cell–like DLBCLs. BCR stimulation leads to downregulation of miR-181a expression. Different miR-181a overexpression studies as well as knockdown experiments of miR-181a in DLBCL cell line models suggested that various regulators of NF-κB signaling such as CARD11, NFKBIA, or REL are directly regulated by miR-181a. Additional experiments showed that miR-181a represses NF-κB activity irrespective of the presence of activating pathway mutations, indicating that miR-181a represents a novel negative regulator of NF-κB signaling in ABC DLBCL.
Another major finding revealed by this study was that expression of miR-181a decreased proliferation and induced cytotoxicity especially in in vitro models of ABC DLBCL. These results were confirmed in vivo in ABC DLBCL xenograft mouse models, as miR-181a expression resulted in significantly slower lymphoma growth and prolonged survival.
Collectively, the study by Kozloski et al provides important novel insights into the control of oncogenic NF-κB signaling in ABC DLBCL. It is evident from this study that miR-181a plays an important role in regulating NF-κB signaling (see figure). NF-κB pathway activation seems to be the pathogenetic hallmark of ABC DLBCL biology and various molecular mechanisms have been identified that drive this constitutive signaling (see figure). However, as indicated in a recently published phase 1/2 study, various ABC lymphomas lack known mutations in NF-κB regulators, indicating that other molecular mechanisms regulate its constitutive activity.9 It is tempting to speculate whether miR-181a might be involved in the regulation of NF-κB signaling in these tumors.
Further studies are required to fully unravel the role of miR-181a in the molecular pathogenesis of ABC DLBCL. Currently, the molecular mechanisms suppressing miR-181a expression are not fully elucidated. Furthermore, it is unknown whether expression of miR-181a is reduced throughout all ABC DLBCL tumors or whether expression could vary within this category of DLBCLs. Finally, it would be of great interest to investigate whether miR-181a is involved in the biology of other NF-κB–dependent lymphomas.
Conflict-of-interest disclosure: The author declares no competing financial interests.