Key Points
Dexamethasone vs prednisone in induction of pediatric ALL led to significant relapse reduction and increased treatment-related mortality.
No overall survival benefit was achieved with dexamethasone except in the subset of patients with T-cell ALL and good early treatment response.
Abstract
Induction therapy for childhood acute lymphoblastic leukemia (ALL) traditionally includes prednisone; yet, dexamethasone may have higher antileukemic potency, leading to fewer relapses and improved survival. After a 7-day prednisone prephase, 3720 patients enrolled on trial Associazione Italiana di Ematologia e Oncologia Pediatrica and Berlin-Frankfurt-Münster (AIEOP-BFM) ALL 2000 were randomly selected to receive either dexamethasone (10 mg/m2 per day) or prednisone (60 mg/m2 per day) for 3 weeks plus tapering in induction. The 5-year cumulative incidence of relapse (± standard error) was 10.8 ± 0.7% in the dexamethasone and 15.6 ± 0.8% in the prednisone group (P < .0001), showing the largest effect on extramedullary relapses. The benefit of dexamethasone was partially counterbalanced by a significantly higher induction-related death rate (2.5% vs 0.9%, P = .00013), resulting in 5-year event-free survival rates of 83.9 ± 0.9% for dexamethasone and 80.8 ± 0.9% for prednisone (P = .024). No difference was seen in 5-year overall survival (OS) in the total cohort (dexamethasone, 90.3 ± 0.7%; prednisone, 90.5 ± 0.7%). Retrospective analyses of predefined subgroups revealed a significant survival benefit from dexamethasone only for patients with T-cell ALL and good response to the prednisone prephase (prednisone good-response [PGR]) (dexamethasone, 91.4 ± 2.4%; prednisone, 82.6 ± 3.2%; P = .036). In patients with precursor B-cell ALL and PGR, survival after relapse was found to be significantly worse if patients were previously assigned to the dexamethasone arm. We conclude that, for patients with PGR in the large subgroup of precursor B-cell ALL, dexamethasone especially reduced the incidence of better salvageable relapses, resulting in inferior survival after relapse. This explains the lack of benefit from dexamethasone in overall survival that we observed in the total cohort except in the subset of T-cell ALL patients with PGR. This trial was registered at www.clinicaltrials.gov (BFM: NCT00430118, AIEOP: NCT00613457).
Introduction
Since the early era of treating patients with acute lymphoblastic leukemia (ALL), glucocorticoids have been an essential component of therapy regimens.1,2 Traditionally, prednisone has been the most commonly used glucocorticoid in remission induction, whereas dexamethasone has been applied during the reintensification phase.
Dexamethasone has a six- to sevenfold higher efficacy than prednisone in terms of antiinflammatory effects,3 which traditionally led to dexamethasone/prednisone equivalent dosages of 1:6 to 1:7. Data on the relative antileukemic potency of dexamethasone and prednisone in vitro suggest an ∼16-fold higher median cytotoxic potency of dexamethasone, although with a large interindividual variability.4 In vitro cytotoxicity assays using stroma-supported cultures of ALL blasts indicated a five- to sixfold higher cytotoxic potency of dexamethasone.5
Additional factors may contribute to a greater efficacy of dexamethasone in vivo, namely a longer plasma half-life and a lower protein-bound fraction in combination with a longer half-life in the cerebral spinal fluid (CSF), leading to better CSF penetration and higher CSF concentrations.6 Accordingly, some early clinical trials reported superior outcome using dexamethasone instead of prednisone during induction treatment, in particular because of a reduced rate of relapses in the central nervous system (CNS).7,8
These data provided the rationale for a randomized question that was implemented in the collaborative clinical trial AIEOP-BFM ALL 2000 conducted by the Associazione Italiana di Ematologia e Oncologia Pediatrica (AIEOP) and Berlin-Frankfurt-Münster (BFM) ALL study groups between 2000 and 2006. Results of this trial regarding the prognostic impact of minimal residual disease (MRD) have already been reported.9,10 Here, we report on the results of a randomization during the induction phase to test the hypothesis that treatment with dexamethasone instead of prednisone provides a better event-free survival (EFS) and overall survival (OS) in childhood ALL.
Patients and methods
Patients and study design
Children and adolescent patients from the ages of 1 to 17 years were diagnosed with ALL in one of the 127 participating study centers in Austria, Germany, Italy, and Switzerland (details are provided in the supplemental Appendix, available on the Blood Web site) and registered in the AIEOP-BFM ALL 2000 randomized trial after obtaining written informed consent from their guardians.
Diagnostic studies included cytomorphology, immunophenotyping, molecular genetic screening for the presence of ETV6-RUNX1, BCR-ABL, and MLL-AF4 fusion transcripts, early cytomorphologic response assessment, and quantitative assessment of MRD based on immunoglobulin and T-cell receptor gene rearrangements. Tests were performed according to standard procedures as published before.9-14 Prednisone good-response and poor-response were defined as <1.0 × 109/L or ≥1.0 × 109/L blasts in blood, respectively, after a 7-day prednisone prephase and one intrathecal dose of methotrexate.14 Complete remission (CR) was defined as <5% blasts in the regenerating bone marrow and absence of extramedullary disease. Nonresponse was defined as not having achieved CR after the third pulsatile high-dose block. Relapse was defined as recurrence of ≥25% lymphoblasts in bone marrow or localized leukemic infiltrate at any site.
Risk group assignment was based on cytologic and molecular response to treatment and on genetic features of ALL blasts. Patients with at least one of these listed criteria—prednisone poor-response, no CR on day 33, evidence of t(9;22) (or BCR-ABL), evidence of t(4;11) (or MLL-AF4), or MRD load of 5 × 10−4 or more on day 78 (MRD-HR)—were allocated to the high-risk group (HR). In the absence of high-risk criteria, patients were assigned to the medium-risk group (MR) if they had positive MRD on day 33 and/or day 78 but at a level of <5 × 10−4 on day 78 (MRD-MR), or were not classifiable by MRD. If MRD was negative on day 33 and day 78 with at least 2 markers with a sensitivity of 10−4 or better (MRD-SR), patients were allocated to the standard-risk group (SR).
The study protocol was approved by the competent ethics committees of the national coordinating centers (Hannover Medical School, Hannover; St. Anna Children’s Hospital, Vienna; University Children's Hospital, Zürich; S. Gerardo Hospital, Monza).
Randomization and treatment
In this open-label study, patients were randomly assigned to receive the standard glucocorticoid therapy with prednisone or the experimental therapy with dexamethasone as part of the 4-drug induction therapy phase Protocol IA. Randomization was performed by day 8 in a 1:1 ratio. It used permuted blocks of 4 patients and was stratified by country and in Italy and Germany in addition by center. All patients started therapy with a 7-day prephase with prednisone and one intrathecal dose of methotrexate. After the prednisone prephase, glucocorticoid therapy was continued according to the randomization arm with either prednisone (60 mg/m2 per day) or dexamethasone (10 mg/m2 per day) for an additional 21 days with subsequent tapering over 9 days.
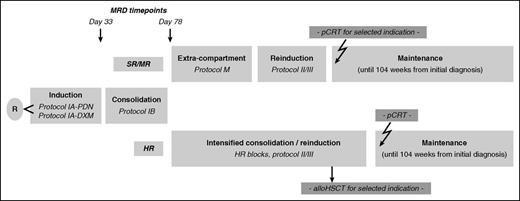
The treatment outline is provided in Figure 1. Criteria for eligibility for allogeneic stem cell transplantation and cranial irradiation are shown in supplemental Tables 1 and 2 in the supplemental Appendix. Full treatment details and drug doses were published earlier9,10 and are also listed in supplemental Table 3 in the supplemental Appendix.
Treatment outline of AIEOP-BFM ALL 2000. alloHSCT, allogeneic hematopoietic stem cell transplantation; pCRT, preventive cranial radiotherapy; Protocol IA-PDN, Protocol IA with prednisone; Protocol IA-DXM, Protocol IA with dexamethasone; R, randomization.
Treatment outline of AIEOP-BFM ALL 2000. alloHSCT, allogeneic hematopoietic stem cell transplantation; pCRT, preventive cranial radiotherapy; Protocol IA-PDN, Protocol IA with prednisone; Protocol IA-DXM, Protocol IA with dexamethasone; R, randomization.
Outcomes
The primary outcome in this study was event-free survival. Event-free survival was defined as the time from diagnosis to the date of last follow-up or first event. Events were nonresponse, relapse, secondary neoplasm, or death from any cause. Failure to achieve remission as a result of early death or nonresponse was considered as event at time zero. Secondary outcomes were overall survival, short- and long-term toxicity, treatment-related death in induction or in remission, and MRD levels at end of induction and after consolidation. Overall survival was defined as the time from diagnosis to death from any cause or last follow-up.
Statistical analysis
Analyses were performed by randomization arm (intent-to-treat), except the analyses of treatment-related toxicity, which were done as “as-treated” analysis. The Kaplan-Meier method was used to estimate survival rates; differences between groups were compared with the log-rank test. Cumulative incidence functions for competing events were constructed by the method of Kalbfleisch and Prentice and were compared with the Gray test.15 The Cox proportional hazard model was used for uni- and multivariate analyses. Those risk factors for survival after relapse that were significant in univariate analysis (tested: gender, age at relapse [< vs ≥10 years], white blood count [WBC] at diagnosis [< vs ≥100 × 109/L], MRD at end of induction [negative vs positive] and on day 78 [< vs ≥ 5 × 10−4], relapse risk group [S1/S2 vs S3/S416 ], and ETV6-RUNX1 status) were included in the multivariate analysis of survival after relapse. Differences in the distribution of categorical variables were analyzed using the Fisher exact test.
The sample size for randomization of induction treatment was calculated in the light of the estimations for the primary endpoint (ie, event-free survival). According to the results of preceding studies, the probability of 4-year event-free survival of patients treated with prednisone was estimated to be 75%. To detect an increase of 5%, 2948 patients were required to be randomly placed (2-sided α = .05, power 90%). On the basis of the previous trial, we would have expected an overall survival of 84% and 87% for the prednisone and dexamethasone arms, respectively. The study was not powered to detect the expected survival difference of 3%.
A Data Safety and Monitoring Committee periodically supervised the study progress. In view of safety concerns, the Committee suggested in October 2004 halting the randomization for patients aged 10 years or older.
The trial was registered at www.clinicaltrials.gov with registration numbers NCT00430118 for BFM and NCT00613457 for AIEOP.
Patient data were updated in January 2014 with a median follow-up of 8.8 years.
Results
Patient characteristics
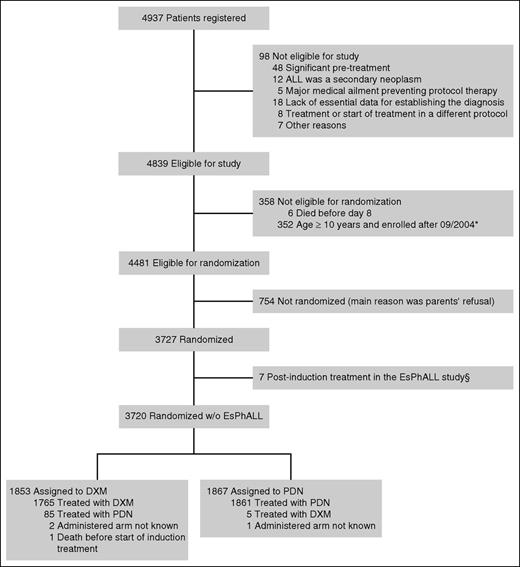
Of 4937 patients who were registered in the AIEOP-BFM ALL 2000 trial from July 1, 2000 to July 31, 2006, 98 were not eligible for evaluation (for details, see Figure 217 ). Of the remaining 4839 eligible patients, 358 patients were not eligible for the randomization either because they died in the first week of therapy or because of age ≥10 years (which was an exclusion criterion after the amendment from October 2004), resulting in 4481 patients being eligible for randomization. Of these patients, 754 (16.8%) were not randomized mainly because of parents’ refusal, and an additional 7 patients (0.2%) with translocation t(9;22) were transferred to the EsPhALL trial (European Intergroup Study on Post-induction Treatment of Philadelphia Chromosome-positive ALL) after induction treatment and were therefore excluded from the analysis. Of the remaining 3720 patients randomly placed, 1853 were assigned to the dexamethasone arm and 1867 patients to the prednisone arm (Figure 2).
Consolidated Standards for Reporting of Trials (CONSORT) diagram.*Stop of randomization for patients ≥10 years of age in October 2004. §Seven randomized patients with Ph+ ALL dropped out of the study after induction treatment because of participation in the EsPhALL trial for postinduction treatment of Ph+ ALL, which has been open from 2004 onward.17 Patient characteristics of randomized and eligible nonrandomized patients are presented in supplemental Table 4.
Consolidated Standards for Reporting of Trials (CONSORT) diagram.*Stop of randomization for patients ≥10 years of age in October 2004. §Seven randomized patients with Ph+ ALL dropped out of the study after induction treatment because of participation in the EsPhALL trial for postinduction treatment of Ph+ ALL, which has been open from 2004 onward.17 Patient characteristics of randomized and eligible nonrandomized patients are presented in supplemental Table 4.
Initial patient characteristics were equally distributed between the 2 randomization groups (Table 1). There were minor differences that reached statistical significance between eligible patients who did or did not undergo randomization with regard to positivity for ETV6-RUNX1, National Cancer Institute (NCI) risk groups within B-lineage ALL patients, and age groups (supplemental Table 4 of the supplemental Appendix).
Initial patient characteristics
| . | Dexamethasone* . | Prednisone* . |
|---|---|---|
| N (%) . | N (%) . | |
| Sex | ||
| Female | 803 (43.3) | 864 (46.3) |
| Male | 1050 (56.7) | 1003 (53.7) |
| Age (y) | ||
| ≥1 to <6 | 1147 (61.9) | 1127 (60.4) |
| ≥6 to <10 | 376 (20.3) | 402 (21.5) |
| ≥10 to <15 | 262 (14.1) | 252 (13.5) |
| ≥15 | 68 (3.7) | 86 (4.6) |
| Initial WBC (× 109/L) | ||
| <20 | 1200 (64.8) | 1182 (63.3) |
| 20 to <100 | 477 (25.7) | 505 (27.1) |
| ≥100 | 176 (9.5) | 180 (9.6) |
| CNS status | ||
| CNS negative | 1770 (97.5) | 1766 (97.1) |
| CNS positive | 46 (2.5) | 53 (2.9) |
| Immunophenotype | ||
| Precursor B | 1604 (87.8) | 1619 (88.3) |
| T | 220 (12.0) | 212 (11.6) |
| Other† | 2 (0.1) | 4 (0.2) |
| ETV6-RUNX1 | ||
| Positive | 405 (24.1) | 392 (22.8) |
| Negative | 1276 (75.9) | 1331 (77.2) |
| BCR-ABL | ||
| Positive | 35 (2.0) | 30 (1.7) |
| Negative | 1743 (98.0) | 1781 (98.3) |
| MLL-AF4 | ||
| Positive | 7 (0.4) | 13 (0.7) |
| Negative | 1718 (99.6) | 1747 (99.3) |
| DNA index | ||
| <1.16 | 1153 (81.1) | 1150 (80.8) |
| ≥1.16 | 268 (18.9) | 273 (19.2) |
| B-lineage NCI Risk criteria‡ | ||
| Standard risk | 1159 (72.3) | 1178 (72.8) |
| High risk | 445 (27.7) | 441 (27.2) |
| T-lineage NCI Risk criteria‡ | ||
| Standard risk | 61 (27.7) | 51 (24.1) |
| High risk | 159 (72.3) | 161 (75.9) |
| . | Dexamethasone* . | Prednisone* . |
|---|---|---|
| N (%) . | N (%) . | |
| Sex | ||
| Female | 803 (43.3) | 864 (46.3) |
| Male | 1050 (56.7) | 1003 (53.7) |
| Age (y) | ||
| ≥1 to <6 | 1147 (61.9) | 1127 (60.4) |
| ≥6 to <10 | 376 (20.3) | 402 (21.5) |
| ≥10 to <15 | 262 (14.1) | 252 (13.5) |
| ≥15 | 68 (3.7) | 86 (4.6) |
| Initial WBC (× 109/L) | ||
| <20 | 1200 (64.8) | 1182 (63.3) |
| 20 to <100 | 477 (25.7) | 505 (27.1) |
| ≥100 | 176 (9.5) | 180 (9.6) |
| CNS status | ||
| CNS negative | 1770 (97.5) | 1766 (97.1) |
| CNS positive | 46 (2.5) | 53 (2.9) |
| Immunophenotype | ||
| Precursor B | 1604 (87.8) | 1619 (88.3) |
| T | 220 (12.0) | 212 (11.6) |
| Other† | 2 (0.1) | 4 (0.2) |
| ETV6-RUNX1 | ||
| Positive | 405 (24.1) | 392 (22.8) |
| Negative | 1276 (75.9) | 1331 (77.2) |
| BCR-ABL | ||
| Positive | 35 (2.0) | 30 (1.7) |
| Negative | 1743 (98.0) | 1781 (98.3) |
| MLL-AF4 | ||
| Positive | 7 (0.4) | 13 (0.7) |
| Negative | 1718 (99.6) | 1747 (99.3) |
| DNA index | ||
| <1.16 | 1153 (81.1) | 1150 (80.8) |
| ≥1.16 | 268 (18.9) | 273 (19.2) |
| B-lineage NCI Risk criteria‡ | ||
| Standard risk | 1159 (72.3) | 1178 (72.8) |
| High risk | 445 (27.7) | 441 (27.2) |
| T-lineage NCI Risk criteria‡ | ||
| Standard risk | 61 (27.7) | 51 (24.1) |
| High risk | 159 (72.3) | 161 (75.9) |
Data refer to patients with successful investigation of the respective criteria.
Mature B-cell leukemia, cytomorphologically FAB L1 (n = 3), natural killer cell leukemia (n = 1), acute undifferentiated leukemia (n = 1).
NCI-SR, age ≥1 and <10 y and WBC <50 × 109/L; NCI-HR, age ≥10 y or WBC ≥50 × 109/L.
Treatment outcome
The proportion of patients who did not reach CR on day 33 was similar in the 2 randomization groups (Table 2). In pB-ALL patients, a more rapid MRD response with a significant shift to lower MRD results on day 33 could be shown in the dexamethasone group; the difference was no longer obvious on day 78. In T-cell ALL (T-ALL), there was also a shift of ∼5 to 6% of the patients toward lower MRD levels in the dexamethasone arm, which was apparent on day 33 and day 78, but was not statistically significant (Table 2).
Response parameters
| . | Dexamethasone* . | Prednisone* . | P . |
|---|---|---|---|
| N (%) . | N (%) . | ||
| pB-ALL prednisone response | |||
| Good | 1494 (93.5) | 1511 (93.6) | .94 |
| Poor | 104 (6.5) | 104 (6.4) | |
| T-ALL prednisone response | |||
| Good | 140 (66.7) | 140 (66.4) | .92 |
| Poor | 74 (33.3) | 71 (33.6) | |
| Remission d33 | |||
| Remission d33 | 1777 (97.8) | 1812 (97.8) | 1.00 |
| No remission d33 | 40 (2.2) | 40 (2.2) | |
| pB-ALL MRD day 33† | |||
| Negative | 580 (47.1) | 565 (43.7) | .00057 |
| Positive <5 × 10−4 | 439 (35.7) | 426 (32.9) | |
| Positive ≥5 × 10−4 | 212 (17.2) | 303 (23.4) | |
| pB-ALL MRD day 78† | |||
| Negative | 970 (78.8) | 1002 (77.3) | .36 |
| Positive <5 × 10−4 | 194 (15.7) | 207 (16.0) | |
| Positive ≥5 × 10−4 | 67 (5.4) | 88 (6.8) | |
| T-ALL MRD day 33† | |||
| Negative | 29 (18.8) | 22 (13.8) | .43 |
| Positive <5 × 10−4 | 41 (26.6) | 41 (25.8) | |
| Positive ≥5 × 10−4 | 84 (54.5) | 96 (60.4) | |
| T-ALL MRD day 78† | |||
| Negative | 78 (50.3) | 70 (43.8) | .43 |
| Positive <5 × 10−4 | 48 (31.0) | 52 (32.5) | |
| Positive ≥5 × 10−4 | 29 (18.7) | 38 (23.8) | |
| MRD risk group† | |||
| MRD-SR | 597 (42.3) | 584 (39.4) | .11 |
| MRD-MR | 717 (50.9) | 771 (52.1) | |
| MRD-HR | 96 (6.8) | 126 (8.5) | |
| Final risk group | |||
| SR-2000 | 577 (31.1) | 561 (30.0) | .77 |
| MR-2000 | 1001 (54.0) | 1026 (55.0) | |
| HR-2000 | 275 (14.8) | 280 (15.0) |
| . | Dexamethasone* . | Prednisone* . | P . |
|---|---|---|---|
| N (%) . | N (%) . | ||
| pB-ALL prednisone response | |||
| Good | 1494 (93.5) | 1511 (93.6) | .94 |
| Poor | 104 (6.5) | 104 (6.4) | |
| T-ALL prednisone response | |||
| Good | 140 (66.7) | 140 (66.4) | .92 |
| Poor | 74 (33.3) | 71 (33.6) | |
| Remission d33 | |||
| Remission d33 | 1777 (97.8) | 1812 (97.8) | 1.00 |
| No remission d33 | 40 (2.2) | 40 (2.2) | |
| pB-ALL MRD day 33† | |||
| Negative | 580 (47.1) | 565 (43.7) | .00057 |
| Positive <5 × 10−4 | 439 (35.7) | 426 (32.9) | |
| Positive ≥5 × 10−4 | 212 (17.2) | 303 (23.4) | |
| pB-ALL MRD day 78† | |||
| Negative | 970 (78.8) | 1002 (77.3) | .36 |
| Positive <5 × 10−4 | 194 (15.7) | 207 (16.0) | |
| Positive ≥5 × 10−4 | 67 (5.4) | 88 (6.8) | |
| T-ALL MRD day 33† | |||
| Negative | 29 (18.8) | 22 (13.8) | .43 |
| Positive <5 × 10−4 | 41 (26.6) | 41 (25.8) | |
| Positive ≥5 × 10−4 | 84 (54.5) | 96 (60.4) | |
| T-ALL MRD day 78† | |||
| Negative | 78 (50.3) | 70 (43.8) | .43 |
| Positive <5 × 10−4 | 48 (31.0) | 52 (32.5) | |
| Positive ≥5 × 10−4 | 29 (18.7) | 38 (23.8) | |
| MRD risk group† | |||
| MRD-SR | 597 (42.3) | 584 (39.4) | .11 |
| MRD-MR | 717 (50.9) | 771 (52.1) | |
| MRD-HR | 96 (6.8) | 126 (8.5) | |
| Final risk group | |||
| SR-2000 | 577 (31.1) | 561 (30.0) | .77 |
| MR-2000 | 1001 (54.0) | 1026 (55.0) | |
| HR-2000 | 275 (14.8) | 280 (15.0) |
Data refer to patients with successful investigation of the respective criteria.
MRD data are shown for patients who could successfully be classified by MRD according to the protocol criteria.
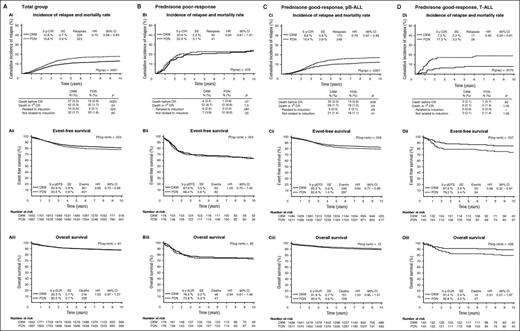
Events are shown in Table 3. The overall relapse incidence was reduced by one third in the dexamethasone arm (Figure 3Ai). Relapse reduction was more pronounced for extramedullary relapses than for isolated bone marrow relapses. Death rates before achievement of CR and in first CR related to induction treatment were significantly higher in patients assigned to receive dexamethasone. No difference between the randomization groups was seen with regard to the rate of nonresponse, postinduction deaths, and the incidence of secondary neoplasms. Event-free survival was significantly better for patients randomly assigned to the dexamethasone arm compared with patients assigned to receive prednisone (hazard ratio [HR], 0.85 [0.73-0.98]; Figure 3Aii). No difference between the randomization groups could be demonstrated for overall survival (HR, 1.05 [0.87-1.27]; Figure 3Aiii).
Events
| . | Randomization group as assigned . | . | . | |||
|---|---|---|---|---|---|---|
| . | DXM (n = 1853) . | PDN (n = 1867) . | . | . | ||
| . | N . | %† . | N . | %† . | P§ . | HR (95% CI) . |
| Death before CR | 37 | 2.0 | 15 | 0.8 | .0019 | 2.49 (1.36-4.53) |
| Non-response | 3 | 0.2 | 6 | 0.3 | .51 | 0.50 (0.13-2.02) |
| Death in 1st CR | 42 | 2.3 | 32 | 1.7 | .24 | 1.33 (0.84-2.11) |
| Related to induction chemotherapy | 10 | 0.5 | 2 | 0.1 | .022 | 5.09 (1.1-23.3) |
| Related to post-induction chemotherapy | 17 | 0.9 | 15 | 0.8 | .73 | 1.15 (0.57-2.31) |
| Related to alloHSCT* | 12 | 0.6 | 14 | 0.7 | .84 | 0.87 (0.40-1.87) |
| Other | 3 | 0.2 | 1 | 0.1 | .37 | 2.98 (0.31-28.74) |
| All relapses | 229 | 10.8 (0.7) | 323 | 15.6 (0.8) | <.0001 | 0.70 (0.59-0.83) |
| Isolated BM | 158 | 7.6 (0.6) | 204 | 9.7 (0.7) | .013 | 0.77 (0.62-0.95) |
| Isolated CNS | 19 | 0.9 (0.2) | 37 | 1.9 (0.3) | .019 | 0.51 (0.30-0.90) |
| Isolated testes | 9 | 0.4 (0.1) | 23 | 1.1 (0.2) | .016 | 0.39 (0.18-0.84) |
| Combined CNS/BM involved | 15 | 0.7 (0.2) | 30 | 1.5 (0.3) | .027 | 0.50 (0.27-0.92) |
| Combined BM/other (w/o CNS) | 17 | 0.8 (0.2) | 21 | 1.0 (0.2) | .52 | 0.80 (0.42-1.52) |
| Other relapses | 11 | 0.4 (0.1) | 8 | 0.4 (0.1) | .47 | 1.37 (0.55-3.41) |
| Secondary neoplasms | 30 | 1.0 (0.2) | 25 | 0.8 (0.2) | .47 | 1.18 (0.70-2.01) |
| All events | 341 | 16.1 (0.9) | 401 | 19.2 (0.9) | .024 | 0.85 (0.73-0.98) |
| . | Randomization group as assigned . | . | . | |||
|---|---|---|---|---|---|---|
| . | DXM (n = 1853) . | PDN (n = 1867) . | . | . | ||
| . | N . | %† . | N . | %† . | P§ . | HR (95% CI) . |
| Death before CR | 37 | 2.0 | 15 | 0.8 | .0019 | 2.49 (1.36-4.53) |
| Non-response | 3 | 0.2 | 6 | 0.3 | .51 | 0.50 (0.13-2.02) |
| Death in 1st CR | 42 | 2.3 | 32 | 1.7 | .24 | 1.33 (0.84-2.11) |
| Related to induction chemotherapy | 10 | 0.5 | 2 | 0.1 | .022 | 5.09 (1.1-23.3) |
| Related to post-induction chemotherapy | 17 | 0.9 | 15 | 0.8 | .73 | 1.15 (0.57-2.31) |
| Related to alloHSCT* | 12 | 0.6 | 14 | 0.7 | .84 | 0.87 (0.40-1.87) |
| Other | 3 | 0.2 | 1 | 0.1 | .37 | 2.98 (0.31-28.74) |
| All relapses | 229 | 10.8 (0.7) | 323 | 15.6 (0.8) | <.0001 | 0.70 (0.59-0.83) |
| Isolated BM | 158 | 7.6 (0.6) | 204 | 9.7 (0.7) | .013 | 0.77 (0.62-0.95) |
| Isolated CNS | 19 | 0.9 (0.2) | 37 | 1.9 (0.3) | .019 | 0.51 (0.30-0.90) |
| Isolated testes | 9 | 0.4 (0.1) | 23 | 1.1 (0.2) | .016 | 0.39 (0.18-0.84) |
| Combined CNS/BM involved | 15 | 0.7 (0.2) | 30 | 1.5 (0.3) | .027 | 0.50 (0.27-0.92) |
| Combined BM/other (w/o CNS) | 17 | 0.8 (0.2) | 21 | 1.0 (0.2) | .52 | 0.80 (0.42-1.52) |
| Other relapses | 11 | 0.4 (0.1) | 8 | 0.4 (0.1) | .47 | 1.37 (0.55-3.41) |
| Secondary neoplasms | 30 | 1.0 (0.2) | 25 | 0.8 (0.2) | .47 | 1.18 (0.70-2.01) |
| All events | 341 | 16.1 (0.9) | 401 | 19.2 (0.9) | .024 | 0.85 (0.73-0.98) |
alloHSCT, allogeneic hematopoietic stem cell transplantation; BM, bone marrow; CI, confidence interval; CNS, central nervous system; CR, complete remission; DXM, dexamethasone; HR, hazard ratio; PDN, prednisone.
112 patients in the prednisone and 88 patients in the dexamethasone arm underwent allogeneic stem cell transplantation in first CR.
Percentages are presented for deaths and resistant disease; 5-year cumulative incidences (standard error in parentheses) were calculated for relapses, secondary neoplasms, and the total number of events.
Fisher exact test was used for deaths and resistant disease and Gray test was used for relapses and secondary neoplasms.
Relapse incidence, mortality rate, event-free survival, and overall survival according to the assigned randomization arms. Outcome data are shown for (A) the total cohort, (B) patients with prednisone poor-response, (C) precursor B-ALL with prednisone good-response, and (D) T-ALL with prednisone good-response. Subpanels show (i) the incidence of relapse and mortality rate, (ii) the event-free survival, and (iii) overall survival. Numbers of patients at risk in the event-free survival graphs also apply to the relapse incidence graph. 5 y-CIR, 5-year cumulative incidence of relapse; 5 y-pEFS, 5-year event-free survival; 5 y-pSUR, 5-year overall survival; CI, confidence interval; DXM, dexamethasone; HR hazard ratio; PDN, prednisone SE, standard error.
Relapse incidence, mortality rate, event-free survival, and overall survival according to the assigned randomization arms. Outcome data are shown for (A) the total cohort, (B) patients with prednisone poor-response, (C) precursor B-ALL with prednisone good-response, and (D) T-ALL with prednisone good-response. Subpanels show (i) the incidence of relapse and mortality rate, (ii) the event-free survival, and (iii) overall survival. Numbers of patients at risk in the event-free survival graphs also apply to the relapse incidence graph. 5 y-CIR, 5-year cumulative incidence of relapse; 5 y-pEFS, 5-year event-free survival; 5 y-pSUR, 5-year overall survival; CI, confidence interval; DXM, dexamethasone; HR hazard ratio; PDN, prednisone SE, standard error.
Retrospective analyses were performed for clinical subgroups. Analyzing the patients according to age, the relapse reduction in the dexamethasone arm in patients ≥10 years of age did not translate into a difference in event-free survival between the randomization arms because of the higher incidence of induction-related deaths in the dexamethasone group (supplemental Figure 1B). Patients with prednisone poor-response had comparable relapse incidence, event-free survival, and overall survival in the 2 randomization groups (Figure 3Bi-iii), which was also valid when analyzing B- and T-lineage ALL separately (supplemental Table 5) or stratified by treatment with chemotherapy only or chemotherapy with additional hematopoietic allogeneic stem cell transplantation (data not shown). Among the patients with prednisone good-response, a significantly lower incidence of relapse and better event-free survival could be demonstrated in the dexamethasone arm compared with the prednisone arm for patients with B-lineage (Figure 3Ci-ii) and T-lineage ALL (Figure 3Di-ii). In patients with prednisone good-response and T-ALL, the better event-free survival of the dexamethasone group also translated into significantly better survival (Figure 3Diii). This was in contrast to the patients with prednisone good-response and pB-ALL, who had an even inferior—though statistically insignificant—survival rate in the dexamethasone group (Figure 3Ciii). Excluding the patients ≥10 years of age from this group or including only patients who survived at least 60 days did not significantly change the survival results within this subset (supplemental Figure 1C-D).
Detailed outcome data of further clinical and biological subgroups are presented in supplemental Table 5 of the supplemental Appendix.
Survival after relapse
Survival after relapse was significantly better in the pB-ALL patients with prednisone good-response previously assigned to the prednisone arm compared with the corresponding patients of the dexamethasone arm (5-year probability of survival [5 y-pSUR] after relapse: dexamethasone 51.9%, standard error [SE] 4.1%, n = 173, 81 deaths; prednisone 65.7%, SE 3.1%, n = 248, 85 deaths; P = .0053). Patients with relapsed ALL previously assigned to dexamethasone had a higher proportion of features predicting poor survival after relapse (Table 4). In a multivariate Cox analysis including these factors as covariates, the type of glucocorticoid in induction completely lost its significance (Table 4). Despite the worse risk profile of the relapses in the dexamethasone arm, the proportion of patients who underwent allogeneic stem cell transplantation in second CR was not higher in this group compared with the patients who had relapsed in the prednisone arm (dexamethasone 57.2% [99/173], prednisone 60.9% [151/248]).
Results of the univariate and multivariate Cox regression analyses on survival after relapse in patients with pB-ALL and prednisone good-response according to randomization arm (as assigned) and other characteristics
| . | Relapses by assigned randomization arm . | Survival after relapse . | |||||||
|---|---|---|---|---|---|---|---|---|---|
| . | DXM . | PDN . | . | Univariate analysis . | Multivariate analysis . | ||||
| . | N (%) . | N (%) . | P . | Hazard ratio . | 95% CI . | P . | Hazard ratio . | 95% CI . | P . |
| Randomization arm in frontline treatment | |||||||||
| Prednisone | NA | 248 | 1 | 1 | |||||
| Dexamethasone | 173 | NA | 1.54 | 1.14-2.09 | .0053 | 1.13 | 0.80-1.59 | .50 | |
| Risk group in relapse* | |||||||||
| S1/S2 | 117 (67.6) | 184 (74.2) | 1 | 1 | |||||
| S3/S4 | 56 (32.4) | 64 (25.8) | .14 | 3.65 | 2.69-4.96 | <.0001 | 3.49 | 2.46-4.94 | <.0001 |
| ETV6-RUNX1 | |||||||||
| Positive | 19 (12.7) | 51 (21.8) | 0.40 | 0.23-0.70 | .0012 | 0.44 | 0.24-0.81 | .0077 | |
| Negative | 131 (87.3) | 183 (78.2) | .023 | 1 | 1 | ||||
| MRD on day 78 of frontline treatment | |||||||||
| <5 × 10−4 | 136 (86.6) | 213 (91.8) | 1 | 1 | |||||
| ≥5 × 10−4 | 21 (13.4) | 19 (8.2) | .098 | 4.22 | 2.87-6.21 | <.0001 | 3.00 | 1.98-4.54 | <.0001 |
| . | Relapses by assigned randomization arm . | Survival after relapse . | |||||||
|---|---|---|---|---|---|---|---|---|---|
| . | DXM . | PDN . | . | Univariate analysis . | Multivariate analysis . | ||||
| . | N (%) . | N (%) . | P . | Hazard ratio . | 95% CI . | P . | Hazard ratio . | 95% CI . | P . |
| Randomization arm in frontline treatment | |||||||||
| Prednisone | NA | 248 | 1 | 1 | |||||
| Dexamethasone | 173 | NA | 1.54 | 1.14-2.09 | .0053 | 1.13 | 0.80-1.59 | .50 | |
| Risk group in relapse* | |||||||||
| S1/S2 | 117 (67.6) | 184 (74.2) | 1 | 1 | |||||
| S3/S4 | 56 (32.4) | 64 (25.8) | .14 | 3.65 | 2.69-4.96 | <.0001 | 3.49 | 2.46-4.94 | <.0001 |
| ETV6-RUNX1 | |||||||||
| Positive | 19 (12.7) | 51 (21.8) | 0.40 | 0.23-0.70 | .0012 | 0.44 | 0.24-0.81 | .0077 | |
| Negative | 131 (87.3) | 183 (78.2) | .023 | 1 | 1 | ||||
| MRD on day 78 of frontline treatment | |||||||||
| <5 × 10−4 | 136 (86.6) | 213 (91.8) | 1 | 1 | |||||
| ≥5 × 10−4 | 21 (13.4) | 19 (8.2) | .098 | 4.22 | 2.87-6.21 | <.0001 | 3.00 | 1.98-4.54 | <.0001 |
Risk groups in relapsed patients with pB-ALL are defined as follows: S1, late (ie, >6 mo after cessation of frontline treatment) isolated extramedullary relapse; S3, early (ie, >18 mo after initial diagnosis and before 6 mo after cessation of frontline treatment) isolated bone marrow relapse; S4, very early (ie, within 18 mo after initial diagnosis) isolated or combined bone marrow relapse; S2, all others.16
CI, confidence interval; DXM, dexamethasone; MRD, minimal residual disease; NA, not applicable; PDN, prednisone.
No significant difference in survival after relapse was seen in the small group of patients with T-ALL and prednisone good-response (5 y-pSUR after relapse: prednisone 23.1%, SE 8.3%, n = 26, 20 deaths; dexamethasone 36.4%, 4.5%, n = 11, 7 deaths; P = .62).
Treatment-related complications and deaths in induction
Incidences of life-threatening and fatal adverse events related to the induction phase Protocol IA according to the randomized treatment arm and age are shown in Table 5.18 Overall, 64% of the life-threatening events and 69% of deaths were infection-related. The risk of a life-threatening infection increased over the time of the induction phase: 55% of induction-related life-threatening infections (63/114) and 43% of the fatal infections (18/42) developed after the fourth week of induction, with similar distribution over time in both treatment arms (data not shown). The majority of life-threatening and fatal infections was of bacterial origin (life-threatening [n = 113]: bacterial 43%, fungal 35%, viral 7%, infectious organism not identified/not known 15%; fatal [n = 42]: bacterial 38%, fungal 26%, viral 7%, infectious organism not identified/not known 29%); 31 of the 49 life-threatening and 13 of the 16 fatal bacterial infections were caused by gram-negative rods. The incidence of life-threatening and fatal infections was significantly higher in patients treated with dexamethasone compared with those who received prednisone, which was attributed to more bacterial and fungal infections as well as more infections of unknown origin (Table 5).
Treatment-related life-threatening adverse events related to induction therapy*
| . | Life-threatening adverse events† . | Fatal adverse events . | ||||
|---|---|---|---|---|---|---|
| . | DXM‡ . | PDN‡ . | P . | DXM‡ . | PDN‡ . | P . |
| N (%§) . | N (%§) . | N (%§) . | N (%§) . | |||
| All patients | 1770 | 1946 | 1770 | 1946 | ||
| All life-threatening events | 124 (7.0) | 53 (2.7) | <.0001 | 42 (2.4) | 19 (1.0) | .0011 |
| Infection-related | 80 (4.5) | 33 (1.7) | <.0001 | 29 (1.6) | 13 (0.6) | .0075 |
| Bacterial¶ | 33 | 16 | 10 | 6 | ||
| Fungal‖ | 29 | 11 | 8 | 3 | ||
| Viral | 4 | 3 | 0 | 3 | ||
| Organism nk/nd | 14 | 3 | 11 | 1 | ||
| Not infection-related | 44 (2.5) | 20 (1.0) | .0009 | 13 (0.7) | 6 (0.4) | .11 |
| Neurologic# | 14 | 5 | 4 | 1 | ||
| Gastrointestinal** | 12 | 4 | 3 | 0 | ||
| Liver | 2 | 0 | 2 | 0 | ||
| Pancreatitis | 2 | 3 | 0 | 1 | ||
| Thrombosis including SVT | 8 | 3 | 2 | 1 | ||
| Other | 6 | 5 | 2 | 3 | ||
| Age <10 y | 1458 | 1593 | 1458 | 1593 | ||
| All life-threatening events | 84 (5.8) | 32 (2.0) | <.0001 | 24 (1.6) | 8 (0.5) | .002 |
| Infection-related | 56 (3.8) | 22 (1.4) | <.0001 | 16 (1.1) | 6 (0.4) | .030 |
| Bacterial | 20 | 12 | 5 | 4 | ||
| Fungal | 22 | 6 | 4 | 0 | ||
| Viral | 4 | 2 | 0 | 2 | ||
| Organism nk/nd | 10 | 2 | 7 | 0 | ||
| Not infection-related | 28 (1.9) | 10 (0.6) | .0016 | 8 (0.5) | 2 (0.1) | .056 |
| Neurologic | 12 | 4 | 3 | 1 | ||
| Gastrointestinal | 5 | 3 | 1 | 0 | ||
| Liver | 2 | 0 | 2 | 0 | ||
| Pancreatitis | 1 | 0 | 0 | 0 | ||
| Thrombosis including SVT | 4 | 0 | 2 | 0 | ||
| Other | 4 | 3 | 0 | 1 | ||
| Age ≥10 y | 312 | 353 | 312 | 353 | ||
| All life-threatening events | 40 (12.8) | 21 (5.9) | .0028 | 18 (5.8) | 11 (3.1) | .13 |
| Infection-related | 24 (7.7) | 11 (3.1) | .0091 | 13 (4.2) | 7 (2.0) | .11 |
| Bacterial | 13 | 4 | 5 | 2 | ||
| Fungal | 7 | 5 | 4 | 3 | ||
| Viral | 0 | 1 | 0 | 1 | ||
| Organism nk/nd | 4 | 1 | 4 | 1 | ||
| Not infection-related | 16 (5.1) | 10 (2.8) | .16 | 5 (1.6) | 4 (1.1) | .74 |
| Neurological | 2 | 1 | 1 | 0 | ||
| Gastrointestinal | 7 | 1 | 2 | 0 | ||
| Liver | 0 | 0 | 0 | 0 | ||
| Pancreatitis | 1 | 3 | 0 | 1 | ||
| Thrombosis including SVT | 4 | 3 | 0 | 1 | ||
| Other | 2 | 2 | 2 | 2 | ||
| . | Life-threatening adverse events† . | Fatal adverse events . | ||||
|---|---|---|---|---|---|---|
| . | DXM‡ . | PDN‡ . | P . | DXM‡ . | PDN‡ . | P . |
| N (%§) . | N (%§) . | N (%§) . | N (%§) . | |||
| All patients | 1770 | 1946 | 1770 | 1946 | ||
| All life-threatening events | 124 (7.0) | 53 (2.7) | <.0001 | 42 (2.4) | 19 (1.0) | .0011 |
| Infection-related | 80 (4.5) | 33 (1.7) | <.0001 | 29 (1.6) | 13 (0.6) | .0075 |
| Bacterial¶ | 33 | 16 | 10 | 6 | ||
| Fungal‖ | 29 | 11 | 8 | 3 | ||
| Viral | 4 | 3 | 0 | 3 | ||
| Organism nk/nd | 14 | 3 | 11 | 1 | ||
| Not infection-related | 44 (2.5) | 20 (1.0) | .0009 | 13 (0.7) | 6 (0.4) | .11 |
| Neurologic# | 14 | 5 | 4 | 1 | ||
| Gastrointestinal** | 12 | 4 | 3 | 0 | ||
| Liver | 2 | 0 | 2 | 0 | ||
| Pancreatitis | 2 | 3 | 0 | 1 | ||
| Thrombosis including SVT | 8 | 3 | 2 | 1 | ||
| Other | 6 | 5 | 2 | 3 | ||
| Age <10 y | 1458 | 1593 | 1458 | 1593 | ||
| All life-threatening events | 84 (5.8) | 32 (2.0) | <.0001 | 24 (1.6) | 8 (0.5) | .002 |
| Infection-related | 56 (3.8) | 22 (1.4) | <.0001 | 16 (1.1) | 6 (0.4) | .030 |
| Bacterial | 20 | 12 | 5 | 4 | ||
| Fungal | 22 | 6 | 4 | 0 | ||
| Viral | 4 | 2 | 0 | 2 | ||
| Organism nk/nd | 10 | 2 | 7 | 0 | ||
| Not infection-related | 28 (1.9) | 10 (0.6) | .0016 | 8 (0.5) | 2 (0.1) | .056 |
| Neurologic | 12 | 4 | 3 | 1 | ||
| Gastrointestinal | 5 | 3 | 1 | 0 | ||
| Liver | 2 | 0 | 2 | 0 | ||
| Pancreatitis | 1 | 0 | 0 | 0 | ||
| Thrombosis including SVT | 4 | 0 | 2 | 0 | ||
| Other | 4 | 3 | 0 | 1 | ||
| Age ≥10 y | 312 | 353 | 312 | 353 | ||
| All life-threatening events | 40 (12.8) | 21 (5.9) | .0028 | 18 (5.8) | 11 (3.1) | .13 |
| Infection-related | 24 (7.7) | 11 (3.1) | .0091 | 13 (4.2) | 7 (2.0) | .11 |
| Bacterial | 13 | 4 | 5 | 2 | ||
| Fungal | 7 | 5 | 4 | 3 | ||
| Viral | 0 | 1 | 0 | 1 | ||
| Organism nk/nd | 4 | 1 | 4 | 1 | ||
| Not infection-related | 16 (5.1) | 10 (2.8) | .16 | 5 (1.6) | 4 (1.1) | .74 |
| Neurological | 2 | 1 | 1 | 0 | ||
| Gastrointestinal | 7 | 1 | 2 | 0 | ||
| Liver | 0 | 0 | 0 | 0 | ||
| Pancreatitis | 1 | 3 | 0 | 1 | ||
| Thrombosis including SVT | 4 | 3 | 0 | 1 | ||
| Other | 2 | 2 | 2 | 2 | ||
DXM, dexamethasone therapy in induction phase Protocol IA; nd, no data; nk, not known; PDN, prednisone therapy in Protocol IA9,10 ; SVT, sinus venous thrombosis.
The table includes all life-threatening events that were related to therapy and occurred during or after induction Protocol IA before start of consolidation element Protocol IB.
An adverse event was considered as life-threatening if its occurrence placed the patient at immediate risk of death. An adverse event that might have caused death, if it had occurred in a more severe form, was not considered as life-threatening.
Randomization group as treated in induction.
Percentages are related to the total number of randomized patients treated in the respective arm.
DXM: gram-negative rods, n = 22 (9 patients died); gram-positive rods, n = 5 (1 patient died); gram-positive coccals, n = 9 (1 patient died). PDN: gram-negative rods, n = 9 (4 patients died); gram-positive rods, n = 3 (1 patient died); gram-positive coccals, n = 4 (1 patient died).
Fungal infections were according to the EORTC/MSG criteria.18 DXM: molds, n = 17 (7 patients died); yeasts, n = 4 (1 patient died); fungus not identified/no data, n = 8 (1 patient died). PDN: molds, n = 3 (2 patients died); yeasts, n = 6 (1 patient died), fungus not identified/no data, n = 2.
DXM: seizure/signs of encephalopathy, n = 7 (1 patient died); cerebral infarction/hemorrhage, n = 6 (3 patients died); severe psychosis, n = 1. PDN: seizure/signs of encephalopathy, n = 3; cerebral infarction/hemorrhage, n = 2 (1 patient died).
DXM: gastrointestinal perforation, n = 6 (1 patient died); gastrointestinal bleeding, n = 5 (1 patient died), necrotizing enterocolitis/esophagitis, n = 1 (died). PDN: gastrointestinal perforation, n = 2, gastrointestinal bleeding, n = 2.
A higher incidence in the dexamethasone-treated patients could also be found for the noninfectious treatment complications, which could in particular be shown for events of neurologic and gastrointestinal etiology (Table 5).
Osteonecrosis
Only patients from the BFM group were included in the analyses of osteonecroses because collection of these data was not prospectively done in the AIEOP group.
Because randomization was stopped for patients at the age of 10 years or older in October of 2004, only patients with ALL diagnosis before this date were included in those analyses that were performed across age groups, to avoid a bias as a result of the nonrepresentative age distribution in the entire randomized cohort. The age-stratified analyses were done including all randomized BFM patients.
Five-year cumulative incidence of osteonecrosis was 4.7% (SE 0.5%, n = 1737, 84 osteonecroses). Incidence was higher in patients 10 years of age or older and increased with age (Figure 4A). There was no difference in 5-year cumulative osteonecrosis incidence between the randomization groups, neither in the total group (dexamethasone 4.3% [SE 0.7%], prednisone 5.1% [SE 0.7%]; P = .69 [ALL diagnosis before 10/2004]) nor stratified by age groups (Figure 4B).
Cumulative incidence of osteonecrosis in patients of the BFM group. Data are shown (A) in age groups (1 to <6, 6 to <10, 10 to <15, 15 to <18 years) and (B) in age groups (1 to <10, 10 to <18 years) and randomization arm as treated. 5 y-CIO, 5-year cumulative incidence of osteonecrosis; DXM, dexamethasone; ON, number of osteonecrosis; PDN, prednisone; SE, standard error.
Cumulative incidence of osteonecrosis in patients of the BFM group. Data are shown (A) in age groups (1 to <6, 6 to <10, 10 to <15, 15 to <18 years) and (B) in age groups (1 to <10, 10 to <18 years) and randomization arm as treated. 5 y-CIO, 5-year cumulative incidence of osteonecrosis; DXM, dexamethasone; ON, number of osteonecrosis; PDN, prednisone; SE, standard error.
Discussion
Replacement of prednisone (60 mg/m2 per day) with dexamethasone (10 mg/m2 per day) during ALL induction treatment in the AIEOP-BFM ALL 2000 trial resulted in a highly significant reduction of the relapse rate by about one third. In the era of ALL-BFM protocols, no other intervention had a comparable impact on relapse reduction since the implementation of reinduction treatment in the 1970s.19 This is all the more striking, because the effect resulted from a single antileukemic agent within the setting of multiagent chemotherapy. Dexamethasone proved to be most effective in the prevention of extramedullary relapses, which is consistent with more even tissue distribution in general and better penetration of the blood-brain barrier compared with prednisone.6 The higher antileukemic effectiveness of dexamethasone, however, came at the cost of a significantly higher incidence of induction-related life-threatening events and deaths, which diminished but did not eliminate its favorable effect on event-free survival. At the interim analysis, adolescent patients appeared to be at particular risk of serious treatment complications. Thus, 4 years into the trial, this led to the decision to stop the randomization for patients 10 years of age and older, based on the recommendation of an external data and safety monitoring committee.
Despite the remarkable overall relapse reduction observed in the dexamethasone group, no relevant effect could be shown for patients with prednisone poor-response. This might reflect a general glucocorticoid and multidrug resistance of the leukemic cells of these patients, which cannot be overcome even by dexamethasone. In addition, a positive effect of dexamethasone might be obscured by the more intensive therapy administered to patients with prednisone poor-response.
A significant relapse reduction with dexamethasone was also seen in the randomized trials CCG-1922 for NCI standard-risk patients and MRC-ALL97, using lower glucocorticoid induction doses than in our trial (40 mg/m2 per day prednisone and 6.0 or 6.5 mg/m2 per day dexamethasone, respectively).20,21 The overall relapse incidence and event-free survival rates of the dexamethasone arms were comparable in CCG-1922, MRC-ALL97, and our trial, although the incidence of CNS relapses was lower in our trial. However, event-free survival of patients in the prednisone arm in CCG-1922 and MRC-ALL97 was inferior to the results in our trial, thus resulting in a more pronounced benefit from dexamethasone in those trials (HRs of event-free survival in CCG-1922, MRC-ALL97, and AIEOP-BFM ALL 2000 were 0.65, 0.68, and 0.85, respectively). The randomized trials L95-14 of the Tokyo Children’s Cancer Study Group22 and EORTC CLG 5895123 studied the effect of dexamethasone vs prednisone during induction using dexamethasone doses of 8 mg/m2 per day or 6 mg/m2 per day, respectively. The prednisone dose was 60 mg/m2 per day in both trials. No relapse reduction by the use of dexamethasone could be shown in these trials, with the exception of a marginally significant lower incidence of CNS relapse in the EORTC trial. This suggests that the benefit of dexamethasone compared with prednisone (60 mg/m2 per day) may be blurred if the dexamethasone dose is reduced.
The higher incidence of induction-related death in the dexamethasone arm of our trial was also reflected by a higher rate of life-threatening toxicity. Among the life-threatening infections, we observed an excess of bacterial (primarily gram-negative rods) as well as fungal (primarily molds) infections in the dexamethasone arm. A higher incidence in dexamethasone-treated patients could also be shown for life-threatening neurologic and gastrointestinal complications. The gastrointestinal toxicity mainly manifested as gastric bleedings and perforations without clearly different patterns in the 2 treatment arms. Etiologies of the neurologic events were more heterogeneous, and specific patterns that differed between the 2 arms were also not evident.
No significant difference in early treatment deaths could be demonstrated between the randomization arms in the CCG-1922 and MRC-ALL97 trials, a finding that at first sight seems to be in contrast to our results.20,21 However, the rate of early deaths in the dexamethasone arm of MRC-ALL97 was also more than twice that of the prednisone arm, though not reaching statistical significance. Furthermore, for direct comparison of our results with those of the CCG-1922 trial, we assessed the difference in death rates before CR between the randomization arms in NCI standard-risk patients and also found no statistically significant difference in this subgroup in our trial (supplemental Table 5). In the Japanese L95-14 trial, a trend toward a higher rate of induction-related infectious deaths was observed in the dexamethasone arm,22 whereas no difference in early treatment-related deaths was seen in the EORTC CLG 58951 trial.23 A considerably higher incidence of toxic deaths in induction was also reported for the Dana-Farber Cancer Institute ALL trial 91-01P using dexamethasone in induction (6 mg/m2 per day) compared with the previous and subsequent trials with prednisone (40 mg/m2 per day).24 In summary, all of these data show that dexamethasone tends to be more toxic with a higher risk of treatment-related mortality in the context of different treatment protocols.
Published data indicate an effect of dexamethasone exposure on the incidence of osteonecrosis.25-28 The overall high incidence of aseptic osteonecroses in the adolescent patients in our study was thus a matter of concern, although it was comparable with the incidence reported in other ALL trials.23,25,27 However, we did not find an excess of aseptic osteonecroses in the patients treated with dexamethasone in our study. This was in line with the findings in the EORTC CLG 589501 and UK MRC ALL97 randomized trials,21,23 although the osteonecrosis rate reported in trial MRC ALL97 was strikingly lower than in our trial.
The objective of treatment intensification is to prevent relapses. However, the mere relapse incidence does not take into account the burden of treatment. Using event-free survival as an endpoint also considers the effects of treatment burden if they lead to a predefined event such as death or second malignancy. This critical reflection of the different types of events is important when evaluating the quality of treatment, because patients with relapsed ALL have a realistic chance to be rescued by a second-line therapy.16,29,30 The evaluation is even more complicated if a considerably higher treatment burden in the experimental arm does not result in a significantly higher death rate and is therefore not reflected when calculating event-free survival rates. The AIEOP-BFM ALL 2000 study produced a statistically significant difference in 5-year event-free survival of 3% between the dexamethasone and prednisone arms in the large group of 3720 patients. This result reflects a relapse reduction from 15% to 10% in the dexamethasone arm, which came at the cost of induction-related treatment deaths in 2.5% of these patients compared with 0.9% in the prednisone arm. Furthermore, because survival after relapse in the prednisone arm exceeded the survival after relapse in the dexamethasone arm, overall survival was equal in the 2 randomization arms. The significantly better survival after relapse in the prednisone arm could be demonstrated for the largest subgroup in our trial (ie, for patients with pB-ALL and prednisone good-response). The findings suggest that the more intensive induction treatment with dexamethasone especially reduced the incidence of less resistant and better salvageable relapses. This was substantiated by a lower rate of prognostically favorable features among the patients who had relapsed in the dexamethasone arm, such as positivity for ETV6-RUNX1, favorable relapse risk group (S1/S2),16 or favorable treatment response during the first-line therapy (ie, MRD load of < 5 × 10−4 at week 12) (Table 4).
Unlike patients with pB-ALL and prednisone good-response, patients with T-ALL and prednisone good-response had a clear benefit from dexamethasone not only in terms of relapse reduction and better event-free survival, but also with respect to better overall survival. Besides the fact that this patient subgroup showed the largest relapse reduction with dexamethasone from 17% to 7% with an HR of 0.4 (Figure 3Di), survival after relapse was comparable in the 2 randomization groups, and the prognosis after relapse was in general extremely poor, contributing to a clearer translation of event-free survival into survival.
Altogether, our data show that the intensity of front-line treatment may thus influence survival after relapse. This is an important limitation on the evaluation of front-line treatments, with event-free survival as the primary endpoint. Using overall survival as the only endpoint, however, bears the risk that success or failure of the relapse treatment might distort the effect of the tested therapy. Moreover, this would require higher patient numbers to reach sufficient statistical power. Many pediatric ALL trials are therefore not powered to detect the expected differences in overall survival as is also the case in our trial. Treatment with a protocol that results in better event-free survival despite similar overall survival reduces the number of patients who need relapse treatment, thus saving these patients from the additional burden of this high-intensity additional treatment, often including hematopoietic stem cell transplantation. Doubtless, this is of benefit for individual patients. However, it is counterbalanced by a large proportion of patients who do not benefit from the intensified first-line treatment, but are subjected to the risk of more toxicity. In our study, this would concern 97% of the patients that received the more toxic therapy without benefit to save 3% of the patients from relapse treatment.
Significant relapse reduction and improvement in event-free survival without significant improvement in overall survival has also been experienced in other studies31,32 and will be a relevant matter of debate in modern trials in pediatric oncology. Large subgroups of patients have reached a very high level of outcome,33-38 and considerable improvements have also been achieved for patient subgroups with unfavorable prognosis.17,39,40 There is a substantial risk that further treatment intensification may lead to a shift from relapses to fatal and also relevant nonfatal toxicity.
The results of the randomized study AIEOP-BFM ALL 2000 led to a stratified use of dexamethasone during induction in the subsequent ongoing trial AIEOP-BFM ALL 2009: Patients with prednisone poor-response or other criteria qualifying for the treatment in the high-risk group, as well as patients with pB-ALL and prednisone good-response, receive prednisone (60 mg/m2 per day) in induction. Patients with T-ALL and prednisone good-response are treated with dexamethasone (10 mg/m2 per day) after the prednisone prephase. To prevent severe infectious complications, strong guidelines regarding close clinical monitoring of the patients have been established in the protocol.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the patients and families who participated in this trial, the physicians and nurses of all hospitals for their contribution in performing this study, and the study committees for productive discussions during the development and progress of the trial. They also thank the partners in the reference laboratories and all the technicians for their expert work in cytology, genetics, and MRD diagnostics; and the data managers for their careful study conduction.
This study was supported by Comitato M. L. Verga and Fondazione Tettamanti (Monza), Fondazione Città della Speranza, Fondazione Cariparo (Padova), Associazione Gian Franco Lupo (Pomarico), Associazione Italiana per la Ricerca sul Cancro (IG 5017: A.B., G.C., M.G.V.; special grant 5x1.000: F.L.), Fondazione Cariplo (A.B.), Ministero dell’Istruzione, Università e Ricerca (A.B., F.L.); Deutsche Krebshilfe e.V., (grant 50-2698 Schr1 and grant 50-2410 Ba7), Oncosuisse/Krebsforschung Schweiz (grant OCS 1230-02-2002), and St. Anna Kinderkrebsforschung Austria.
Authorship
Contribution: M. Schrappe, V.C., M.Z., M.G.V., M. Stanulla, A.B., M.A., G.M., F.L., R.B., C.R.B., and F.N. were involved in designing and planning the study; A.M. and M. Schrappe wrote the manuscript; A.M., M. Stanulla, A.B., F.L., F.N., M.A., A.A., R.B., A.E.K., L.L.N., B.K., J.G., R.P., R.C., A.v.S., E.B., C.R., V.C., and M. Schrappe helped in collecting the data and contributed patients to the study; M.G.V. and M.Z. were the study statisticians; M.G.V., M.Z., A.M., and D.S. oversaw data checking and reporting during the study period and analyzed the data; G.C. was responsible for MRD analyses in the Italian part of the study and helped collect data; R.R. and G.B. were responsible for the immunologic analyses in the German and Italian part of the study, respectively, and helped collect data; J.H. was responsible for the genetic analyses in Germany and helped collect data; and all authors approved the final version of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Martin Schrappe, Department of Pediatrics, Christian-Albrechts-University Kiel and University Medical Center Schleswig-Holstein, Campus Kiel, Schwanenweg 20, 24105 Kiel, Germany; e-mail: m.schrappe@pediatrics.uni-kiel.de.
References
Author notes
V.C. and M. Schrappe contributed equally to this study.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal