In this issue of Blood, Ciciliano et al demonstrate that thrombus formation in ferric chloride (FeCl3) thrombosis models relies on physiochemical, rather than biological, mechanisms.1
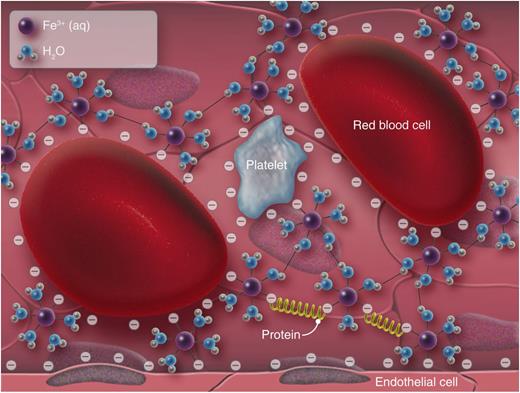
Ferric ions permeate through the endothelium into the lumen. These positively charged ions suppress the negative charge on blood cells, endothelial cells, and plasma proteins, which allows them to form agglomerates. This charge-based mechanism allows blood cells and proteins to accumulate on the vessel wall independent of hemostatic mechanisms. Professional illustration by Luk Cox, Somersault18:24.
Ferric ions permeate through the endothelium into the lumen. These positively charged ions suppress the negative charge on blood cells, endothelial cells, and plasma proteins, which allows them to form agglomerates. This charge-based mechanism allows blood cells and proteins to accumulate on the vessel wall independent of hemostatic mechanisms. Professional illustration by Luk Cox, Somersault18:24.
The FeCl3 model is the most widely used animal model of thrombosis, but its mechanism remains a source of debate. It was originally assumed that thrombus formation was initiated through the generation of reactive oxygen species, leading to denudation of endothelial cells, and subsequent exposure of the prothrombotic subendothelium. This assumption has been called into question by careful light and electron microscopy studies showing that red blood cells (RBCs), rather than platelets, are the first blood cells to adhere to FeCl3-treated endothelial cells,2 and evidence of platelet adhesion and aggregation independent of collagen and fibrinogen receptors.3 Ciciliano et al provide evidence that initial blood cell adhesion is an artifact of ferric ions leaking into the bloodstream leading to flocculation.
Flocculation is a separation strategy in the chemical industry to remove suspended solids or soluble impurities from fluids using metal salts or charged polymers. The mechanism of flocculation relies on charge suppression and entrainment. FeCl3 is one of the more common “coagulants” used, for instance, in water treatment to remove solids. The hydrated form of the ferric ion, Fe(H2O)63+, is positively charged and therefore suppresses the charge around negatively charged cells, effectively bringing them closer together and allowing them to agglomerate. Further hydrolysis results in insoluble ferric hydroxide, Fe(OH)3, that precipitates and entrains agglomerates into large “flocs.” This charge-based mechanism appears to be the missing link needed to describe blood cell adhesion to FeCl3-treated endothelial cells.
Ciciliano et al show in vivo that ferrous ions permeate through the endothelium into the bloodstream at micromolar concentrations. Ferric ions at these concentrations cause flocculation of not only platelets and RBCs, but also plasma proteins. In endothelialized microfluidic channels, ferric ions at these concentrations cause the accumulation of plasma proteins, platelets, and RBCs under flow. The authors propose a 2-step process: the first step is physiochemical, where primarily RBCs, and also platelets and plasma proteins, agglomerate on the vessel wall through a flocculation-like mechanism (see figure). In the second step, wall-bound agglomerates promote thrombus formation by familiar mechanisms associated with platelet function and coagulation. These data suggest that FeCl3 is a poor initiator of vessel wall injury. However, propagation of the thrombus across the lumen, at least at low iron ion concentrations, may resemble thrombosis. The depth into the lumen at which flocculation mechanisms give way to thrombotic mechanisms is difficult to determine and depends on a number of parameters that affect the transport of iron ions through the endothelium, including the size and composition of the vessel wall and the concentration and application of FeCl3. Variability in the transition from physiochemical to biological mechanisms may explain some of the contradictory results reported in the FeCl3 model.3
Is this the death knell for the FeCl3 model? Unlikely, because despite its now well-documented shortcomings,1-3 it is still cheaper, faster, and simpler than most other thrombosis models. It is also sensitive to genetic modifications that affect platelet function, as well as antiplatelet and anticoagulation agents. However, the nonbiological induction of thrombus formation makes it difficult to extrapolate conclusions from this model to human arterial or venous thrombosis that, as far as we know, initiates from an injured, stressed, or otherwise activated endothelium. Fortunately, new animal models of thrombosis provide more biologically relevant stimuli. Cooley developed a model in which the epigastric artery from a mouse is everted and then inserted into the carotid artery or femoral vein of another mouse.4 The adventitia provides a prothrombotic substrate to flowing blood, resulting in large platelet-rich thrombi. Characteristics of human deep vein thrombosis are reproduced by partial ligation of the inferior vena cava.5 Here, innate immune cells adhere to P-selectin on activated endothelial cells followed by the initiation of coagulation by blood cell–derived tissue factor. In both models, the stimuli for thrombus formation are cell and/or extracellular matrix derived rather than chemical, mechanical, or thermal as in other models.
The microfluidic approach used here adds to what is a growing number of in vitro models in experimental hematology.6 Ciciliano et al show the power of these approaches by performing a set of studies that incorporate endothelial cells and whole blood under flow that would be impossible in vivo. The same group used this approach to model hemolytic uremic syndrome.7 Others have recreated vessel geometries characteristic of stenosed vessels8 and even entire vascular networks such as the circle of Willis.9 Importantly, these models are often in close agreement with conclusions drawn from analogous animal models. Physiologically inspired geometries, when combined with the appropriate chemical and mechanical cues, can recreate microenvironments with clinically relevant results, for example, in the production of platelets from stem cell–derived megakaryocytes.10 Although animal models play a central role in biomedical research, and likely will for the foreseeable future, advances in microfabrication, microfluidics, and 3-dimensional printing are providing new models that use human or human-derived cells to complement, and in some cases replace, animal models.
Conflict-of-interest disclosure: The author declares no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal