Abstract

Introduction: Donor cell-derived leukemia/lymphoma (DCL) is an extremely rare complication after allogeneic hematopoietic stem cell transplantation (HSCT). Due to the rarity of DCL, most of the available data have been limited to case reports or small case series, and the number of the patients was still insufficient to understand the clinical features of DCL and to assess the risk factors for its development. In this study, we aimed to obtain the clinical perspectives and identify possible risk factors for DCL by conducting a survey based on data from the nationwide registry of the Japan Society for Hematopoietic Cell Transplantation (JSHCT).
Patients and Methods: In this study, DCL was defined as hematologic malignancy including leukemia, lymphoma, and myelodysplastic syndrome (MDS) which were confirmed as donor origin based on short tandem repeat analysis or fluorescence in situ hybridization (FISH) for sex chromosomes. Our survey identified 40 DCL from 36,870 allogeneic HSCT performed between 1974 and 2012 which achieved engraftment.
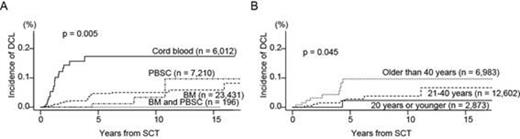
Results: The median interval from HSCT to DCL diagnosis was 22 months (range, 3-190 months). Incidence of DCL was estimated as 0.12 ± 0.02% at 5 years, 0.13 ± 0.02% at 10 years, and 0.16 ± 0.03% at 15 years from HSCT. The incidence was correlated with types of stem cell sources, 0.09 ± 0.02% with bone marrow (n = 23,431), 0.02 ± 0.02% with PBSC (n = 7,210), no DCL with combined BM and PB (n = 196), while 0.35 ± 0.09% with CB (n = 6,012) with statistical significance (Figure A, p = 0.0047). When limited to HSCT performed after 2004 (n = 20,346), the incidence of DCL after CB transplantation (n = 4,966, 0.29 ± 0.09%) was significantly higher than that of non-CB transplantation (n = 15,380, 0.09 ± 0.03%, p = 0.0013). Excluding CB, older age was associated with higher incidence of DCL, 0.05 ± 0.05% with donor ≤ 20 years old, 0.06 ± 0.03% with donor of 21-40 years old, and 0.20 ± 0.07% with donor > 40 years old (Figure B, p = 0.045). On the other hand, patient age did not show statistical significance with incidence of DCL.
No significant difference in the incidence of DCL was noted between other factors. The incidence was not different between gender match/mismatch (0.10 ± 0.03% with gender match and 0.17 ± 0.04% with gender mismatch, p = 0.56). G-CSF usage also did not show correlation with incidence of DCL (0.14 ± 0.03% for HSCT with G-CSF, 0.10 ± 0.07% for HSCT without G-CSF, p = 0.47). Underlying disease of patients, conditioning regimen (with or without TBI), and GVHD prophylaxis did not correlated with incidence of DCL.
Of the 40 DCL, 7 were lymphoid malignancy (2 ALL and 5 B-cell lymphoma) and the rest were myeloid malignancy (10 AML and 23 myelodysplastic syndrome). In the seven patients with lymphoid DCL, two B-cell lymphoma had alteration affecting chromosome 8q24, and one ALL case had t(4;11). In the 33 patients with myeloid DCL, -7 (n = 5), +8 (n = 3) and +21 (n = 2) were recurrently observed. Of note, +8 and +21 were mainly detected in AML, whereas all of -7 patients was MDS. Overall survival probability was estimated as 36.4 ± 8.1% at 4 years from diagnosis of DCL. Our survey obtained information regarding donor health condition from 11 related donors. Only one donor developed MDS with gain of chromosome 8, which was the same feature with DCL, but the rest of the donors did not develop hematological malignant diseases afterwards.
Conclusion: CB was a risk factor for DCL development compared to other stem cell sources, and it also should be noted that donor age affected the incidence of DCL. Our study revealed the frequency and risk factors for DCL. Given the results, especially the high frequency of CB-derived DCL, dominance of myeloid phenotype, and distribution of cytogenetic abnormalities, we are convinced that DCL is not a natural occurrence of hematological malignancy. Further molecular and immunological investigation would clarify the pathogenesis of DCL, and may provide additional clues for the understanding of the underlying mechanism of typical hematological malignancies.
Nakaseko:Otsuka: Honoraria, Research Funding; Pfizer: Honoraria, Research Funding, Speakers Bureau; BMS: Honoraria, Research Funding, Speakers Bureau; Novartis: Honoraria, Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal