Abstract
Introduction: The randomized phase 3 ENDEAVOR study (NCT01568866; N=929) demonstrated that carfilzomib and dexamethasone (Kd) significantly improved progression-free survival (PFS) compared with bortezomib (BTZ) and dexamethasone (Vd) (median 18.7 vs 9.4 months; hazard ratio [HR]: 0.53; 95% confidence interval [CI]:0.44-0.65; P<.0001) (Dimopoulos, J Clin Oncol 2015;33:abstr 8509; Dimopoulos, Haematologica 2015;100[s1]:abstr LB2071) in relapsed multiple myeloma (RMM). Herein, we present a subgroup analysis of treatment with Kd or Vd after first relapse vs ≥2 prior lines of therapy; the effect of previous exposure to BTZ or lenalidomide (LEN) was also investigated.
Methods: Adult patients with RMM (1-3 prior lines of therapy) were eligible. Patients were randomized 1:1 to Kd or Vd. Patients in the Kd arm received carfilzomib (30-min intravenous [IV] infusion) on days 1, 2, 8, 9, 15, and 16 (20 mg/m2 on days 1 and 2 of cycle 1; 56 mg/m2 thereafter) and dexamethasone 20 mg on days 1, 2, 8, 9, 15, 16, 22, and 23 of a 28-day cycle. Patients in the Vd arm received BTZ 1.3 mg/m2 (IV or subcutaneously) on days 1, 4, 8, and 11 and dexamethasone 20 mg on days 1, 2, 4, 5, 8, 9, 11, and 12 of a 21-day cycle. Cycles were repeated until disease progression or unacceptable toxicity. The primary end point was PFS. Secondary end points included overall survival, overall response rate (ORR), duration of response, rate of grade ≥2 peripheral neuropathy (PN), and safety.
Results: A total of 929 patients were randomized (Kd: 464; Vd: 465). The proportion of patients with 1 (Kd: 50.0%; Vd: 49.9%) vs ≥2 (Kd: 50.0%; Vd: 50.1%) prior lines of therapy and with previous exposure to BTZ (Kd: 53.9%; Vd: 54.2%) or LEN (Kd: 38.1%; Vd: 38.1%) was balanced between the treatment arms. The proportion of patients with prior BTZ or LEN exposure was also balanced across treatment arms within the subgroups of patients with 1 and ≥2 prior lines of therapy.
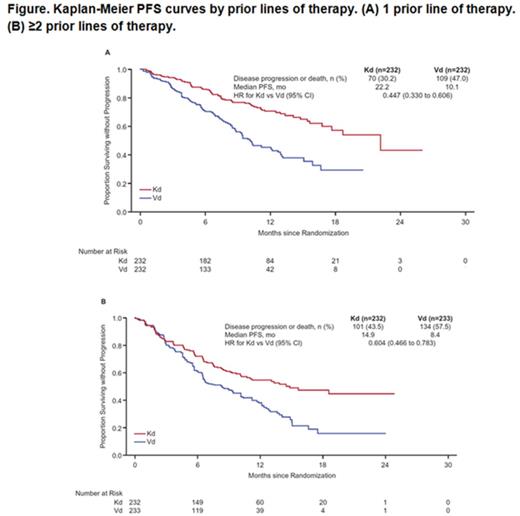
Efficacy outcomes by prior lines of therapy are shown in the Table; PFS curves are shown in the Figure. Median PFS for patients with 1 prior line was 22.2 months (95% CI: 17.7-not estimable [NE]) for Kd vs 10.1 months (95% CI: 8.8-12.7) for Vd (HR: 0.45; 95% CI: 0.33-0.61). Median PFS for patients with ≥2 prior lines was 14.9 months (95% CI: 10.2-NE) for Kd vs 8.4 months (95% CI: 6.5-10.2) for Vd (HR: 0.60; 95% CI: 0.47-0.78). Median PFS for Kd vs Vd was 15.6 months vs 8.1 months (HR: 0.56; 95% CI: 0.44-0.73) for patients with prior BTZ exposure and NE vs 11.2 months (HR: 0.48; 95% CI: 0.36-0.66) for patients without prior BTZ exposure. Median PFS for Kd vs Vd was 12.9 months vs 7.3 months (HR: 0.69; 95% CI: 0.52-0.92) for patients with prior LEN exposure and 22.2 months vs 10.2 months (HR: 0.43; 95% CI: 0.32-0.56) for patients without prior LEN exposure. ORRs (≥partial response) for Kd vs Vd were 81.9% vs 65.5% (odds ratio [OR]: 2.38; 95% CI: 1.55-3.66) in patients with 1 prior line and 72.0% vs 59.7% (OR: 1.74; 95% CI: 1.18-2.56) in patients with ≥2 prior lines. ORRs for Kd vs Vd were 71.2% vs 60.3% (OR: 1.63; 95% CI: 1.12-2.36) in patients with prior BTZ exposure, 83.6% vs 65.3% (OR: 2.72; 95% CI: 1.72-4.31) in patients without prior BTZ exposure, 70.1% vs 59.3% (OR: 1.60; 95% CI: 1.03-2.49) in patients with prior LEN exposure, and 81.2% vs 64.6% (OR: 2.37; 95% CI: 1.62-3.47) in patients without prior LEN exposure.
Grade ≥3 adverse events (AEs) were reported in 69.8% (Kd) and 63.9% (Vd) of patients with 1 prior line and 76.6% (Kd) and 69.9% (Vd) of patients with ≥2 prior lines. Rates for grade ≥3 AEs of interest by prior lines of therapy are presented in the Table. Grade ≥3 hypertension, dyspnea, and cardiac failure were more common with Kd vs Vd. The rate of grade ≥2 PN was lower with Kd vs Vd in patients with 1 prior line (6.5% vs 30.0%; OR: 0.16; 95% CI: 0.09-0.29) and ≥2 prior lines (5.6% vs 34.1%; OR: 0.12; 95% CI: 0.06-0.22).
Conclusion: There was a clinically meaningful improvement in PFS for patients with RMM who were treated with Kd compared with Vd regardless of the number of prior lines of therapy (1 or ≥2). This improvement was most notable for those with just 1 prior line, where median PFS was improved by over 1 year with Kd vs Vd. PFS benefit with Kd vs Vd was observed regardless of prior exposure to specific agents, including BTZ and LEN. A higher ORR was also observed with Kd vs Vd across prior treatment subgroups. Kd had a favorable benefit-risk profile in RMM, irrespective of prior treatment. Kd should be considered in patients who have progressed on LEN maintenance.
Moreau:Novartis, Janssen, Celgene, Millennium, Onyx Pharmaceuticals: Consultancy, Honoraria. Joshua:Celgene: Membership on an entity's Board of Directors or advisory committees. Palumbo:Novartis, Sanofi Aventis: Honoraria; Celgene, Millennium Pharmaceuticals, Amgen, Bristol-Myers Squibb, Genmab, Janssen-Cilag, Onyx Pharmaceuticals: Consultancy, Honoraria. Goldschmidt:Janssen: Consultancy, Honoraria, Research Funding; Celgene: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Research Funding; Onyx: Consultancy, Honoraria; Amgen: Consultancy; Takeda: Consultancy; BMS: Consultancy, Research Funding; Chugai: Honoraria, Research Funding; Millennium: Honoraria, Research Funding. Hájek:Janssen-Cilag: Honoraria; Celgene, Amgen: Consultancy, Honoraria. Facon:Onyx/Amgen: Membership on an entity's Board of Directors or advisory committees. Ludwig:Janssen Cilag: Honoraria, Speakers Bureau; Bristol Myers Squibb: Honoraria, Speakers Bureau; Onyx: Honoraria, Speakers Bureau; Celgene Corporation: Honoraria, Speakers Bureau; Takeda: Research Funding. Niesvizky:Celgene, Millennium, Onyx: Consultancy, Speakers Bureau. Oriol:Celgene, Janssen, Amgen: Consultancy, Speakers Bureau. Rosiñol:Celgene, Janssen: Honoraria. Gaidano:Celgene: Research Funding; Morphosys, Roche, Novartis, GlaxoSmith Kline, Amgen, Janssen, Karyopharm: Honoraria, Other: Advisory Boards. Weisel:Celgene: Consultancy, Honoraria, Other: Travel Support, Research Funding; Amgen: Consultancy, Honoraria, Other: Travel Support; Janssen: Consultancy, Honoraria, Other: Travel Support, Research Funding; Onyx: Consultancy, Honoraria; Novartis: Other: Travel Support; Takeda: Other: Travel Support; Noxxon: Consultancy; Bristol Myers Squibb: Consultancy, Honoraria, Other: Travel Support. Gillenwater:Onyx, Amgen: Employment, Other: Stock. Mohamed:Onyx/Amgen: Employment, Other: Stock. Feng:Amgen/Onyx: Employment, Equity Ownership. Dimopoulos:Celgene,Onyx, Janssen, Novartis, Amgen: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal