Abstract
Relapse remains a major barrier to the long-term overall survival (OS) of pediatric patients with acute lymphoblastic leukemia (ALL). Allogeneic HSCT is a potentially curative option for these patients and its mechanism relies on graft-versus-leukemia (GvL) and delivery of high-dose chemotherapy. However, the mechanism and degree of GvL in curing ALL is not fully understood. Unrelated cord blood (CB) is an attractive donor option for these patients due to rapid procurement and lenient HLA matching without increased graft-versus-host disease (GvHD). Despite less GvHD, relapse is not increased when compared to other donor sources. Therefore, through collaboration between Eurocord, PDWP-EBMT and Duke University, we performed a retrospective analysis to identify risk factors associated with relapse, and the role of GvHD (as time dependent co-variate) in preventing relapse after unrelated CB transplantation (CBT) for children with ALL.
We analyzed 640 children (<18 years (y)) with ALL in complete remission (CR) who received a single-unit CBT in either first (n=257, 40%) or second (n=383, 60%) CR from 2000-2012. Most patients were diagnosed with B-cell (79%) or T-cell (18%) lineage ALL and had no CNS involvement (92%). Cytogenetic data was available for 411 patients (CR1=171, CR2=240), and 37% were considered intermediate risk and 36% poor risk. Pre-transplant, 49% of patients were CMV seropositive. All patients received myeloablative regimens and most received anti-thymocyte globulin (88%). Regimens included total body irradiation (TBI; 69%) with either cyclophosphamide (Cy)+Fludarabine (Flu; 10%) or other agents (59%), Busulfan (Bu)+ Cy (16%), or Thiotepa+Bu+Flu (8%). Most patients received HLA mismatched CBs at 1 (50%) or 2+ (34%) loci. GvHD prophylaxis included cyclosporine with either steroids (72%) or mycophenolate mofetil (21%), or other agents (6%).
Considering CR1 patients only, the median age at CBT was 5.3 y. Most were diagnosed with B-cell ALL (75%) and approximately half of those with known cytogenetics were considered poor risk. The median duration from diagnosis to CBT was 6.7 months and median follow up was 47 months. Estimated OS and LFS at 5 y for CR1 patients was 59% and 52%, respectively. Improved OS and LFS were associated with TBI-containing regimens and younger age at time of CBT (Table 1). The CI of relapse at 5 y was 23% for CR1 patients. In a multivariate analysis (MVA) the presence of acute GvHD (grade II-IV) and TBI-containing regimens were both protective of relapse (Table 1). No impact of GvHD was observed on OS, LFS or NRM.
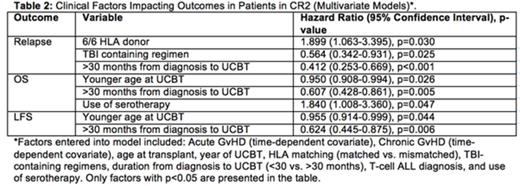
In CR2 patients, the median age at CBT was 6.9 y. Disease was primarily B-lineage ALL (82%) with intermediate or poor risk cytogenetics in 40% and 28% of patients, respectively. Median time from diagnosis to CBT was 36 months and median follow up was 54 months. Estimated OS and LFS in CR2 patients were 46% and 44%, respectively. In MVA, younger age and longer duration from diagnosis to CBT (>30 months) was associated with improved OS and LFS (Table 2). Conversely, the use of ATG was associated with lower OS.
In CR2 patients, the CI of relapse was 28%. In MVA, longer duration from diagnosis to CBT (>30 months) and receiving TBI were both associated with less relapse. Importantly, receiving a fully matched HLA CB graft was a strong risk factor for increased relapse compared to mismatched CB recipients. Acute GvHD (II-IV) in this cohort was associated with higher mortality but not with relapse.
In this large retrospective collaborative study, we investigated the impact of GvHD as a marker of GvL in pediatric ALL patients after CBT. In CR1 patients, acute GvHD and use of TBI were protective of relapse. However in CR2 patients, use of TBI, longer duration from diagnosis to CBT and HLA mismatched grafts were associated with decreased incidence of relapse but not with the presence of GvHD. These results showed that the impact of GvHD as a GvL marker is more evident in CR1 patients than CR2. Whereas, the impact of HLA mismatch CB on relapse is more important in CR2 patients. Decreasing immunosuppression more rapidly for CR1 patients or avoiding HLA identical CB for CR2 patients should be further investigated. In both cohorts, TBI has shown to be an important protective factor for relapse.
Bader:Riemser: Other: Institutional grants; Neovii: Other: Institutional grants; Medac: Other: Institutional grants; Amgen: Consultancy; Novartis: Consultancy; Jazz Pharmaceuticals: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal