Abstract
INTRODUCTION: Patients with Hodgkin Lymphoma (HL) relapsing post autologous transplant (ASCT) are not cured with standard chemotherapy. In addition, a subset of patients with relapsed or primary-refractory HL fare poorly with ASCT. Such patients may benefit from allogeneic transplantation (allo-HCT) with its graft-versus-lymphoma (GVL) effect.
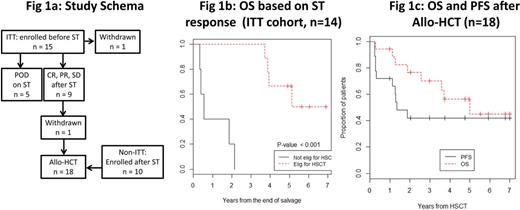
METHODS: We performed a phase II study of salvage therapy (ST) followed by allo-HCT in adult patients with relapsed/refractory (rel/ref) HL (NCT00574496, Fig. 1a). Conditioning was dictated by PET status after ST, with NMA flu/cy/TBI 200 cGy for patients in CR and RIC mel/flu for those with PR/SD. Patients in the intent-to-treat (ITT) cohort were enrolled prior to ST and proceeded to allo-HCT if in CR, PR, or SD after 1 line of ST. The primary endpoint was successful allo-HCT and PFS at 1 year after allo-HCT (estimated as a proportion as all patients had at least 1 year of followup). Landmark analysis (from end of ST) with Kaplan-Meier curves and log-rank test were used to compare OS and PFS in the ITT cohort. A second cohort of patients referred with CR, PR, or SD after ST received HCT on protocol, but was not included in the ITT analysis. No differences in OS or PFS after HCT were seen between ITT and non-ITT cohorts, and patients were combined for further analysis. OS and PFS from time of HCT were estimated using all HCT patients, and PFS was compared based on baseline covariates. Cumulative incidence of GVHD, relapse/POD and nonrelapse mortality (NRM) were estimated using competing risks methodology. P-values less than 0.05 were considered significant.
RESULTS: From 6/2008 to 6/2014, 25 patients were consented, 15 on the ITT analysis and 10 on the post-ST arm (Table 1). All had relapse after ASCT, primary refractory or high-risk HL relapsed within 1 year of 1st-line therapy. Allografts (n = 18) were PBSC from matched or single-allele mismatched related (n = 8) or unrelated (n = 3) donor, or double unit cord blood grafts (n = 7). Eleven were in PET CR before HCT and 7 in PR. ITT analysis (n=15): 5 patients had POD on ST and were ineligible for allo-HCT. Of the remaining 9, 1 withdrew during conditioning. 1-year and 3-year OS were 50% (95% CI 22.5, 100) and 16.7% (95% CI 2.8, 99.7), respectively, in patients with POD after ST, and 100% at both time points if no POD after ST (Fig 1b). At median 5.6 years of follow-up, 5 patients survive. The percent of patients successfully meeting the primary endpoint was 33% (95% CI 13, 61). Allo-HCT analysis (n=18): Cumulative incidence (CI) of grade 2-4 and 3-4 aGVHD at d+100 were 23.3% (95% CI 13.1, 55.3) and 11.1% (95% CI 1.70, 30.4), respectively. CI of cGVHD at 1 year and 3 years was 11.1% (95% CI 1.7, 30.7) and 35.6% (95% CI 13.2-59.0), respectively, and of mild severity in all but 1 patient. 3-year CI of relapse/POD was 34.3% (95% CI 13.2-56.7), and NRM 23.6% (95% CI 6.8, 46.1). Estimated 3-year PFS was 42.1% (95% CI 24.1, 73.6) and OS 70.3% (95% CI 51.5, 96.1) (Fig 1c). There was no significant association between PFS and disease stage or status (CR vs. PR). There was a trend toward poorer PFS in the 5 patients without prior ASCT (3 year PFS 20.0% vs. 50.8%, p = 0.088), 3 of whom had primary refractory HL.
CONCLUSION: We demonstrate that allo-HCT provides long-term survival for a substantial portion of patients with rel/ref HL. Though limited by small sample size, the ITT analysis showed more than 1/3 of patients never attained sufficient disease control for allo-HCT, and have a dismal prognosis. Of note, none had received brentuximab or a checkpoint inhibitor, and the long-term impact of these agents in those patients remains to be seen. In patients undergoing allo-HCT with chemosensitive disease, proceeding to allo-HCT in PET PR vs. CR had no significant negative impact on PFS in this limited sample. The trend toward poor outcomes in patients who had not previously undergone ASCT likely reflects poor prognosis in patients with primary refractory disease. Factors informing prognosis after allo-HCT, and interventions to attenuate risk, remain an important area for further investigation.
Patient characteristics
| . | Median (range) age in yrs . | Median (range) prior lines of therapy . | N (%) prior ASCT . | Stage at relapse . | Disease status pre-ST . | Disease status pre-HCT . |
|---|---|---|---|---|---|---|
| ITT (n = 15) | 32 (22-51) | 3 (1-4) | 8 (53.3) | III: 4 IV: 11 | 1st relapse: 6 ≥ 2nd relapse: 5 Refractory: 4 | 7 CR 2 PR 5 POD 1 withdrew |
| All HCT (n = 18) | 36 (24-53) | 4 (2-6) | 13 (72.2) | II: 1 III: 4 IV: 13 | 1st relapse: 3 ≥ 2nd relapse: 11 Refractory: 4 | 11 CR 7 PR |
| . | Median (range) age in yrs . | Median (range) prior lines of therapy . | N (%) prior ASCT . | Stage at relapse . | Disease status pre-ST . | Disease status pre-HCT . |
|---|---|---|---|---|---|---|
| ITT (n = 15) | 32 (22-51) | 3 (1-4) | 8 (53.3) | III: 4 IV: 11 | 1st relapse: 6 ≥ 2nd relapse: 5 Refractory: 4 | 7 CR 2 PR 5 POD 1 withdrew |
| All HCT (n = 18) | 36 (24-53) | 4 (2-6) | 13 (72.2) | II: 1 III: 4 IV: 13 | 1st relapse: 3 ≥ 2nd relapse: 11 Refractory: 4 | 11 CR 7 PR |
Perales:BeTheMatch/ National Marrow Donor Program: Membership on an entity's Board of Directors or advisory committees; Takeda: Honoraria; Astellas: Honoraria; Merck: Honoraria; Amgen: Honoraria. Giralt:TAKEDA: Consultancy, Honoraria, Research Funding; JAZZ: Consultancy, Honoraria, Research Funding, Speakers Bureau; AMGEN: Consultancy, Research Funding; SANOFI: Consultancy, Honoraria, Research Funding; CELGENE: Consultancy, Honoraria, Research Funding. Straus:Millenium Pharmaceuticals: Research Funding. Moskowitz:GSK: Research Funding; Merck: Consultancy, Research Funding; Seattle Genetics: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal