Abstract
Background: Targeting specific immune inhibitory receptors (iRs) with monoclonal antibodies has led to paradigm-shifting treatment practices in a variety of solid cancers. These advances were in part driven by tremendous progress in phenotypic and functional characterization of altered iR expression patterns and memory T cell differentiation states such as exhaustion and senescence. Effector T cell dynamics and iR expression patterns in AML patients (pts) at diagnosis and after induction chemotherapy are not well understood and, if deciphered, are poised to be critically important for optimal integration of therapeutic blockade of various iRs in the clinic.
Methods: We analyzed T cell dynamics and iR expression in peripheral blood (PB, n=45) and bone marrow (BM, n=38) cells from 49 pts (median age 60, range 21-76) with newly diagnosed AML. After induction, 36 (73%) pts entered complete remission (CR) whereas 13 (27%) were non responders (NR). Samples were collected at diagnosis, upon recovery after induction and following consolidation/salvage chemotherapy. Using multi-parameter flow cytometry, we characterized the differentiation status (CD45RA, CCR7), and the expression of co-stimulatory receptors (CD27, CD28) and iRs. Our gating strategy excluded NK T cells (CD3+ CD56+) from downstream analyses. Co-expression of iRs was analyzed in combination of 3 (2B4, BTLA, TIM3) or 4 (KLRG-1, CD57, PD-1 and CD160) markers. As a control, we used PB (n=41)/BM (n=16) lymphocytes from healthy controls (HC). Percentage of cells expressing specific markers were log transformed and modeled with mixed-effect linear regression models. Differential response outcomes over time were tested with interaction terms. Co-expression of multiple iRs was also analyzed with SPICE software version 5.3.
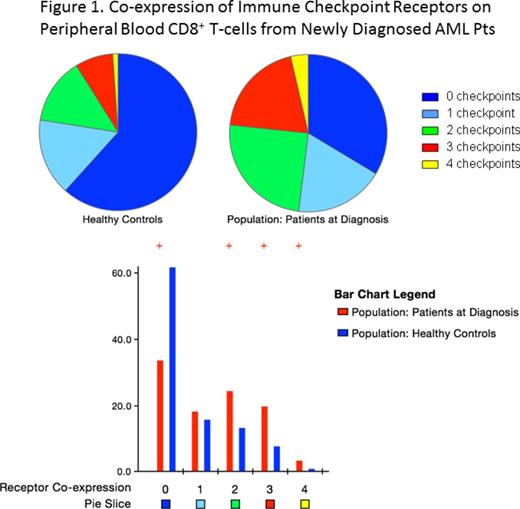
Results: At diagnosis, AML pts showed significantly lower median frequency of CD8+ naïve (CD45RA+ CCR7+) T cells in PB, but higher frequencies of terminal differentiated effector memory (TEMRA; CD45RA+ CCR7-) and phenotypically senescent CD8+ CD27- CD28- CD57+ T cells. Significantly higher percentages of PB CD4+ and CD8+ T cells were found to express PD1 and 2B4 compared to HC. Additionally, the frequency of PB CD8+ T cells co-expressing 2-4 iRs was significantly higher in the PB of AML pts (Fig.1). Surprisingly, in contrast to PB, the only significant finding in the BM of AML pts at diagnosis was increased frequency of CD8+ CD27- CD28- CD57+ T cells (p<0.001) compared to HC.
At the time of hematopoietic recovery from chemotherapy, TEMRAs and CD8+ CD27- CD28- CD57+ T cells significantly decreased in PB and BM of AML pts, compared to pretreatment levels. However, if analyzed by response, frequencies of these populations declined only in CR pts (p<0.001), but remained unchanged in NR pts. Analysis of iR co-expression in relation to the response to chemotherapy and time revealed that the frequency of CD8+ T cells co-expressing multiple IRs decreases in CR pts but increases in NR pts. These response-associated changes in iR co-expression were observed only in BM while, in PB, the iR co-expression profile remained unchanged irrespective of response.
Finally, we assessed the effect of diverse pre-treatment factors on T cell composition at AML diagnosis. We found that older age was associated with increased frequency of CD8+ T cells expressing the iR marker KLRG-1 and the senescent T cell phenotype CD8+ CD27- CD28- CD57+ (p<0.001) but age did not affect iR co-expression on T cells in either PB or BM. CMV seropositivity was associated with increased CD8+ TEMRAs in PB and CD8+ T cells co-expressing multiple iRs (mostly Tim3 and 2B4) in both compartments. The effect of sex, cytogenetic risk group, or ELN category was insignificant.
Conclusion: Our study provides critical insights into T cell differentiation and iR expression at diagnosis and during the course of treatment in pts with AML. We have identified several dominant expression patterns suggesting that iR signatures are consistent with immune recognition of AML and their role in sculpting the effector T cell responses directed against AML cell populations. However, data need to be interpreted in the context of the anatomical compartment and non-inheritable variables such as CMV and age. While ongoing work is focused on the deciphering significance of IRs expression for the interpretation of T cell functionality, our data support the rationale for therapeutic blocking of iRs in AML.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal