Abstract
BH3-mimetic ABT-199 (venetoclax, VEN) is a selective small-molecule antagonist of the anti-apoptotic BCL-2 protein. It binds to BCL-2 specifically, causing the release of pro-apoptotic BAX and BH3-only proteins and induction of cell death. Our studies indicated that AML is a BCL-2 dependent disease that, in pre-clinical studies, responds robustly to VEN by induction of apoptotic cell death (Pan et al., Cancer Discovery 2014). As a single agent, VEN demonstrated clinical activity in relapsed/refractory AML, yet patients who initially responded ultimately developed resistance and progressed. In this study we investigated mechanisms of acquired resistance to VEN in preclinical AML models.
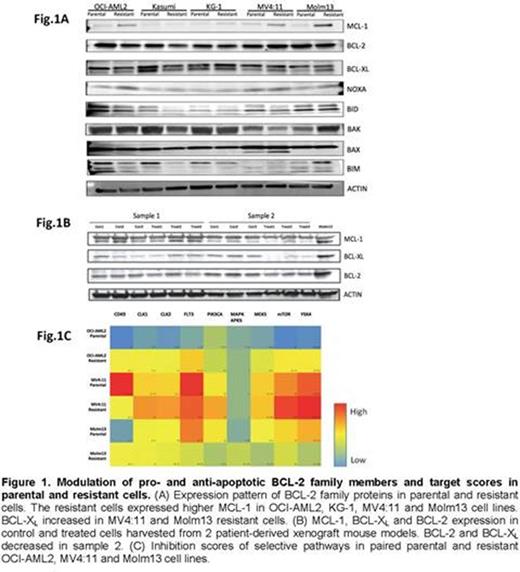
First, we generated 5 VEN-resistant cell lines (OCI-AML2, Kasumi, KG-1, MV4;11 and Molm13; with VEN cell-killing IC50s of 0.021µM, 0.046µM, 0.073µM, 0.020µM and 0.050µM, respectively) by exposing the cells to gradually increasing VEN concentrations. The IC50s of resistant cells are 15.2µM, 5.7µM, 31.6µM, 11.4µM and 15.4µM (124-723-fold greater than their parental counterparts). Protein analysis of resistant cells using immunoblotting demonstrated increased expression of MCL-1, a known resistance factor to VEN, in 4 resistant cell lines (OCI-AML2, KG-1, Mv4;11 and Molm13); and BCL-XL increase in MV4;11 and Molm13 resistant cells. To characterize the functional role of MCL-1 and BCL-XL in resistance to VEN, we co-treated parental and resistant cells with novel MCL-1 and BCL-XL- selective inhibitors (A-1210477 and A-1155463). The combination of VEN with A-1210477 or A-1155463 showed synergistic growth inhibition in all 5 parental cell lines (combination indices (CI) for A-1210477 were 0.15-0.62; CI for A-1155463 were 0.33-0.51, except >3 for KG-1). Notably, 4 out of 5 resistant cell lines (OCI-AML2, Kasumi, MV4;11, Molm13) became more sensitive to MCL-1 selective inhibitor A-1155463 but not to BCL-XL inhibitor A-1210477. However, no further effects were seen in resistant cells when combined with VEN.
We next compared sensitivity of three paired parental and resistant cell lines (OCI-AML2, MV4;11 and Molm13) to a library of 130 specific small-molecule inhibitors (Tyner, et.al.. Cancer Res. 2013). Cells were co-treated with VEN and each specific inhibitor, and drug target scores were calculated based on the IC50 of measured effectiveness of panel drugs against the cells. The screening revealed modulation of sensitivity to mTOR, MEK, and FLT3 pathways in resistant cells (Fig.1C). To confirm these findings, we next co-treated AML cells with VEN and specific inhibitors of the mTOR pathway (rapamycin and AZD2014) or MEK pathway (CI1040) in all 5 paired parental and resistant cell lines; or with FLT3 inhibitors (quizartinib and sorafenib) in parental and resistant MV4;11 and Molm13, which harbor FLT3-ITD. The combination of VEN and AZD2014 achieved synergistic effects in all 5 parental cell lines (CI AZD2014: 0.08-0.94), and VEN/rapamycin were synergistic in 3 parental cell lines (CI rapamycin: 0.00-0.55, except 1.76 for KG-1 and 1.59 for Molm13). Combination of VEN with CI1040 achieved synergy in OCI-AML2, Kasumi, MV4;11 and Molm13 parental cell lines (CI: 0.14-0.61). Finally, VEN/FLT3 inhibitors achieved synergistic effects in MV4;11 and Molm13 parental cell lines (CI quizartinib: 0.66-0.69; CI sorafenib: 0.64-0.71). The resistant cell lines exhibited sensitivity to these inhibitors as single agents, and no synergistic effects were seen when combined with VEN.
We have further induced in vivo resistance in two primary AML xenografts by treating NSG mice engrafted with 2nd passage AML cells with 100 mg/kg Q.D. VEN for 4 weeks followed by harvest of leukemic cells that repopulated the mouse after treatment discontinuation. While the proteomics, gene expression (RNAseq) and drug screening assays are in progress, preliminary immunoblotting studies demonstrated decreased expression of BCL-XL and BCL-2 (Fig.1B).
In summary, we identified multiple mechanisms of acquired resistance to VEN, which ultimately modulate the balance between pro- and anti-apoptotic BCL-2 family members. Our studies indicate that upfront combination of VEN with selective inhibitors of MCL-1, or with inhibitors of specific signaling pathways, can synergistically induce apoptosis in AML cells and conceivably prevent emergence of VEN resistance.
Leverson:AbbVie: Employment, Equity Ownership. Tyner:Aptose Biosciences: Research Funding; Constellation Pharmaceuticals: Research Funding; Janssen Pharmaceuticals: Research Funding; Array Biopharma: Research Funding; Incyte: Research Funding. Konopleva:Novartis: Research Funding; AbbVie: Research Funding; Stemline: Research Funding; Calithera: Research Funding; Threshold: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal