Abstract

Introduction
Cytokine Induced Killer (CIK) cells are memory T lymphocytes which have acquired CD56 expression and Natural Killer (NK) like unrestricted cytotoxicity, following in vitro activation by anti CD3 OKT3 and IFNg and subsequent expansion with IL-2.
CIK cells have demonstrated in vitro and in vivo anti tumor activity, direct intratumor homing following iv. administration and, more importantly, a very reduced Graft Versus Host (GVH) activity, in several experimental allogeneic models.
Indeed we and others have demonstrated very limited GVH activity in preliminary phase I studies, with donor derived (matched) CIK cells in patients with different hematological neoplasms, previously treated by allogeneic Hematopoietic Stem Cells (HSC) transplantations and subsequently relapsed of diseases 1.
Methods
To better delineate the toxicity profile, as well as the potential anti tumor efficacy, of donor derived CIK cells, we prospectively studied 48 patients relapsed after allogeneic stem cell transplantation performed using either a matched related (N=28) or unrelated donor (n= 20, including 1 haplo). This phase II multicenter study was authorized by Istituto Superiore di Sanità, as for Advanced Therapeutic Medicinal Product (ATMP) regulations, approved by the Agenzia Italiana del Farmaco and (AIFA). The trial was registered as (EUDRACT n 2008-003185-26, ClinicalTrial.gov: NCT01186809)
Results
In this interim analysis, forty-eight patients (including childrens and adults) have been so far enrolled into this study protocol. The median age was 48 (range 6-67) and a diagnosis of ALL (n=9, 20%), AML (n=29, 60%), MM (n=5, 8%), HD (n=3, 6%), MPN (n=2, 4%), NHL (n=1, 2%). Reasons for being enrolled into study was a hematologic relapse in 36 (75%) or a molecular relapse in 12 (25%).
The therapeutic strategy consisted of two infusions of unmanipulated DLI (each of 1 x 106/kg cells) at 3 weeks interval, followed by three infusions of donor derived CIK cells given at 3 weeks interval. The first 12 patients were treated with growing numbers of CIK cells, in groups of three patients per dose level. Since DLT was never observed (acute GVHD of grade III or more) the highest dose planned (5 x 106/kg, 5 x 106/kg and 10 x 106/kg) was then administered to subsequent consecutive 36 patients.
4 patients died for disease progression and 1 patient developed aGVHD (grade I, skin only) during the DLI treatment and could not proceed to the planned subsequent CIK administration. Of the 43 patients who eventually received at least one infusion of CIK cells, 15 patients did not complete the program, 9 for disease progression and death, 3 for insurgence of grade II aGVHD (skin only in 2 cases, skin and gut in 1 case), 1 for hemolytic anemia, 1 for insufficient cell supply and 1 for medical decision. Overall, 28 patients received the complete cell therapy planned (58%).
Overall, of the 48 patients enrolled, 5 (10%) suffered from aGVHD (1 grade I, 3 grade II, 1 grade III). During follow up, chronic GVHD was observed in 7 patients (14 %) (3 mild and 4 moderate).
As per protocol, clinical response was determined 100 days after the last CIK administration and the study was analyzed on an intent to treat basis. An early death occurred in 13 (27%) patients (4 during the DLI), before the clinical response could be evaluated. A CR was observed in 9 (19 %) and a PR in 7 (14%) for an overall response rate of 16 (33%). No response was observed in 19 (39%).
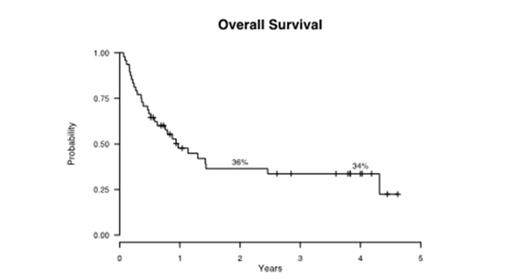
At 2 and 4 years, the event free survival of the 48 patients is 22% and 18%, while the overall survival is of 37% and 34%, respectively. For the small group of patients who achieved a complete response, the disease free survival is of 64% at 2 years and 51% at 4 years.
By univariate analysis, survival was significantly associated to the type of relapse (molecular) (p 0.0081) since at 2 and 4 years it was and 24% and 27% vs. 71% and 71 % for patients enrolled for a hematologic or a molecular relapses, respectively. By multivariate analysis, the type of relapse remained the only significant predictor of survival (0.0160 p value).
Conclusion
This study shows the feasibility of CIK preparation and administration as well as the relatively low toxicity of the program (10% aGVHD grades I-III) in spite of the fact that 20 patients received cells from matched unrelated donors. Finally, the study offers the suggestion that CIK cells may be efficacious to treat post-transplant relapse.
1 Introna M. et al, Haematologica, 2007, 92, 7, 948.
Introna:roche: Research Funding. Rambaldi:Roche: Honoraria; Novartis: Honoraria; Amgen: Honoraria; Celgene: Research Funding; Pierre Fabre: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal