Abstract
Background
Treatment of older (>60y) patients (pts) with AML remains challenging. Azacitidine (AZA) showed a trend towards a better overall survival (OS) in older pts with AML vs. conventional care (Dombret H, Blood. 2015) in the AZA-AML-001 trial. However, comparison between AZA and intensive chemotherapy (IC) was limited by the low number of subjects randomized to AZA or IC. The Medical Research Council (MRC) and the Leukemia Research Foundation (LRF) developed and validated a 1y survival risk index score in a large series of older AML pts (N=2843; AML11 and AML14 trials) treated with IC and non-intensive chemotherapy (NI), identifying 3 groups with different risk estimates (Wheatley K, B J Haematol, 2009).
Aim
To assess the impact of AZA as front-line therapy in older AML pts unfit for IC from different national registries who served as the basis for the European ALMA score (Spain, Italy, France and Austria), now expanded with the cases from PETHEMA AML Registry, and stratified by the MRC/LRF risk score, and to display a tentative nonrandomized comparison between IC, NI and AZA within those risk strata.
Methods
Retrospective analysis of 456 AML pts who received front-line AZA within drug label, off-label or compassionate named patient programs. Cytogenetic, age, white blood count (WBC), PS and AML type categorized pts as good, standard and poor-risk groups, as stated by Wheatley's score.
Results
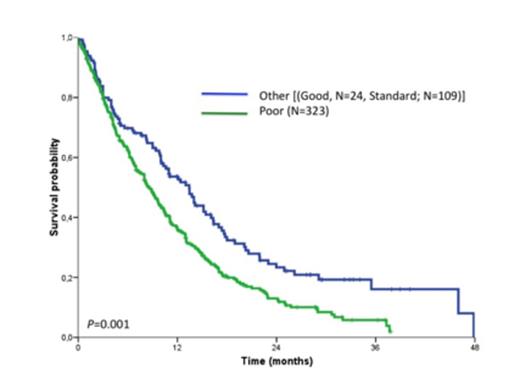
Baseline characteristics of pts and distribution across MRC/LRF risk categories are shown in Table 1. After accounting for the above 5 parameters, 323 pts (71%) were categorized as poor-risk (as compares to 31% and 37%, respectively, from the MRC/LRF AML11 and AML14 trials). The poor-risk subset included pts with age >75y (61%), adverse karyotype (45%), secondary AML (62%), WBC >10e9/L (32%) and PS³3 (6%). After 28 months median follow-up (95% CI: 25-31), median OS for the whole series was 9.7 months (95% CI: 8.5-11). Median OS for the good, standard and poor-risk groups was 15.1, 12.4 and 8.5 months, respectively (p=0.001. Fig 1), while 1y OS estimates were 64%, 51% and 36%, respectively. A comparison of these estimates with those of MRC/LRF trials are also shown in Table 1. As regard 1y OS, AZA therapy seems to confer a clinical benefit similar to that of IC, and superior to NI chemotherapy.
Conclusion
Although retrospective and non-matched, this is the largest comparison between AZA and IC in older AML pts. AZA therapy seems to confer a clinical benefit similar to IC, that in the poor-risk subset (n=323) might be even more relevant.
Baseline characteristics and 1y OS (N=456)
| Parameter . | N (%) . | ||||
|---|---|---|---|---|---|
| Age (median) | 75 (56-93) | ||||
| PS | 0-1: 345 (76) 2: 88 (19.5) >2: 19 (4.5) | ||||
| WCB (>109/L) | 103 (25) | ||||
| Therapy-related/AHD1 AML | 220 (48) | ||||
| Cytogenetic according to MRC2 | Inter: 245 (53.7) Adv: 150 (32.9) NA: 61 (13.4) | ||||
| Risk categories | Good: 24 (5.3) Standard: 109 (23.9) Poor: 323 (70.8) | ||||
| 1 year Overall Survival (%) | |||||
| AML113 | AML14I | AML14NI | AML14NIA | E-ALMA+ | |
| n | 1071 | 1137 | 275 | NA | 456 |
| Therapy | IC | IC | HU + LDAC +/- ATRA | LDAC +/- Mylotarg | AZA |
| MRC/LRF Risk group | |||||
| Good | 53 | 60 | 25 | 36 | 64 |
| Standard | 43 | 48 | 33 | 42 | 51 |
| Poor | 16 | 30 | 10 | 14 | 36 |
| Parameter . | N (%) . | ||||
|---|---|---|---|---|---|
| Age (median) | 75 (56-93) | ||||
| PS | 0-1: 345 (76) 2: 88 (19.5) >2: 19 (4.5) | ||||
| WCB (>109/L) | 103 (25) | ||||
| Therapy-related/AHD1 AML | 220 (48) | ||||
| Cytogenetic according to MRC2 | Inter: 245 (53.7) Adv: 150 (32.9) NA: 61 (13.4) | ||||
| Risk categories | Good: 24 (5.3) Standard: 109 (23.9) Poor: 323 (70.8) | ||||
| 1 year Overall Survival (%) | |||||
| AML113 | AML14I | AML14NI | AML14NIA | E-ALMA+ | |
| n | 1071 | 1137 | 275 | NA | 456 |
| Therapy | IC | IC | HU + LDAC +/- ATRA | LDAC +/- Mylotarg | AZA |
| MRC/LRF Risk group | |||||
| Good | 53 | 60 | 25 | 36 | 64 |
| Standard | 43 | 48 | 33 | 42 | 51 |
| Poor | 16 | 30 | 10 | 14 | 36 |
1Antecedent hematologic disorder
2Cytogenetic: Good: t(8;21), inv(16); Adverse: -5, -7, del(5q), abn(3q), complex (5 or more). Intermediate: Normal karyotype and all other abnormal karyotypes. NA: Not available.
3AML11 trial: 2 induction courses (cytarabine and anthracycline, ± thioguanine or etoposide). If CR: One or 3 consolidation courses ±I FN maintenance.
4AML14 included 2 schedules: Intensive (AML14I: 2 induction courses with daunorubicin and cytarabine. If CR: One consolidation course) and non-intensive (AML14NI: Hydroxicarbamide with LDAC, ±ATRA or AML14NIA: LDAC vs LDAC plus Mylotarg)
Survival probability
Falantes:Celgene: Honoraria. Off Label Use: Azacitidine in AML patients with >30% blasts. Pleyer:Celgene: Consultancy, Honoraria; AOP Orphan Pharmaceuticals: Honoraria; Novartis: Consultancy, Honoraria; Bristol-Myers Squibb: Consultancy, Honoraria. Itzykson:Oncoethix: Research Funding. Venditti:Celgene: Honoraria. Burgstaller:AOP Orphan Pharmaceuticals: Honoraria, Research Funding; Novartis: Honoraria; Celgene: Consultancy, Honoraria, Research Funding; Mundipharma: Honoraria. Musto:Celgene: Honoraria. Greil:AOP Orphan: Research Funding; GSK: Research Funding; Cephalon: Consultancy, Honoraria, Research Funding; Amgen: Honoraria, Research Funding; Eisai: Honoraria; Mundipharma: Honoraria, Research Funding; Merck: Honoraria; Janssen-Cilag: Honoraria; Genentech: Honoraria, Research Funding; Celgene: Consultancy; Ratiopharm: Research Funding; Sanofi Aventis: Honoraria; Pfizer: Honoraria, Research Funding; Boehringer-Ingelheim: Honoraria; Astra-Zeneca: Honoraria; Novartis: Honoraria; Bristol-Myers-Squibb: Consultancy, Honoraria; Roche, Celgene: Honoraria, Research Funding. Fenaux:Amgen: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Celgene Corporation: Honoraria, Research Funding. Ramos:GlaxoSmithKline: Honoraria; Janssen-Cilag: Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Honoraria; Celgene Corporation: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Amgen: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal