Abstract
Background/methods: Hodgkin lymphoma (HL) is characterized by elevations in serum cytokines and chemokines, produced by HL Reed-Sternberg cells and surrounding inflammatory cells, several which have been found to be prognostic and/or predictive for response to therapy. We previously reported the results of our phase II study evaluating PET-adapted salvage therapy with single-agent brentuximab vedotin (BV) followed by augmented ICE for patients with relapsed or refractory (rel/ref) HL (Lancet Oncology 2015). In this study, patients who failed 1 line of therapy for HL were treated with 2 cycles of BV, 1.2mg/Kg, administered weekly, 3 weeks on and 1 week off. Those who acheived PET-normalization proceeded directly to consolidation with autologous stem cell transplantation (ASCT). Those with persistent abnormalities on PET received augmented ICE prior to consideration for ASCT. Patients with localized, nodal-based disease that had not previously been radiated received involved field radiation prior to ASCT. Interleukin-6 (IL-6), interleukin-10 (IL-10), tumor necrosis factor-α (TNF-α), interferon-γ (IFN-γ), and cysteine-cysteine thymus and activation related chemokine (TARC) were measured at baseline and after 2 cycles of BV by multiplex enzyme-linked immunosorbent assay (ELISA) array. We aimed to evaluate the prognostic and predictive significance of these cytokines and chemokines in this uniformly treated patient population.
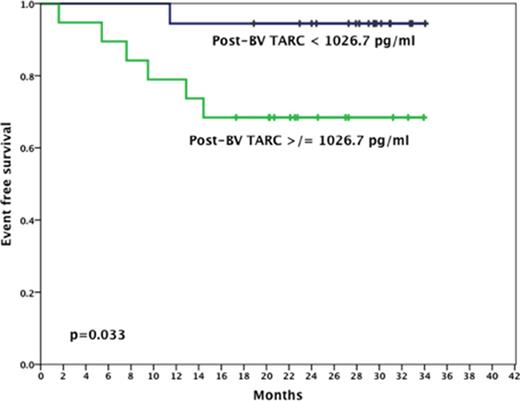
Results: Of the 45 patients enrolled onto this protocol 37 (82%) had serum samples available both at baseline and after 2 cycles of BV for analysis. Table 1 displays the median values and ranges at baseline and after treatment with BV. Baseline levels of IL-6, IL-10, TNF-α, IFN-γ, and TARC were abnormal in 32%, 8%, 78%, 97%, and 97%, respectively. Elevated baseline IFN-γ and IL-10 correlated with presence of extranodal sites of disease (p=0.003 and 0.049 respectively) whereas elevated IL-10 and TNF-α correlated with the presence of B-symptoms (p=0.019 and 0.019 respectively). With regard to response to treatment, percent change in TARC (TARC%) from baseline to post-BV predicted for PET-normalization following BV (OR 5.82, 95% C.I 1.18-43.74). Furthermore, lower post-BV TARC was significantly associated with improved event free survival (EFS) (2 year EFS 94% vs 67%, p=0.033) (Figure 1). No other factors correlated with response to therapy, event free survival, or overall survival.
Conclusions: To date, this is the largest series evaluating the prognostic and predictive significance of TARC in rel/ref HL patients treated with BV. Our analysis confirms the role of TARC as a biomarker of response to BV and PET-normalization. In line with its correlation with PET-normalization, post-BV TARC level was also predictive of EFS. Continued incorporation of TARC evaluation in prospective clinical trials for HL is warranted to better define its role in predicting PET-normalization and prognosis.
| Cytokine/chemokine . | Pre-brentuximab vedotin (pg/ml) . | Post-brentuximab vedotin (pg/ml) . | ||
|---|---|---|---|---|
| . | median . | range . | median . | range . |
| IL-6 | 2.27 | 0.10-154.44 | 1.41 | 0.09-34.00 |
| IL-10 | 0.38 | 0.09-112.29 | 0.45 | 0.14-17.53 |
| TNF-α | 2.55 | 0.55-15.15 | 2.25 | 0.58-22.31 |
| IFN-γ | 8.66 | 1.45-1553.67 | 9.01 | 2.62-112.83 |
| TARC | 8250.00 | 236.10-220773.00 | 1026.70 | 241.70-34453.00 |
| Cytokine/chemokine . | Pre-brentuximab vedotin (pg/ml) . | Post-brentuximab vedotin (pg/ml) . | ||
|---|---|---|---|---|
| . | median . | range . | median . | range . |
| IL-6 | 2.27 | 0.10-154.44 | 1.41 | 0.09-34.00 |
| IL-10 | 0.38 | 0.09-112.29 | 0.45 | 0.14-17.53 |
| TNF-α | 2.55 | 0.55-15.15 | 2.25 | 0.58-22.31 |
| IFN-γ | 8.66 | 1.45-1553.67 | 9.01 | 2.62-112.83 |
| TARC | 8250.00 | 236.10-220773.00 | 1026.70 | 241.70-34453.00 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal