Abstract
Background: Mitogen activated protein kinase (MAPK) pathway is activated in myeloid malignancies both mutationally and non-mutationally. Most frequent mutations are encountered in RAS genes. While direct inhibition of RAS has been elusive, MEK inhibition downstream of RAS is a viable alternative. Trametinib is an allosteric MEK 1/2 inhibitor with pre-clinical activity against multiple cell lines representative of myeloid malignancies. A Phase 1/2 trial in relapsed/refractory acute myeloid leukemia (AML), myelodysplastic syndrome (MDS) and chronic myelomonocytic leukemia (CMML) involving 97 patients showed remissions with or without recovery of counts in 20% of patients harboring mutations in RAS oncogenes.
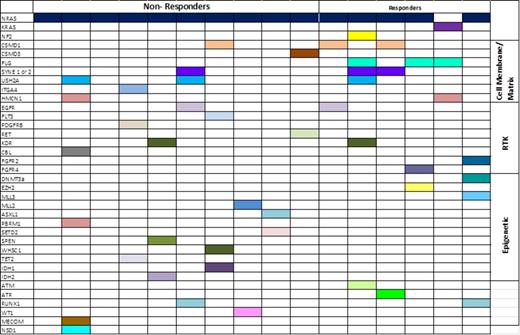
Methods: As responses were only seen among patients with RAS mutations, in collaboration with the Sheikh Khalifa Bin Zayed Al Nahyan Institute for Personalized Cancer Therapy (IPCT) at MD Anderson Cancer Center, we undertook sequencing of DNA extracted from bone marrow samples of 6 responders and 10 non-responders (all with RAS mutation) before treatment on a next generation sequencing (NGS) platform of 202 cancer-relevant genes All of these patients also had at least one follow up bone marrow sample collected during treatment or at loss of response.
Results: Patients were of median age of 69 years (range, 40-79) with median bone marrow blast count of 25 (range, 6-88), median WBC count of 6.1X109 /L (range, 0.4-29.3) and received a median of 2 prior therapies (range, 1-5). Cytogenetics was diploid in 6, complex/-7 in 5 patients. Fifteen of the sixteen patients had an NRAS mutation (Codon 12=9, codon 61=4, codon 13=1) and one patient had a KRAS mutation in codon 12. None carried concomitant mutation in NPM1, KIT or CEBPA genes, and one patient with an NRAS mutation also had a FLT3 D835 mutation. Median baseline RAS allelic burden was 34.4% (range, 18-73) with no difference among responders and non-responders. One non-responder lost the mutant NRAS allele at follow up but gained a FLT3 D835E mutation. There was no overall significant difference in RAS allelic burden at follow-up in non-responders or responders. The range of RAS allelic frequency change was a gain in 11% to a loss of 28% in non-responders and a 17% gain to a 20% loss in responders, for all patients with data collected before and after treatment.
Median baseline frequency of mutations or identified copy number changes was 7.25, including both responders (range, 4-16) and non-responders (range, 4-10). Before the start of treatment, 70% of the non-responders had additional mutations in genes encoding epigenetic regulators e.g. MLL2, SETD2, TET2, IDH1 or 2 etc. , compared with only 33% of responders (Fig.1). Of the 7 non-responders with mutations in an epigenetic regulator, we obtained data at follow-up on 6 patients. Each of these 6 patients retained the mutation at follow-up and an additional non-responder gained a mutation in an epigenetic regulator at follow-up. Interestingly 100% of responders had at least one mutation in a gene encoding a member of the cellular matrix and/or involved in cellular adhesion e.g. CSMD1, CSMD3, FLG, USH2A etc. before treatment, compared with only 50% of non-responders. This trend also persisted after treatment, with only one responder losing such a mutation.
Conclusion: Mutation analysis in a subset of patients with RAS mutations and myeloid malignancies treated with trametinib suggest presence of higher frequency of epigenetic mutations among non-responders. Further study is needed to determine whether the combination of MEK 1/2 inhibitor with epigenetic therapy may improve outcomes.
Cortes:Pfizer: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Teva: Research Funding; BerGenBio AS: Research Funding; Ariad: Consultancy, Research Funding; BMS: Consultancy, Research Funding; Astellas: Consultancy, Research Funding; Ambit: Consultancy, Research Funding; Arog: Research Funding; Celator: Research Funding; Jenssen: Consultancy. Jabbour:Pfizer: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal