Abstract
Background.
The AML is a heterogeneous disease with a high variety of subtypes stratified by cytogenetic and molecular markers. To date, the major prognosis criteria is cytogenetic, but 40-50% of de novo AML patients have normal karyotype; AML treatment is based on risk profiles depending on age and genetic molecular factor. New methods such as Next Generation Sequencing (NGS) and ex vivo sensitivity drug tests might be able to improve this classification and to individualize the treatment for AML patients.
Aims.
We performed targeted massively parallel sequencing on a 32 myeloid genes custom panel to identify a mutational profile of AML which predicts ex vivo pharmacological and clinical response.
Methods.
We analyzed bone marrow (BM) samples at diagnosis from 39 AML patients, 34 were treated with chemotherapy; 28 AML patients received one cycle of Idarubicin (Ida)/ Cytarabine(Cyt) induction treatment (3+7) and 8 received one cycle of Fludarabine/Cyt. Median age at diagnosis was 53 years (24-81), male:female ratio 19:16.
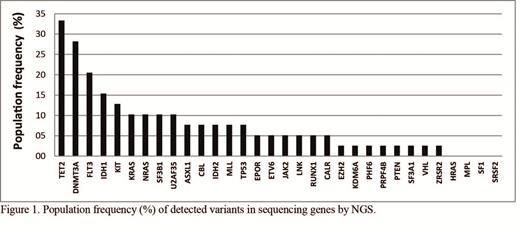
We carried out targeted gene sequencing by NGS (Ion Torrent Proton System-Life Technologies) using a 32 genes custom panel (all coding regions) implicated in leukemia prognosis, including ASXL1, CBL, DNMT3A, EPOR, ETV6, EZH2, FLT3, HRAS, IDH1, IDH2, JAK2, KDM6A, KIT, KRAS, LNK, MLL, MPL, NRAS, PHF6, PRPF40B, PTEN, RUNX1, SF1, SF3A1, SF3B1, SRSF2, TET2, TP53, U2AF35, VHL, ZRSR2 and CALR.
Ex vivo pharmacological studies were performed using an innovative automated flow cytometry method based platform (Ex-viTech) is able to evaluate effect of drugs used to treat AML, Cyt and Ida, using 4 parameter: Emax (Effective Maximum Response) measures potency, EC50 (Effective Concentration inducing 50% cell death) measures efficacy, and the activity was quantified by AUC (Area Under Curve) and VUS (Volume Under Superficies).
Clinical response was evaluated after induction treat. Complete remission was defined according to hematologic recovery and blast count fewer than 5%.
Analysis of NGS results was performed by Ion Report software. Differences measured by Exvitech were determined using t-test or Kruskal-Wallis test. Discrete variables of patients with and without gene variants were compared using the X2 test. For survival analysis we used Kaplan-Meier analysis (log rank) using SPSS 15. Two sided p values below 0.05 were considered statistically significant.
Results.
We found 94 non-synonymous variants (SNVs and small Indels) in coding regions. On average, 90.8% of the target sequence showed mean depth coverage ~ 1100x. See Figure 1.
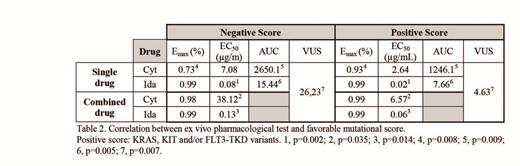
We analyzed results of pharmacological test by Ex-viTech plataform in function of presence of gene variants. Only significant favorable differences were detected: KRAS (Cyt-Emax p=0,000, Ida-EC50 p=0.001, VUS p=0.003, Cyt-AUC p=0.036, Ida-AUC p=0.000), KIT (VUS p=0,010) and FLT3-TKD (Cyt-Emax p=0.002, Cyt-AUC p=0.001, VUS p=0.011).
Mutational positive score, found it in 40% of patients, was defined by the presence of variants in KRAS, KIT and/or FLT3-TKD; it was correlated with pharmacological results and clinical response. All cases with positive score (n=13) achieve complete remission (CR); only 11 cases without favorable score (n=21) achieve RC (p=0.003) after induction treatment (See Table 2). In addition, response obtained for Ida Emax and Ida EC50 by Ex-viTech was able to detect patients who reached CR after induction treatment (p=0.042, p=0,039 respectively).
Ex-viTech results showed that patients with positive score have a significantly more potent and effective cytotoxic effect than patients without it. See table 2.
No differences were observed respect Overall Survival (OS) between cases with mutational favorable score and without it. However, we observed a plateau in OS with favorable mutational score. With a median follow-up of 5.9 months (1.9-25.74), patients having positive score showed better relapse free survival (p = 0.013). See Figure 3.
Conclusion.
Very deep sequencing NGS identifies a mutational profile score (KRAS, KIT or FLT3-TKD) in AML patients, which predicts ex vivo pharmacological and clinical response. This favorable score was found in 40% of AML patients. Merging NGS and ex vivo drug sensibility might be able early to predict response to induction and individualize treatments.
This study was funded by Instituto Carlos III (PI13/02387).
Ballesteros:Vivia Biotech: Employment.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal