Key Points
Pregnancy recalls short-lived immunity against TAAs mimicking antileukemic responses after allogeneic stem cell transplantation.
Abstract
Donor-derived immunity against tumor-associated antigens (TAAs) may exert selective antileukemic activity reprieving the allogeneic recipient from graft-versus-host disease. As TAAs are highly expressed in placental tissues we hypothesized that pregnancy could drive respective immunity in healthy individuals. Thus, we investigated the frequency and level of immune responses against clinically relevant TAAs in 114 blood donors and 44 women during their first pregnancy. Quantitative reverse-transcription polymerase chain reaction was employed to detect low levels of interferon-γ after primary peptide stimulation of CD8+ T lymphocytes. In blood donors, primary immune responses of low and/or high avidity were found against WT1 (15%), MUC1 (14%), PRAME (7%), and HER2/neu (5%) and exerted killing functions against leukemic cells. Men had higher responses than women, likely due to gonadal cancer-testis-antigen expression. Interestingly, a history of prior delivery was not associated with increased responses, whereas the strongest responses during pregnancy were found in early trimesters to disappear after delivery. This boost and loss of TAA-specific immunity suggests that virtually every donor harbors the potential to mount antileukemic immune responses in a recipient. However, in the absence of the driving target and a permissive environment, they are short-lived and thus require supplemental strategies such as vaccination or immunomodulation to facilitate their persistence.
Introduction
The graft-versus-leukemia (GVL) effect is the central component of the hematopoietic stem cell allograft’s ability to cure hematologic malignancies.1-3 Donor-derived T lymphocytes targeting minor histocompatibility antigens such as Y-chromosomal antigens in female-into-male transplants are well known to contribute largely to this strong immunologic effect, which may also cause graft-versus-host disease (GVHD) when the target antigen’s expression is not restricted to the hematologic site.4-9 Meanwhile, it has become evident that in addition to recognition of hematologically restricted minor histocompatibility antigens, donor T lymphocytes can exert selective GVL effects by recognition of tumor-associated antigens (TAAs) on leukemic tissues.10-12 The efficacy of these TAA-specific immune responses particularly depends on the level of antigen expression in the target tissue and the presence of a proinflammatory immune environment allowing donor-derived T lymphocytes of lower avidity to overcome peripheral tolerance and to attack the malignant cells in a selective manner.13,14
Rezvani et al first described the detection of immune responses against Wilms tumor protein 1 (WT1) in a smaller group of healthy stem cell donors and the expansion of WT1-specific T lymphocytes in the host.12 However, so far little is known about the exact frequency, origin, and functionality of TAA-directed immune responses in healthy donors awaiting their transfer into the host where an optimal immunologic environment and proper target expression facilitate their therapeutic potential.11,15,16 As it is evident that women can be immunized by pregnancies with male infants17,18 and transfer this immunity against Y-chromosomal–encoded antigens to male allograft recipients,19,20 we wanted to explore the possibility of pregnancy inducing immune responses against TAAs in healthy women, too. Indeed, several TAAs with clinical relevance in tumor and/or transplant immunotherapy such as human epidermal growth factor receptor 2 (HER2/neu), mucin 1 (MUC1), preferentially expressed antigen of melanoma (PRAME), and WT1 are highly expressed in placental tissues.21-24 Thus, we investigated the effects of pregnancy and gender on the frequency of immune responses against these TAAs in a large, prospectively designed cross-sectional study in 114 volunteer blood donors completed by longitudinal analyses in 44 first-time pregnant women.
Material and methods
Study design and subjects
Based on the preliminary experience from Rezvani et al,12 we hypothesized that 20% (p = 0.2) of HLA-A*02:01-positive healthy individuals could carry positive immune responses against WT1 and assumed that pregnancy increases this frequency.
In a cross-sectional analysis in volunteer blood donors (study group I), 3 subgroups should be analyzed including nulligravidous women, primi- or multiparous women, and men. Taking the potential effects of pregnancy into account, we hypothesized that nulligravidous women and men have a lower frequency (p1 = 0.1) and women with a history of delivery have a higher frequency (p2 = 0.4) of positive immune responses. Using a 2-sided χ2 test with a power of 80% (β = 0.2) and a level of significance of 95% (α = 0.05), at least 38 volunteers needed to be included for each subgroup to be able to show significant differences.
In a longitudinal analysis in healthy women during their first pregnancy (study group II), 3 time points were to be analyzed including the baseline at the first to second trimester, 1 to 4 days after delivery, and 2 to 3 months after delivery. To show significant differences between the time points, a paired χ2 test according to McNemar was applied to test the hypothesis that a conversion of immune responses from negative to positive results appears in the course of pregnancy. Using the parameters as stated above, at least 38 volunteers needed to be included for this study group. To compensate for expected loss of follow-up or the fact that sampling may not be possible at every time point, we decided to recruit at least 44 women at baseline. After an ethical amendment, additional blood samples should be drawn after completion of nursing where possible to extend the time period after pregnancy and consider the effects of alterations in peripheral blood counts as well as hormonal changes after delivery and nursing.
The original scientific study protocol and further amendments were approved by the local Ethical Committee of the Medical Faculty, University of Würzburg, Germany. All volunteers provided their written informed consent, in accordance with the Declaration of Helsinki.
Cell processing
Peripheral blood mononuclear cells (PBMCs) from healthy platelet donors were isolated from leukoreduction system chambers (Trima Accel apheresis apparatus, Terumo BCT, Lakewood, CO)25 or directly from venous blood by density-gradient centrifugation using LSM 1077 lymphocyte separation medium (PAA Laboratories GmbH, Cölbe, Germany). Additionally, 10 mL venous blood was drawn from pregnant women to obtain serum.
Peptide synthesis
Peptides were prepared by JPT Peptide Technologies (Berlin, Germany) to a minimum purity of 95%. The identity of each peptide was confirmed by mass spectral analysis. The following HLA-A*02:01–restricted peptides were used in this study as described elsewhere12,26-28 : CMV-pp65495-503 (NLVPMVATV), gp100209-217(210M) (IMDQVPFSV), HER2/neu369-377 (KIFGSLAFL), MUC1950-958 (STAPPVHNV), PRAME300-309 (ALYVDSLFFL), and WT1126-134 (RMFPNAPYL).
Restimulation of antigen-specific T lymphocytes
CD8+ T lymphocytes were purified from PBMCs using a commercially available kit (Dynabeads CD8 Positive Isolation Kit; Life Technologies, Darmstadt, Germany). For every condition, 1 × 106 CD8+ T lymphocytes were resuspended in RPMI 1640 (Life Technologies) supplemented with 10% (vol/vol) heat-inactivated human AB serum (HABS; PAA Laboratories) and rested overnight in 96-well round bottom plates in a humidified incubator at 37°C and 5% CO2. The next day, 1 × 106 T2 cells (ATCC CRL-199229 ) were pulsed with the respective peptides (peptide concentration of 0.1 and 10 µmol/L, as described elsewhere12 ) and incubated for 2 hours in serum-free RPMI 1640. After irradiation with a total dose of 30 Gy, peptide-pulsed T2 cells were washed once and coincubated with CD8+ T lymphocytes for 3 hours.
qRT-PCR
Interferon-γ (IFN-γ) messenger RNA (mRNA) expression upon antigen-specific stimulation was analyzed using quantitative reverse-transcription polymerase chain reaction (qRT-PCR). IFN-γ mRNA expression was normalized to CD8 mRNA levels and expressed as relative expression as compared with the stimulation with the irrelevant melanoma antigen Glycoprotein 100 (gp100). Total RNA was isolated using TRIzol reagent according to the manufacturer’s recommendations (Life Technologies). RNA integrity was verified using the Experion automated electrophoresis station from Bio-Rad Laboratories (Munich, Germany). Complementary DNA was synthesized from 1 µg total RNA using the iScript cDNA synthesis kit (Bio-Rad Laboratories). The following protocol was run on the thermal cycler Primus 96 (Peqlab Biotechnologie, Erlangen, Germany): 5 minutes at 25°C, 30 minutes at 42°C, and 5 minutes at 85°C. The qRT-PCR reactions were performed on a CFX96 real-time PCR system (Bio-Rad Laboratories) operated by CFX Manager Software 2.0 (Bio-Rad Laboratories). Thermal cycler parameters included 5 minutes at 95°C, 40 cycles at 95°C for 15 seconds, 60°C for 1 minute, and 72°C for 5 minutes. Reactions were prepared using the iScript Supermix ready-to-use solution (Bio-Rad Laboratories) with optimal concentration of reaction components. Primers and probes were synthesized by Eurofins MWG Operon, Ebersberg, Germany. Primer and probe sequences were used as described by Rezvani et al.12 Purified PCR products were sequenced to confirm their accuracy (SeqLab, Göttingen, Germany). All PCR reactions were performed in duplicates and reported as mean ± standard deviation.
Dextramer staining
PBMCs were stained using commercially available allophycocyanin (APC)-conjugated HLA-A*02:01 dextramer molecules (Immudex, Copenhagen, Denmark) loaded with the respective antigens. Briefly, cells were incubated in phosphate-buffered saline (Life Technologies) supplemented with 10% (vol/vol) heat-inactivated fetal calf serum (Sigma-Aldrich Chemie, Schnelldorf, Germany) for 20 minutes on ice. Cells were washed once and stained with the respective APC-conjugated dextramer for 30 minutes at room temperature (RT). Cells were washed and additionally stained with fluorescein isothiocyanate–conjugated anti-CD3 (SK7) and PerCP-conjugated anti-CD8 (SK1; both from BD Biosciences, Heidelberg, Germany) antibodies for 15 minutes at RT. Cells with the forward and side light scatter properties of lymphocytes were analyzed using a FACSCalibur flow cytometer (Becton-Dickinson, Heidelberg, Germany). Data analysis was performed using FlowJo 7.6.1 software (Tree Star, Ashland, OR).
Expansion of antigen-specific T lymphocytes
For each condition, thawed or freshly isolated 1 × 107 PBMCs were seeded on day −1 in 24-well plates at a density of 2.5 × 106 cells/mL in cytotoxic T lymphocyte (CTL) medium containing RPMI 1640 supplemented with 10% (vol/vol) heat-inactivated HABS, penicillin (100 U/mL; Life Technologies), streptomycin (100 µg/mL; Life Technologies), 2 mmol/L l-glutamine (Sigma-Aldrich), 12.5 mmol/L HEPES (N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid; Sigma-Aldrich), and 50 µmol/L 2-mercaptoethanol (Sigma-Aldrich). On day 0, cells were peptide-pulsed (0.1 and 10 µmol/L, respectively) and dextramer staining was performed as described above. On day 3, PBMCs were seeded in 12-well plates at a density of 2.5 × 106 cells/mL and restimulated with autologous peptide-pulsed, irradiated PBMCs and interleukin-2 (IL-2), IL-7, and IL-15 (all from Miltenyi Biotec, Bergisch Gladbach, Germany) at a final concentration of 30 U/mL (IL-2) and 5 ng/mL (IL-7 and IL-15), respectively. On days 6 and 9, PBMCs were stimulated with autologous peptide-pulsed, irradiated PBMCs and the cytokines mentioned above. On day 14, 1 batch of the cells was restimulated with Dynabeads Human T-Activator CD3/CD28 (Life Technologies) according to the manufacturer’s instructions. On days 16 (7 days after last peptide stimulation) and 21 (7 days after bead restimulation), cells were harvested, stained with dextramers, and functionally analyzed using CD107a/b degranulation assay.
CD107a/b degranulation assay
A total of 1 × 106 T2 cells or K562-A2 cells (kindly provided by Professor Wolfgang Herr, University of Regensburg, Germany30 ) were peptide-pulsed and incubated for 2 hours in serum-free RPMI 1640. Cells were washed once and transferred to 96-well round bottom plates containing 1 × 106 expanded antigen-specific T lymphocytes in 200 µL RPMI 1640 supplemented with 10% (vol/vol) heat-inactivated HABS. Positive control wells were stimulated with 250 ng/mL phorbol 12-myristate 13-acetate (Sigma-Aldrich) and 10 µg/mL ionomycin (Sigma-Aldrich). Fluorescein isothiocyanate–conjugated anti-CD107a (H4A3) and anti-CD107b (H4B4; both from BD Biosciences) antibodies were added simultaneously to all wells. After 1 hour, monensin (BD GolgiStop, BD Biosciences) was added to all wells and the cells were incubated for 4 hours. Cells were stained with APC-conjugated anti-CD3 (SK7) and PerCP-conjugated anti-CD8 (SK1; both from BD Biosciences) antibodies for 15 minutes at RT and analyzed by flow cytometry.
IFN-γ ELISPOT assay
Freshly isolated or thawed PBMCs were resuspended in CTL medium and seeded in 24-well plates at a density of 1 × 107 cells/mL for 48 hours according to the “Restore” protocol.31 IFN-γ enzyme-linked immunosorbent spot assay (ELISPOT) assay was performed using the ELISpotPLUS for Human IFNγ Kit (Mabtech, Hamburg, Germany) according to the manufacturer’s instructions.
Peptide-pulsed and irradiated T2 cells served as stimulator cells. Positive control wells were stimulated with phorbol 12-myristate 13-acetate (250 ng/mL) and ionomycin (10 µg/mL), and negative control wells were mock stimulated with medium. Spots were counted using ImmunoSpot Series 4.0 analyzer and ImmunoSpot 4.0.16 software (CTL-Europe, Bonn, Germany).
Peripheral blood counts
For basic hematologic blood analysis, fractions of drawn whole-blood samples were analyzed using the KX-21N apparatus (Sysmex Germany, Norderstedt, Germany) used for clinical purposes as well.
Determination of hormone levels
Quantitative hormone levels for β human chorionic gonadotropin (β-hCG), estradiol, progesterone, and prolactin were measured by our central laboratory using an automated electrochemiluminescence immunoassay method.
Statistical analysis
Normal distribution was evaluated using the D’Agostino-Pearson omnibus K2 normality test. Continuous variables with normal distribution are presented as means with standard deviation and continuous variables with non-Gaussian distribution as median values with ranges. Categorical variables are presented as absolute numbers and respective percentage. Two groups with normal distribution were compared using nonpaired t tests and 2 groups with skew distribution using the Mann-Whitney U test. Fisher’s exact test was applied for evaluation of differences in frequencies between subgroups. Kruskal-Wallis 1-way analysis of variance with Dunn’s multiple comparison was performed to compare >2 subgroups. Spearman’s rank correlation test was employed for correlation analyses. P < .05 was considered significant. Statistical analyses and graphs were conducted applying Prism 5.04 software (GraphPad Software, San Diego, CA).
Results
Cross-sectional analysis in volunteer blood donors
Subject characteristics.
Between March 2010 and June 2011, 193 volunteer blood donors (118 women and 75 men) with a known A*02 HLA subtype were screened for eligibility in the cross-sectional study group I after providing written informed consent. Of these, 180 were confirmed to be HLA-A*02:01 positive. Finally, PBMCs were collected from 124 consecutively recruited donors, of whom 10 dropped out due to the quality of collected PBMCs being below the required level, leaving 114 donors in total and 38 per subgroup for final analysis as originally planned. Their characteristics are displayed in Table 1. Sample acquisition was closed in December 2011.
Characteristics of 114 HLA-A*02:01+ volunteer blood donors (cross-sectional study group I)
| . | All donors (n = 114) . | Nulligravidous women (n = 38) . | Primi-/ multiparous women* (n = 38) . | Men (n = 38) . |
|---|---|---|---|---|
| Age, y | ||||
| Median | 39 | 28 | 46 | 41 |
| Range | 21-63 | 21-53 | 28-63 | 21-56 |
| Serologic CMV status | ||||
| Positive | 33 | 10 | 14 | 9 |
| Negative | 73 | 27 | 17 | 29 |
| Not available | 8 | 1 | 7 | 0 |
| Receipt of a prior blood transfusion | ||||
| Yes | 2 | 0 | 1 | 1 |
| No | 112 | 38 | 37 | 37 |
| Number of pregnancies (women only) | ||||
| 0 | 38 | 38 | 0 | — |
| 1 | 10 | 0 | 10 | — |
| 2 | 18 | 0 | 18 | — |
| 3 | 6 | 0 | 6 | — |
| 4 | 3 | 0 | 3 | — |
| 5 | 1 | 0 | 1 | — |
| Current oral contraception (women only) | ||||
| Yes | 28 | 21 | 7 | — |
| No | 48 | 17 | 31 | — |
| Postmenopause (women only)† | ||||
| Yes | 7 | 1 | 6 | — |
| No | 69 | 37 | 32 | — |
| . | All donors (n = 114) . | Nulligravidous women (n = 38) . | Primi-/ multiparous women* (n = 38) . | Men (n = 38) . |
|---|---|---|---|---|
| Age, y | ||||
| Median | 39 | 28 | 46 | 41 |
| Range | 21-63 | 21-53 | 28-63 | 21-56 |
| Serologic CMV status | ||||
| Positive | 33 | 10 | 14 | 9 |
| Negative | 73 | 27 | 17 | 29 |
| Not available | 8 | 1 | 7 | 0 |
| Receipt of a prior blood transfusion | ||||
| Yes | 2 | 0 | 1 | 1 |
| No | 112 | 38 | 37 | 37 |
| Number of pregnancies (women only) | ||||
| 0 | 38 | 38 | 0 | — |
| 1 | 10 | 0 | 10 | — |
| 2 | 18 | 0 | 18 | — |
| 3 | 6 | 0 | 6 | — |
| 4 | 3 | 0 | 3 | — |
| 5 | 1 | 0 | 1 | — |
| Current oral contraception (women only) | ||||
| Yes | 28 | 21 | 7 | — |
| No | 48 | 17 | 31 | — |
| Postmenopause (women only)† | ||||
| Yes | 7 | 1 | 6 | — |
| No | 69 | 37 | 32 | — |
Women were not pregnant at time of blood donation.
Postmenopause was defined as last menstrual bleeding at least 12 months before study inclusion.
Immune levels and frequencies against TAAs.
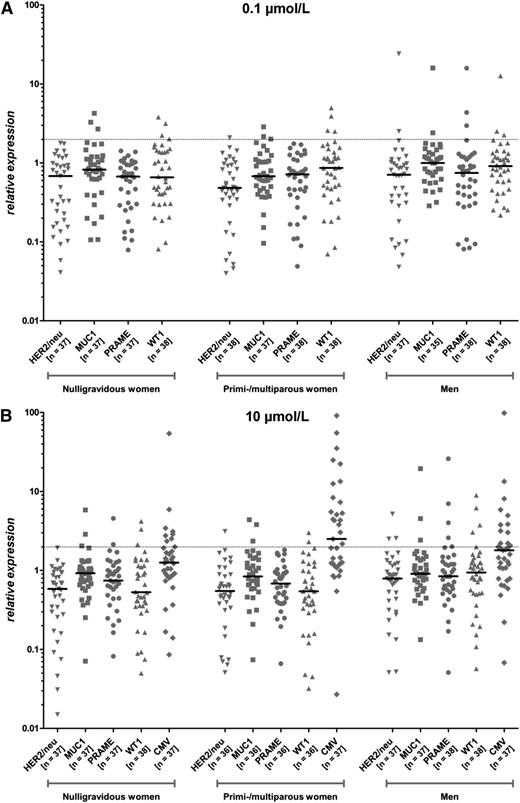
Of the analyzed 114 healthy volunteer donors 32% (n = 37; 11 nulligravidous women, 12 primi- or multiparous women, and 14 men) showed positive immune responses against at least 1 TAA including HER2/neu, MUC1, PRAME, and WT1 in their CD8+ T lymphocytes using a qRT-PCR–based IFN-γ detection assay. This included both low and high avidity immune responses as suggested by the IFN-γ production following stimulation using 2 different peptide concentrations (0.1 and 10 µmol/L). The exact frequencies in the different subgroups are displayed in Table 2, whereas individual immune levels of each donor are displayed in Figure 1. Comparing nulligravidous and primi- or multiparous women, there was no significant difference regarding the levels of immune responses. However, men showed more frequent positive and higher levels of immune responses as compared with women (Figure 1; Table 2). Using the Mann-Whitney U test, this difference in immune levels between women and men was significant for HER2/neu and WT1 solely when using 10 µmol/L peptide concentrations for stimulation as depicted in Figure 2.
Frequency of CD8+ T-cell IFN-γ immune responses against TAAs and CMV in 114 HLA-A*02:01+ volunteer blood donors (cross-sectional study group I)
| . | All donors . | Nulligravidous women . | Primi-/multiparous women . | Men . | ||||
|---|---|---|---|---|---|---|---|---|
| n . | % . | n . | % . | n . | % . | n . | % . | |
| HER2/neu | ||||||||
| 0.1 µmol/L | 3/112 | 3 | 0/37 | 0 | 1/38 | 3 | 2/37 | 5 |
| 10 µmol/L | 4/110 | 4 | 0/37 | 0 | 1/36 | 3 | 3/37 | 8 |
| 0.1 and/or 10 µmol/L | 6/114 | 5 | 0/38 | 0 | 2/38 | 5 | 4/38 | 11 |
| MUC1 | ||||||||
| 0.1 µmol/L | 8/109 | 7 | 3/37 | 8 | 3/37 | 8 | 2/35 | 6 |
| 10 µmol/L | 9/110 | 8 | 3/37 | 8 | 3/36 | 8 | 3/37 | 8 |
| 0.1 and/or 10 µmol/L | 16/114 | 14 | 6/38 | 16 | 6/38 | 16 | 4/38 | 11 |
| PRAME | ||||||||
| 0.1 µmol/L | 3/113 | 3 | 0/37 | 0 | 0/38 | 0 | 3/38 | 8 |
| 10 µmol/L | 7/111 | 6 | 2/37 | 5 | 0/36 | 0 | 5/38 | 13 |
| 0.1 and/or 10 µmol/L | 8/114 | 7 | 2/38 | 5 | 0/38 | 0 | 6/38 | 16 |
| WT1 | ||||||||
| 0.1 µmol/L | 11/114 | 10 | 4/38 | 11 | 4/38 | 11 | 3/38 | 8 |
| 10 µmol/L | 9/112 | 8 | 3/38 | 8 | 2/36 | 6 | 4/38 | 11 |
| 0.1 and/or 10 µmol/L | 17/114 | 15 | 5/38 | 13 | 6/38 | 16 | 6/38 | 16 |
| CMV | ||||||||
| 10 µmol/L | 42/111 | 38 | 8/37 | 22 | 20/37 | 54 | 14/37 | 38 |
| . | All donors . | Nulligravidous women . | Primi-/multiparous women . | Men . | ||||
|---|---|---|---|---|---|---|---|---|
| n . | % . | n . | % . | n . | % . | n . | % . | |
| HER2/neu | ||||||||
| 0.1 µmol/L | 3/112 | 3 | 0/37 | 0 | 1/38 | 3 | 2/37 | 5 |
| 10 µmol/L | 4/110 | 4 | 0/37 | 0 | 1/36 | 3 | 3/37 | 8 |
| 0.1 and/or 10 µmol/L | 6/114 | 5 | 0/38 | 0 | 2/38 | 5 | 4/38 | 11 |
| MUC1 | ||||||||
| 0.1 µmol/L | 8/109 | 7 | 3/37 | 8 | 3/37 | 8 | 2/35 | 6 |
| 10 µmol/L | 9/110 | 8 | 3/37 | 8 | 3/36 | 8 | 3/37 | 8 |
| 0.1 and/or 10 µmol/L | 16/114 | 14 | 6/38 | 16 | 6/38 | 16 | 4/38 | 11 |
| PRAME | ||||||||
| 0.1 µmol/L | 3/113 | 3 | 0/37 | 0 | 0/38 | 0 | 3/38 | 8 |
| 10 µmol/L | 7/111 | 6 | 2/37 | 5 | 0/36 | 0 | 5/38 | 13 |
| 0.1 and/or 10 µmol/L | 8/114 | 7 | 2/38 | 5 | 0/38 | 0 | 6/38 | 16 |
| WT1 | ||||||||
| 0.1 µmol/L | 11/114 | 10 | 4/38 | 11 | 4/38 | 11 | 3/38 | 8 |
| 10 µmol/L | 9/112 | 8 | 3/38 | 8 | 2/36 | 6 | 4/38 | 11 |
| 0.1 and/or 10 µmol/L | 17/114 | 15 | 5/38 | 13 | 6/38 | 16 | 6/38 | 16 |
| CMV | ||||||||
| 10 µmol/L | 42/111 | 38 | 8/37 | 22 | 20/37 | 54 | 14/37 | 38 |
Immune responses against TAAs in 114 HLA-A*02:01+ volunteer blood donors (cross-sectional study group I). CD8+ isolated T lymphocytes were coincubated with peptide-loaded irradiated T2 cells for 3 hours using 2 different peptide concentrations (0.1 and 10 µmol/L). Total RNA was isolated and qRT-PCR was performed. IFN-γ mRNA expression was normalized to CD8 mRNA levels and expressed as relative expression compared with stimulation with the irrelevant antigen gp100. (A) Peptide concentration of 0.1 µmol/L. (B) Peptide concentration of 10 µmol/L. The dashed lines indicate the threshold for positive immune responses (relative expression level of 2.0). Bars represent the median of a subgroup.
Immune responses against TAAs in 114 HLA-A*02:01+ volunteer blood donors (cross-sectional study group I). CD8+ isolated T lymphocytes were coincubated with peptide-loaded irradiated T2 cells for 3 hours using 2 different peptide concentrations (0.1 and 10 µmol/L). Total RNA was isolated and qRT-PCR was performed. IFN-γ mRNA expression was normalized to CD8 mRNA levels and expressed as relative expression compared with stimulation with the irrelevant antigen gp100. (A) Peptide concentration of 0.1 µmol/L. (B) Peptide concentration of 10 µmol/L. The dashed lines indicate the threshold for positive immune responses (relative expression level of 2.0). Bars represent the median of a subgroup.
Immune responses against HER2/neu and WT1 in 76 HLA-A*02:01+ women and 38 HLA-A*02:01+ men (cross-sectional study group I). IFN-γ mRNA expression upon antigen-specific stimulation with the TAAs HER2/neu and WT1 in nulligravidous as well as primi- or multiparous women compared with men. The dashed line indicates the threshold for positive immune responses (relative expression level of 2.0). Bars represent the median of a subgroup. Closed triangles represent women, and open triangles represent men.
Immune responses against HER2/neu and WT1 in 76 HLA-A*02:01+ women and 38 HLA-A*02:01+ men (cross-sectional study group I). IFN-γ mRNA expression upon antigen-specific stimulation with the TAAs HER2/neu and WT1 in nulligravidous as well as primi- or multiparous women compared with men. The dashed line indicates the threshold for positive immune responses (relative expression level of 2.0). Bars represent the median of a subgroup. Closed triangles represent women, and open triangles represent men.
Functional analysis of immune responses against TAAs.
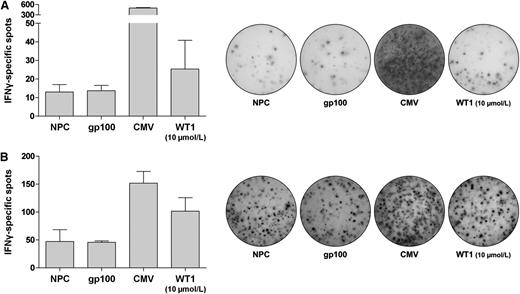
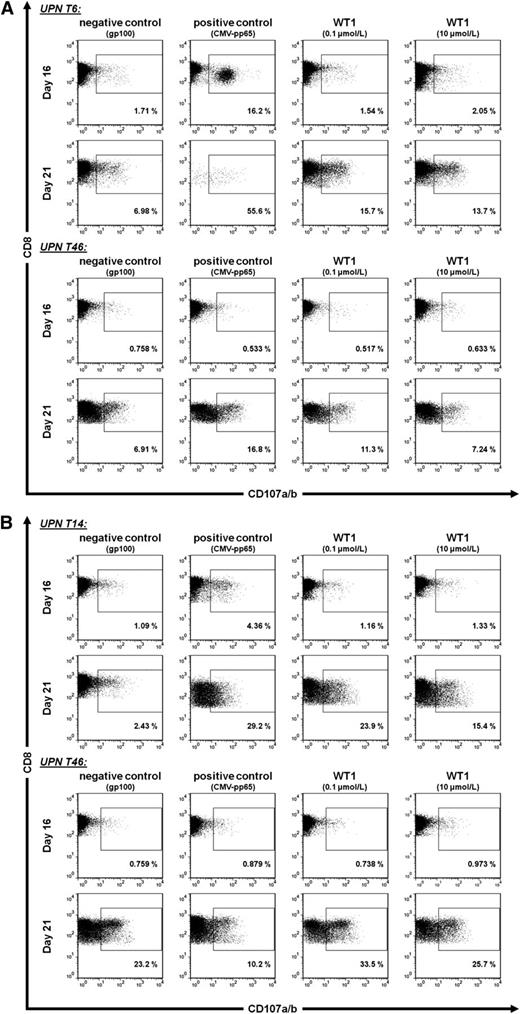
A selection of donors showing positive immune responses in the qRT-PCR-based assay were tested again using the ELISPOT technique confirming the previously described results. Two representative experiments are displayed in Figure 3. Furthermore, the ability of WT1-specific CD8+ T lymphocytes to expand in vitro upon peptide stimulation is shown in Figure 4 in 2 representative donors. CD8+ T lymphocytes were technically depicted using WT1-specific multimers for flow cytometry showing that the frequency of WT1-specfic immune responses increased from 0.034% to 0.620% after 21 days in one subject and from 0.069 to 0.741% after 16 days in another subject. These experiments reflect a 10 to 20-fold expansion of WT1-specific CD8+ T lymphocytes. Finally, the ability of donor-derived CD8+ T lymphocytes to kill WT1-positive target cells was shown against WT1-expressing leukemic K562-A2 cells and peptide-loaded T2 cells using a CD107a/b-based degranulation assay. Killing could be detected after using 0.1 and 10 µmol/L peptide concentrations, suggesting that low- and high-avidity CD8+ T lymphocytes carry the ability to lyse HLA-A*02:01–positive target cells (Figure 5).
IFN-γ ELISPOT assay results. IFN-γ ELISPOT assay was performed using a commercially available kit according to the manufacturer’s instructions. PBMCs were resuspended in CTL medium and incubated for 48 hours (“Restore” protocol). Peptide-pulsed and irradiated T2 cells served as stimulator cells. Each error bar represents the standard deviation. (A) Representative subject UPN T64. (B) Representative subject UPN T14.
IFN-γ ELISPOT assay results. IFN-γ ELISPOT assay was performed using a commercially available kit according to the manufacturer’s instructions. PBMCs were resuspended in CTL medium and incubated for 48 hours (“Restore” protocol). Peptide-pulsed and irradiated T2 cells served as stimulator cells. Each error bar represents the standard deviation. (A) Representative subject UPN T64. (B) Representative subject UPN T14.
In vitro T-cell expansion. Two batches of PBMCs from each donor were peptide-stimulated (10 µmol/L) over a course of 9 days. The first batch was analyzed on day 16 without further restimulation. The second batch was restimulated with CD3/CD28-coated beads on day 14 and analyzed on day 21. Cells were analyzed using dextramer staining on day 0 (ex vivo), day 16 (first batch), and day 21 (second batch). After gating cells with the forward and side light scatter properties of lymphocytes, dextramer-positive cells were measured as percentage of CD3/CD8-positive cells. Empty dextramer was used as negative control; CMV-pp65 was used as positive control. (A) Fluorescence-activated cell sorter (FACS) dot plots of representative female subject UPN T6. (B) FACS dot plots of representative male subject UPN T14.
In vitro T-cell expansion. Two batches of PBMCs from each donor were peptide-stimulated (10 µmol/L) over a course of 9 days. The first batch was analyzed on day 16 without further restimulation. The second batch was restimulated with CD3/CD28-coated beads on day 14 and analyzed on day 21. Cells were analyzed using dextramer staining on day 0 (ex vivo), day 16 (first batch), and day 21 (second batch). After gating cells with the forward and side light scatter properties of lymphocytes, dextramer-positive cells were measured as percentage of CD3/CD8-positive cells. Empty dextramer was used as negative control; CMV-pp65 was used as positive control. (A) Fluorescence-activated cell sorter (FACS) dot plots of representative female subject UPN T6. (B) FACS dot plots of representative male subject UPN T14.
CD107a/b-degranulation assay. PBMCs were peptide-stimulated over a course of 9 days. The first analysis was performed on day 16 without further restimulation; the second analysis was performed on day 21 after 7 days of restimulation with CD3/CD28-coated beads. After gating cells with the forward and side light scatter properties of lymphocytes, the degranulation was measured as percentage of CD107a/b-positive cells of CD3/CD8-positive cells. gp100 was used as negative control; CMV-pp65 was used as positive control. Two different cell lines were used as targets. (A) FACS dot plots of 2 representative subjects (UPN T6 and UPN T46) for T2 cells as targets. (B) FACS dot plots of 2 representative subjects (UPN T14 and UPN T46) for K562-A2 cells as targets.
CD107a/b-degranulation assay. PBMCs were peptide-stimulated over a course of 9 days. The first analysis was performed on day 16 without further restimulation; the second analysis was performed on day 21 after 7 days of restimulation with CD3/CD28-coated beads. After gating cells with the forward and side light scatter properties of lymphocytes, the degranulation was measured as percentage of CD107a/b-positive cells of CD3/CD8-positive cells. gp100 was used as negative control; CMV-pp65 was used as positive control. Two different cell lines were used as targets. (A) FACS dot plots of 2 representative subjects (UPN T6 and UPN T46) for T2 cells as targets. (B) FACS dot plots of 2 representative subjects (UPN T14 and UPN T46) for K562-A2 cells as targets.
Longitudinal analysis in first-time pregnant women
Subject characteristics.
Between March 2010 and November 2011, 93 women in their first pregnancy were screened for eligibility in the longitudinal analysis after providing written informed consent. Of these, 50 women (54%) were confirmed to be HLA-A*02:01-positive and PBMCs were collected from 47 women, 3 of whom dropped out due to a violation of inclusion criteria (1 HLA subtype was analyzed incorrectly and 2 women had already a history of a prior pregnancy). Finally, 44 HLA-A*02:01–positive first-time pregnant women participated in this prospectively planned longitudinal study group II. Their characteristics are displayed in Table 3. Acquisition of blood samples was terminated in May 2013.
Characteristics of 44 HLA-A*02:01+ women in their first pregnancy (longitudinal study group II)
| . | First to second trimester (baseline) n = 43* . | 1 to 4 d after delivery n = 34* . | 2 to 3 mo after delivery n = 34* . | After completion of nursing n = 15† . |
|---|---|---|---|---|
| Age, y | ||||
| Median | 28 | — | — | — |
| Range | 19-39 | — | — | — |
| Time point | ||||
| Median | 22 gestational weeks | 1.5 d postpartum | 54.5 d postpartum | 478 d postpartum |
| Range | 11-34 gestational weeks | 0-4 d postpartum | 43-92 d postpartum | 313-669 d postpartum |
| . | First to second trimester (baseline) n = 43* . | 1 to 4 d after delivery n = 34* . | 2 to 3 mo after delivery n = 34* . | After completion of nursing n = 15† . |
|---|---|---|---|---|
| Age, y | ||||
| Median | 28 | — | — | — |
| Range | 19-39 | — | — | — |
| Time point | ||||
| Median | 22 gestational weeks | 1.5 d postpartum | 54.5 d postpartum | 478 d postpartum |
| Range | 11-34 gestational weeks | 0-4 d postpartum | 43-92 d postpartum | 313-669 d postpartum |
A total of 44 women participated in this longitudinal study. None of the women received blood transfusions during the course of the study.
Blood samples could not be drawn at each time point due to various reasons (loss of follow-up or contact, refusal).
After the ethical amendment, blood could be drawn in 15 women at an additional time point after completion of nursing.
Immune levels and frequencies against TAAs.
The course of CD8-mediated immune levels against the TAAs HER2/neu, MUC1, PRAME, and WT1 as measured by IFN-γ qRT-PCR after peptide stimulation is depicted in Figure 6. Here, it is shown that medians of immune responses against the different TAAs decreased over time. The highest levels were found at the first time point (first to second trimester) declining after delivery and reaching the lowest levels after completion of nursing (Figure 6). Using the 1-way analysis of variance, differences in immune responses against HER2/neu and WT1 were found to be significantly different between the first and the last time points (Figure 6). Looking at frequencies of positive immune responses against TAAs in this longitudinal analysis, this general decline over time could be confirmed for MUC1, PRAME, and WT1, but not for HER2/neu, where positive responses were rare (Table 4). For MUC1, PRAME, and WT1, the highest frequencies were found in the first to second trimester, declining after delivery and disappearing after completion of nursing (Table 4).
Immune responses against TAAs in 44 HLA-A*02:01+ women in their first pregnancy (longitudinal study group II). (A) Peptide concentration of 0.1 µmol/L. (B) Peptide concentration of 10 µmol/L. The dashed lines indicate the threshold for positive immune responses (relative expression level of 2.0). Bars represent the median of a subgroup.
Immune responses against TAAs in 44 HLA-A*02:01+ women in their first pregnancy (longitudinal study group II). (A) Peptide concentration of 0.1 µmol/L. (B) Peptide concentration of 10 µmol/L. The dashed lines indicate the threshold for positive immune responses (relative expression level of 2.0). Bars represent the median of a subgroup.
Frequency of CD8+ T-cell IFN-γ immune responses against TAAs and CMV in 44 HLA-A*02:01+ women in their first pregnancy (longitudinal study group II)
| . | First to second trimester . | 1 to 4 d after delivery . | 2 to 3 mo after delivery . | After completion of nursing . | ||||
|---|---|---|---|---|---|---|---|---|
| n . | % . | n . | % . | n . | % . | n . | % . | |
| HER2/neu | ||||||||
| 0.1 µmol/L | 0/39 | 0 | 1/31 | 3 | 0/34 | 0 | 1/13 | 8 |
| 10 µmol/L | 0/36 | 0 | 0/24 | 0 | 0/26 | 0 | 0/13 | 0 |
| 0.1 and/or 10 µmol/L | 0/43 | 0 | 1/31 | 3 | 0/34 | 0 | 1/14 | 7 |
| MUC1 | ||||||||
| 0.1 µmol/L | 4/36 | 11 | 2/31 | 6 | 1/34 | 3 | 0/11 | 0 |
| 10 µmol/L | 2/32 | 5 | 0/20 | 0 | 0/24 | 0 | 0/11 | 0 |
| 0.1 and/or 10 µmol/L | 6/43 | 14 | 2/31 | 6 | 1/34 | 3 | 0/12 | 0 |
| PRAME | ||||||||
| 0.1 µmol/L | 2/37 | 5 | 1/31 | 3 | 2/33 | 6 | 0/12 | 0 |
| 10 µmol/L | 1/33 | 3 | 2/20 | 10 | 1/25 | 3 | 0/13 | 0 |
| 0.1 and/or 10 µmol/L | 3/43 | 7 | 2/31 | 6 | 2/33 | 6 | 0/13 | 0 |
| WT1 | ||||||||
| 0.1 µmol/L | 11/41 | 27 | 3/31 | 10 | 1/34 | 3 | 0/14 | 0 |
| 10 µmol/L | 7/39 | 17 | 1/29 | 3 | 0/32 | 0 | 0/14 | 0 |
| 0.1 and/or 10 µmol/L | 13/43 | 30 | 3/31 | 10 | 1/34 | 3 | 0/14 | 0 |
| CMV | ||||||||
| 10 µmol/L | 12/23 | 52 | 6/21 | 29 | 15/30 | 50 | 8/11 | 73 |
| . | First to second trimester . | 1 to 4 d after delivery . | 2 to 3 mo after delivery . | After completion of nursing . | ||||
|---|---|---|---|---|---|---|---|---|
| n . | % . | n . | % . | n . | % . | n . | % . | |
| HER2/neu | ||||||||
| 0.1 µmol/L | 0/39 | 0 | 1/31 | 3 | 0/34 | 0 | 1/13 | 8 |
| 10 µmol/L | 0/36 | 0 | 0/24 | 0 | 0/26 | 0 | 0/13 | 0 |
| 0.1 and/or 10 µmol/L | 0/43 | 0 | 1/31 | 3 | 0/34 | 0 | 1/14 | 7 |
| MUC1 | ||||||||
| 0.1 µmol/L | 4/36 | 11 | 2/31 | 6 | 1/34 | 3 | 0/11 | 0 |
| 10 µmol/L | 2/32 | 5 | 0/20 | 0 | 0/24 | 0 | 0/11 | 0 |
| 0.1 and/or 10 µmol/L | 6/43 | 14 | 2/31 | 6 | 1/34 | 3 | 0/12 | 0 |
| PRAME | ||||||||
| 0.1 µmol/L | 2/37 | 5 | 1/31 | 3 | 2/33 | 6 | 0/12 | 0 |
| 10 µmol/L | 1/33 | 3 | 2/20 | 10 | 1/25 | 3 | 0/13 | 0 |
| 0.1 and/or 10 µmol/L | 3/43 | 7 | 2/31 | 6 | 2/33 | 6 | 0/13 | 0 |
| WT1 | ||||||||
| 0.1 µmol/L | 11/41 | 27 | 3/31 | 10 | 1/34 | 3 | 0/14 | 0 |
| 10 µmol/L | 7/39 | 17 | 1/29 | 3 | 0/32 | 0 | 0/14 | 0 |
| 0.1 and/or 10 µmol/L | 13/43 | 30 | 3/31 | 10 | 1/34 | 3 | 0/14 | 0 |
| CMV | ||||||||
| 10 µmol/L | 12/23 | 52 | 6/21 | 29 | 15/30 | 50 | 8/11 | 73 |
This decline in immune responses against TAAs could not be observed for cytomegalovirus (CMV), which was used as a positive control (Figure 6). As expected, pregnancy-induced leukocytosis was primarily a consequence of an increase in neutrophil granulocytes (Table 5), reaching the maximum shortly after delivery and declining further on while absolute lymphocyte counts remained stable. In Table 6, hormonal levels including β-hCG, estradiol, progesterone, and prolactin are displayed, reflecting the expected course over time and being consistent with an intact pregnancy.
Blood parameters of 44 HLA-A*02:01+ women in their first pregnancy (longitudinal study group II)
| . | First to second trimester (n = 8) . | 1 to 4 d after delivery (n = 16) . | 2 to 3 mo after delivery (n = 27) . | After completion of nursing (n = 15) . |
|---|---|---|---|---|
| RBC (×106/µL) | 3.9 ± 0.4 | 3.6 ± 0.5 | 4.5 ± 0.2 | 5.3 ± 0.7 |
| Hemoglobin (g/dL) | 11.8 ± 0.8 | 10.3 ± 1.6 | 12.3 ± 0.9 | 15.0 ± 2.2 |
| WBC (×103/µL) | 9.3 ± 2.9 | 12.9 ± 3.0 | 6.0 ± 1.1 | 6.1 ± 1.3 |
| ALC (×103/µL) | 1.7 ± 0.5 | 2.0 ± 0.6 | 2.1 ± 0.3 | 2.2 ± 0.6 |
| ANC (×103/µL) | 7.0 ± 2.3 | 10.1 ± 2.5 | 3.4 ± 0.9 | 3.5 ± 1.1 |
| Platelets (×103/µL) | 240 ± 57 | 232 ± 53 | 283 ± 60 | 231 ± 67 |
| . | First to second trimester (n = 8) . | 1 to 4 d after delivery (n = 16) . | 2 to 3 mo after delivery (n = 27) . | After completion of nursing (n = 15) . |
|---|---|---|---|---|
| RBC (×106/µL) | 3.9 ± 0.4 | 3.6 ± 0.5 | 4.5 ± 0.2 | 5.3 ± 0.7 |
| Hemoglobin (g/dL) | 11.8 ± 0.8 | 10.3 ± 1.6 | 12.3 ± 0.9 | 15.0 ± 2.2 |
| WBC (×103/µL) | 9.3 ± 2.9 | 12.9 ± 3.0 | 6.0 ± 1.1 | 6.1 ± 1.3 |
| ALC (×103/µL) | 1.7 ± 0.5 | 2.0 ± 0.6 | 2.1 ± 0.3 | 2.2 ± 0.6 |
| ANC (×103/µL) | 7.0 ± 2.3 | 10.1 ± 2.5 | 3.4 ± 0.9 | 3.5 ± 1.1 |
| Platelets (×103/µL) | 240 ± 57 | 232 ± 53 | 283 ± 60 | 231 ± 67 |
ALC, absolute lymphocyte count; ANC, absolute neutrophil count; RBC, red blood cell count; WBC, white blood cell count.
Hormone levels of 44 HLA-A*02:01+ women in their first pregnancy (longitudinal study group II)
| . | First to second trimester (n = 43) . | 1 to 4 d after delivery (n = 34) . | 2 to 3 mo after delivery (n = 34) . | After completion of nursing (n = 15) . |
|---|---|---|---|---|
| β-hCG (mU/mL) | ||||
| Median | 17 477 | 2116 | 0.10 | — |
| Range | 1202-103 863 | 78-46 187 | 0.10-2.8 | — |
| Estradiol (pg/mL) | ||||
| Median | 9343 | 191 | 29 | 29 |
| Range | 1269-25 770 | 38-5464 | 5.0-302 | 5.0-234 |
| Progesterone (ng/mL) | ||||
| Median | 57 | 7.8 | 0.26 | 0.56 |
| Range | 12-605 | 0.90-91 | 0.09-8.9 | 0.09-20 |
| Prolactin (ng/mL) | ||||
| Median | 125 | 255 | 30 | 7.8 |
| Range | 0.50-272 | 51-470 | 1.8-167 | 5.0-23 |
| . | First to second trimester (n = 43) . | 1 to 4 d after delivery (n = 34) . | 2 to 3 mo after delivery (n = 34) . | After completion of nursing (n = 15) . |
|---|---|---|---|---|
| β-hCG (mU/mL) | ||||
| Median | 17 477 | 2116 | 0.10 | — |
| Range | 1202-103 863 | 78-46 187 | 0.10-2.8 | — |
| Estradiol (pg/mL) | ||||
| Median | 9343 | 191 | 29 | 29 |
| Range | 1269-25 770 | 38-5464 | 5.0-302 | 5.0-234 |
| Progesterone (ng/mL) | ||||
| Median | 57 | 7.8 | 0.26 | 0.56 |
| Range | 12-605 | 0.90-91 | 0.09-8.9 | 0.09-20 |
| Prolactin (ng/mL) | ||||
| Median | 125 | 255 | 30 | 7.8 |
| Range | 0.50-272 | 51-470 | 1.8-167 | 5.0-23 |
Association of TAA- and CMV-specific immune responses
There was no correlation of CD8-mediated immune responses against CMV and TAAs during and after pregnancy (Figure 6 and Table 7). However, there was a borderline significant correlation between immune responses against CMV and HER2/neu as well as MUC1 in volunteer blood donors (Table 7), whereas there was no correlation with PRAME or WT1.
Correlation analysis between relative CD8+ T-cell IFN-γ immune responses against TAAs and CMV in HLA-A*02:01+ volunteer blood donors and women in their first pregnancy
| . | HER2/neu . | MUC1 . | PRAME . | WT1 . | ||||
|---|---|---|---|---|---|---|---|---|
| n . | r . | n . | r . | n . | r . | n . | r . | |
| Cross-sectional study group I | ||||||||
| All donors | 107 | 0.203* | 107 | 0.225* | 108 | 0.168 | 109 | 0.149 |
| Nulligravidous women | 36 | 0.023 | 36 | 0.252 | 36 | 0.216 | 37 | 0.034 |
| Primi-/multiparous women | 35 | 0.180 | 35 | 0.045 | 35 | 0.016 | 35 | 0.078 |
| Men | 36 | 0.347* | 36 | 0.292 | 37 | 0.205 | 37 | 0.305 |
| Longitudinal study group II | ||||||||
| First to second trimester | 18 | −0.015 | 16 | −0.124 | 17 | 0.033 | 19 | −0.056 |
| 1 to 4 d after delivery | 19 | 0.059 | 16 | 0.225 | 16 | 0.034 | 21 | 0.056 |
| 2 to 3 mo after delivery | 17 | 0.296 | 16 | 0.353 | 17 | 0.048 | 22 | 0.211 |
| After completion of nursing | 11 | −0.309 | 10 | −0.273 | 11 | −0.009 | 11 | 0.355 |
| . | HER2/neu . | MUC1 . | PRAME . | WT1 . | ||||
|---|---|---|---|---|---|---|---|---|
| n . | r . | n . | r . | n . | r . | n . | r . | |
| Cross-sectional study group I | ||||||||
| All donors | 107 | 0.203* | 107 | 0.225* | 108 | 0.168 | 109 | 0.149 |
| Nulligravidous women | 36 | 0.023 | 36 | 0.252 | 36 | 0.216 | 37 | 0.034 |
| Primi-/multiparous women | 35 | 0.180 | 35 | 0.045 | 35 | 0.016 | 35 | 0.078 |
| Men | 36 | 0.347* | 36 | 0.292 | 37 | 0.205 | 37 | 0.305 |
| Longitudinal study group II | ||||||||
| First to second trimester | 18 | −0.015 | 16 | −0.124 | 17 | 0.033 | 19 | −0.056 |
| 1 to 4 d after delivery | 19 | 0.059 | 16 | 0.225 | 16 | 0.034 | 21 | 0.056 |
| 2 to 3 mo after delivery | 17 | 0.296 | 16 | 0.353 | 17 | 0.048 | 22 | 0.211 |
| After completion of nursing | 11 | −0.309 | 10 | −0.273 | 11 | −0.009 | 11 | 0.355 |
Peptide concentration for stimulation was 10 µmol/L for TAAs and CMV.
r, Spearman’s rank correlation coefficient of relative immune responses; n, number of individuals for whom the correlation between CMV and respective TAA was performed (this number varied, as results for both antigens needed to be available for each individual).
P < .05.
Discussion
Harnessing the allograft’s immunity against leukemia offers a unique mechanism to provide cure to an otherwise lethal disease. Although nonrelapse mortality rates in allogeneic hematopoietic stem cell transplantation (HSCT) have declined steadily over time, relapse rates remain consistently high.32,33 Thus, current research in allogeneic HSCT focuses on the enhancement of GVL effects to optimize disease control.32,34 However, the appearance of severe GVHD requiring immediate immunosuppression regularly compromises these beneficial effects of the allograft.35,36 Consequently, several immunotherapeutic approaches nowadays focus on TAAs as target antigens to mount antileukemic immune responses in the absence of GVHD.34,37 Although it is well accepted that TAA-specific immune responses play a central role in overall GVL,10,38-40 little is known about their origin and ability to persist as functionally active immune cells in the host preventing relapse.
Several groups have shown that patients with hematologic malignancies harbor increased frequencies of TAA-specific immune responses.11,36-42 So far, the presence of these immune responses in healthy individuals could be only demonstrated in cohorts of limited size.11,39 The current study represents, to the best of our knowledge, the first comprehensive work to study the exact frequencies of T-lymphocyte responses against clinically relevant TAAs in a large group of healthy individuals. Here, we could show that one-third of volunteer donors do carry significant immune responses against at least 1 of the studied TAAs. In our study, immune responses were measured directly following a single course of antigen presentation without prior expansion, intending to recruit memory rather than naive responses. Frequencies varied for different TAAs. Against WT1, 15% of the volunteer donors had low- and/or high-avidity immune responses, which is consistent with the original observation in a much smaller cohort.12,41 Similar frequencies were found for MUC1, whereas frequencies against HER2/neu and PRAME were lower. Interestingly, Weber et al were able to detect WT1-specific immune responses in 9 out of a total of 10 healthy donors following multiple rounds of stimulation, suggesting that upon professional and repetitive antigen presentation under the condition of optimal cytokine support, WT1-specific immune responses could be generated from virtually everyone, opening opportunities for immunotherapy.42
For patients with leukemia, it is well known that the high-level expression of TAAs in the malignant tissue facilitates autoimmune reactions mounting in frequencies of 60% and higher as described for patients with WT1-overexpressing acute myeloid leukemias and myelodysplastic syndrome.41,43 Thus, we hypothesized that due to the well-described overexpression of TAAs in placental and fetal tissues, prior pregnancy and the resultant fetomaternal transfer during delivery could have an influence on the generation of long-lasting TAA-specific immune responses in women, as it is known for Y-chromosomal responses in women with male infants.21-24,44 Interestingly, women with prior pregnancy did not have higher frequencies or higher levels of immune responses against 1 of the 4 studied TAAs. These results could be confirmed by the longitudinal analysis performed in the second study group of women with no known history of prior pregnancy. These intraindividual longitudinal courses showed that immune responses were gained in the first 2 trimesters of pregnancy, declined after delivery, and fully lost after completion of nursing. Most likely, the gain of immune responses in early pregnancy is induced by the growth of the fetoplacental unit expressing high levels of TAAs,45 whereas abrogation of the immune response is probably a consequence of the loss of the target antigen after delivery and the continuing immunosuppressive hormonal influence during pregnancy by estrogens.46,47 This steady decline in immune responses against TAAs could not be observed for CMV used as a positive control, suggesting that the observed pattern was specific and independent of the general immune environment. Looking at the blood counts of a representative group of these women in the course of and after pregnancy, the observed trend in TAA-specific immune responses was not accountable to an overall decline in absolute numbers of lymphocytes that stayed stable over time, consistent with physiological conditions of pregnancy.48
Interestingly, men showed a general tendency toward higher frequencies and higher levels of immune responses to TAAs, particularly to HER2/neu and WT1, where the differences between the genders reached statistical significance. Based on the experience from leukemic patients and women at early pregnancy, the appearance of high frequencies of TAA-specific immune responses is most likely associated with tissues overexpressing antigens such as WT1 and HER2/neu.21,41,44,49,50 Thus, a continuous gonadal presence of cancer-testis-antigen–expressing tissues not compromised by an immunosuppressive hormonal environment remains as the likely driving force behind this immunity against TAAs in men.51-53
In volunteer blood donors, responses against TAAs were poorly correlated with those against CMV, reaching only borderline significance for HER2/neu and MUC1, whereas there was no association in pregnant women. In light of the multiple correlations performed, this suggests that a potential cross-reactivity between immune responses against CMV and TAAs appears to be rather unlikely but cannot be fully ruled out.
Taken together, memory-type immune responses against HER2/neu, MUC1, PRAME, and/or WT1 are generally present in one-third of healthy individuals. However, providing the optimal immunologic milieu and repetitive antigen stimulation may allow the exertion of TAA-specific autoimmunity in the majority of healthy individuals as shown for WT1.42 These low- and high-avidity immune cells have the capacity to expand and exert killing functions on leukemic cells as shown in vitro and in animal models postvaccination.12,54,55 The exploitation of donor-derived autoimmunity against selected TAAs by improving donor selection and facilitating adoptive immunotransfer of donor-derived T lymphocytes may significantly contribute to the control of the malignant disease in the absence of GVHD after allotransplantation, where an optimal environment offers unique opportunities for homeostatic expansion.11,56 The presence of the target antigen represents an essential condition for the persistence of the TAA-specific immune responses, as suggested by the studies in the course of pregnancy. Thus, vaccination strategies may avoid their abrogation in the allogeneic recipient.57 Additional depletion of regulatory T lymphocytes, application of immunomodulatory agents such as lenalidomide and the reduction of immunosuppression in the context of selective depletion strategies could antagonize a permissive immune environment particularly enhancing the effects of T lymphocytes of lower avidity against TAAs.58-64 Furthermore, these unique effects may be also facilitated after autologous HSCT, providing a strong antimalignant autoimmune effect on top of high-dose chemotherapy.65 Finally, this study provides novel insights in the regulation of TAA-specific immunity in healthy individuals, best exemplified by the results from pregnancy and in men. Whether increased immune responses in healthy donors as they are found in men generally contribute to an improved TAA-specific immune reconstitution and clinical outcome in allogeneic recipients remains open and should be addressed in clinical trials.
Presented in part at the annual meetings of the Association for Cancer Immunotherapy (Mainz, Germany, May 25-27, 2011) and the American Society for Hematology (Atlanta, GA, December 8-11, 2012 and New Orleans, LA, December 7-10, 2013).66-68
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the subjects for their participation in the study; Dr Silvia Hobert, Professor Jael Backe, Dr Helmut Spingler, Renate Vieth-Laßmann, Dr Martin Witteler, and their assistants as well as Marianne Ahmed for the recruitment of pregnant women; Professor Markus Böck, Dr Sabine Kuhn, Dr Evelyn Putz, and the staff of the Institute of Clinical Transfusion Medicine and Hemotherapy for the recruitment of platelet donors; Monika Koospal and Anita Pietschmann for technical assistance; and Dr Uwe Mäder for statistical assistance. The authors also thank Dr Judy Mielke for critical reading of the manuscript.
This work was supported by grants from the Interdisciplinary Center for Clinical Research (IZKF) of the University of Würzburg, Germany (D-150); “Hilfe im Kampf gegen Krebs e.V.,” Würzburg, Germany (M.L.); and “Deutscher Akademischer Austausch Dienst e.V.,” Bonn, Germany (A.W.).
Authorship
Contribution: M.L., A.W., and M.A. collected samples, performed experiments, analyzed data, and wrote the paper; S.G. and L.B. collected samples and performed experiments; M.S., S.O., H.E., and U.K. provided administrative support; P.H. performed statistical analysis; E.K. provided administrative support; C.O. and S.M. designed the study, analyzed data, and wrote the paper; and all authors critically revised the manuscript for important intellectual content and approved the manuscript to be published.
The current affiliation for A.W. is the Department of Genetic Medicine, Weill Cornell Medical College in Qatar, Doha, Qatar.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Stephan Mielke, Allogeneic Stem Cell Transplantation Program, Department of Internal Medicine II, Hematology and Oncology, Würzburg University Medical Center, Oberdürrbacher Strasse 6, D-97080 Würzburg, Germany; e-mail: mielke_s@ukw.de.
References
Author notes
M.L. and A.W. contributed equally to this study.
C.O. and S.M. contributed equally to this study.