Key Points
Allogeneic BMT into newborn MPS I mice allows high donor-derived hematopoietic engraftment and prevents bone deformities.
Bones of transplanted MPS I mice show significant improvements at radiographic, microcomputed tomography, and histological analyses.
Abstract
Neonatal bone marrow transplantation (BMT) could offer a novel therapeutic opportunity for genetic disorders by providing sustainable levels of the missing protein at birth, thus preventing tissue damage. We tested this concept in mucopolysaccharidosis type I (MPS IH; Hurler syndrome), a lysosomal storage disorder caused by deficiency of α-l-iduronidase. MPS IH is characterized by a broad spectrum of clinical manifestations, including severe progressive skeletal abnormalities. Although BMT increases the life span of patients with MPS IH, musculoskeletal manifestations are only minimally responsive if the timing of BMT delays, suggesting already irreversible bone damage. In this study, we tested the hypothesis that transplanting normal BM into newborn MPS I mice soon after birth can prevent skeletal dysplasia. We observed that neonatal BMT was effective at restoring α-l-iduronidase activity and clearing elevated glycosaminoglycans in blood and multiple organs. At 37 weeks of age, we observed an almost complete normalization of all bone tissue parameters, using radiographic, microcomputed tomography, biochemical, and histological analyses. Overall, the magnitude of improvements correlated with the extent of hematopoietic engraftment. We conclude that BMT at a very early stage in life markedly reduces signs and symptoms of MPS I before they appear.
Introduction
Bone marrow transplantation (BMT) is an efficacious therapeutic modality for a number of nonmalignant conditions, both acquired and genetically determined. In the treatment of genetic disorders, the hematopoiesis transplanted from a healthy allogeneic donor can produce the missing protein at levels sufficient to correct the underlying abnormalities. However, the current clinical experience is only partially successful. One of the reasons for this could be the limited efficacy of the protein provided through the hematopoietic cell secretome. Alternatively, the time at which BMT is currently performed could be too late to prevent organ damage.
This fundamental question is well exemplified by the case of mucopolysaccharidosis type I-Hurler syndrome (MPS IH), a lysosomal storage disease in which allogeneic BMT, although considered first-line treatment, has a limited effect on the skeletal abnormalities. In patients with MPS IH, the intracellular accumulation of glycosaminoglycans (GAGs), dermatan sulfate, and heparan sulfate (HS) disrupts normal cell functions and gives rise to progressive multiorgan morbidity, which is typical for the disease.1,2 The array of musculoskeletal abnormalities seen in Hurler syndrome is known as dysostosis multiplex,3-6 consisting of abnormally shaped vertebrae and ribs, enlarged skull, spatulate ribs, hypoplastic epiphyses, thickened diaphyses, bullet-shaped metacarpals, hip dysplasia, genu valgum, and spinal cord compression.7 Unfortunately, despite successful engraftment of normal donor hematopoietic stem cells that ameliorate multiorgan morbidity, the musculoskeletal manifestations still deteriorate and affect the quality of life in most transplanted patients with MPS IH.8 This is presumably a result of the limited penetration of the expressed α-l-iduronidase (IDUA) enzyme into musculoskeletal tissues.4 Although substantial clinical improvements of joint mobility, coarse facial features, and claw hands were reported after transplantation,9 with age, clinical and radiographic musculoskeletal abnormalities still developed. The incomplete correction of the skeletal phenotype produced by BMT may also be because bone abnormalities are irreversible at the time of the transplant (median age at BMT, 16 months). However, during prenatal and perinatal life, infants with Hurler syndrome have a nearly normal skeletal development, probably because of placental protection.10,11
Therefore, we hypothesize that the first months of life represent the best window of opportunity for preventing bone deformities in Hurler children. Consistent with this hypothesis, a retrospective analysis demonstrated a superior long-term clinical outcome of Hurler patients when BMT was performed early in life.12 In the same direction, recent implementation of newborn screening programs for patients with MPS IH may offer an opportunity to consider BMT in the first months of life.13-15
A few studies have evaluated whether perinatal infusion of hematopoietic stem cells could ameliorate the most critical features in MPS animal models.16-18 To date, neonatal BMT (nBMT) has never been tested in MPS I mice. The mouse model of MPS I was produced through the disruption of the IDUA gene19 and presents skeletal abnormalities similar to those seen in patients with MPS IH, providing a valuable tool for the study of disease pathogenesis. MPS I mice develop extensive dysostosis detectable using histopathologic, radiographic, and microcomputed tomography (micro-CT) analyses at a later stage of life.19-21 BMT has previously been tested in adult MPS I mice preconditioned with irradiation, providing only a partial benefit on skeletal abnormalities.22
In the present study, we have evaluated whether neonatal transplantation of syngeneic BM from wild type (WT) donors could rescue the severe skeletal phenotype in the mouse model of MPS I, using clinical, biochemical, radiographic, and pathological analyses.
Materials and methods
Mouse model
The MPS I mouse model (Idua−/−mice, C57BL/6 background)19 was purchased from the Jackson Laboratory (Bar Harbor, ME). A breeding colony was established from heterozygous mating pairs, and genotyping was performed on tail clip DNA, as described.19 Pregnant dams obtained from the colony (Charles River, Calco, Italy) were housed in the animal facility of the University of Milano-Bicocca. Procedures involving animal handling and care conform to institutional guidelines, in compliance with national laws and policies.
BMT
nBMT was performed as reported.23 Briefly, 1- to 2-day-old pups (Ly5.2 [CD45.2] MPS I or Ly5.2 WT mice) were treated with a single intraperitoneal injection of busulfan (20 mg/kg; Busilvex, Pierre Fabre, Boulogne, France). Eight- to 12-week-old C57BL/6-Ly5.1 (CD45.1) WT donor mice (Charles River) were killed with CO2, and the BM was harvested by flushing femurs and tibiae. Newborn mice were transplanted 24 hours after busulfan administration by intravenous (via temporal vein) injection of 2 × 106 donor BM cells. At 37 weeks of age, tissues from recipient killed mice were harvested and preserved for analyses, as specified here and in the supplemental Methods available on the Blood Web site.
IDUA and β-hexosaminidase activity assay
Analysis of GAGs in tissues and plasma
Histopathology
For the evaluation of long bone morphology, the hind limbs were decalcified in EDTA (Sigma-Aldrich) for 3 weeks and longitudinally embedded in paraffin. Four μm sections were deparaffinized, rehydrated, and stained with hematoxylin/eosin by standard procedures.
For evaluation of growth plate by light microscopy, bone was decalcified and toluidine blue-stained 0.5 μm sections were examined.
Statistical analysis
The distribution of continuous variables was contrasted in groups by the nonparametric test on equality of the medians (Wilcoxon). All tests were at 5% significance level and on a 2-sided alternative, with the exception of those on the micro-CT data where a 1-sided alternative was considered. The relation between engraftment and treatment in the MPS I BMT group was assessed by Pearson’s correlation coefficient and relative P-value for absence of correlation. See the supplemental Methods for details.
Results
Donor hematopoietic engraftment in MPS I mice after nBMT
After conditioning with busulfan, 2- to 3-day-old WT CD45.2+ and MPS I CD45.2+ mice were transplanted with BM cells derived from adult CD45.1+ WT mice (Figure 1A). We compared the engraftment levels of the transplanted groups, consisting of WT recipients (hereafter named WT nBMT; n = 8 mice [3 males, 5 females]) and MPS I recipients (hereafter named MPS I nBMT; n = 14 mice [7 males, 7 females]). Quantification of CD45.1+ donor-derived cells in peripheral blood (PB) revealed no significant differences between the 2 groups of mice at 4 weeks posttransplant (median WT nBMT, 54.72% [range, 22.18% to 87.23%] vs median MPS I nBMT, 59.18% [range, 0.93% to 86.34%]; P = .609). Both transplanted groups maintained stable engraftment levels until euthanasia at 37 weeks of age (PB, median WT nBMT 67.45% [range, 16.00% to 95.86%] vs median MPS I nBMT, 81.30% [range, 0.80% to 95.80%]; P = .714; spleen, median WT nBMT, 83.95% [range, 53.30% to 97.50%] vs median MPS I nBMT, 64.10% [range, 1.37% to 98.30%]; P = .304) (Figure 1B). Among transplanted mice, 13 (8 MPS I nBMT and 5 WT nBMT) of 22 mice presented a high hematopoietic chimerism, defined as more than 50% donor CD45.1+ cells in PB (median, 92.60%' range, 54.70% to 95.86% CD45.1+). Hence, we included this subgroup of highly engrafted mice (hereafter named MPS I nBMT-hi) in all studies reported. The remaining transplanted mice showed an engraftment level of less than 50% of CD45.1+ within PB cells (median, 16.00%; range, 0.80% to 46.40% CD45.1+). In both WT nBMT and MPS I nBMT mice, similar engraftment levels were also observed in hematopoietic organs, such as spleen and thymus (Figure 1C), in which we could also appreciate a comparable presence of myeloid (CD11b, Gr-1), B (CD45R), and T (CD3) lymphoid cells, indicating multilineage donor-derived engraftment (Figure 1C).
Donor hematopoietic engraftment into newborn transplanted MPS I mice. (A) Experimental scheme. Newborn WT and MPS I (CD45.2) mice were conditioned with busulfan (20 mg/kg) on day 1 to 2 after birth and transplanted with 2 × 106 adult BM nucleated cells (CD45.1) on the next day, as indicated. Groups were WT untreated (WT), MPS I untreated (MPS I), MPS I mice transplanted with CD45.1 donor BM cells (MPS I nBMT), and WT mice transplanted with CD45.1 donor BM cells (WT nBMT). Chimerism was determined at 4 weeks of age, and at 37 weeks of age, mice were killed for detection of long-term engraftment, biochemical, radiographic, and histological analyses. (B) Long-term donor chimerism (engraftment of CD45.1+ cells) was determined using flow cytometry in PB and spleen at 37 weeks of age. Upper horizontal line of box represents the 75th percentile, the lower horizontal line of box represents the 25th percentile, the horizontal bar within the box represents the median, the square within box represents the mean, and vertical lines outside the box represent the minimum and maximum. P value was calculated using Wilcoxon nonparametric unpaired test, 2 sides. (C) Representative multilineage donor-derived reconstitution was analyzed, using flow cytometry in spleen (macrophages [MAC], granulocytes [GRAN], B and T lymphoid cells) and thymus (T lymphoid cells) of recipient WT nBMT and MPS I nBMT mice.
Donor hematopoietic engraftment into newborn transplanted MPS I mice. (A) Experimental scheme. Newborn WT and MPS I (CD45.2) mice were conditioned with busulfan (20 mg/kg) on day 1 to 2 after birth and transplanted with 2 × 106 adult BM nucleated cells (CD45.1) on the next day, as indicated. Groups were WT untreated (WT), MPS I untreated (MPS I), MPS I mice transplanted with CD45.1 donor BM cells (MPS I nBMT), and WT mice transplanted with CD45.1 donor BM cells (WT nBMT). Chimerism was determined at 4 weeks of age, and at 37 weeks of age, mice were killed for detection of long-term engraftment, biochemical, radiographic, and histological analyses. (B) Long-term donor chimerism (engraftment of CD45.1+ cells) was determined using flow cytometry in PB and spleen at 37 weeks of age. Upper horizontal line of box represents the 75th percentile, the lower horizontal line of box represents the 25th percentile, the horizontal bar within the box represents the median, the square within box represents the mean, and vertical lines outside the box represent the minimum and maximum. P value was calculated using Wilcoxon nonparametric unpaired test, 2 sides. (C) Representative multilineage donor-derived reconstitution was analyzed, using flow cytometry in spleen (macrophages [MAC], granulocytes [GRAN], B and T lymphoid cells) and thymus (T lymphoid cells) of recipient WT nBMT and MPS I nBMT mice.
At 37 weeks, the median body weight of nontransplanted MPS I mice was similar to that of age-matched WT mice (median MPS I, 33.32 g [range, 18.70 to 37.90 g] vs median WT, 34.68 g [range, 21.84 to 36.46 g]; P = .534). Because of busulfan toxicity, the body weight of transplanted MPS I nBMT mice (median, 21.30 g; range, 16.40 to 40.30 g) and WT nBMT mice (median, 23.55 g; range, 16.77 to 34.35 g) was lower compared with nontransplanted WT mice.
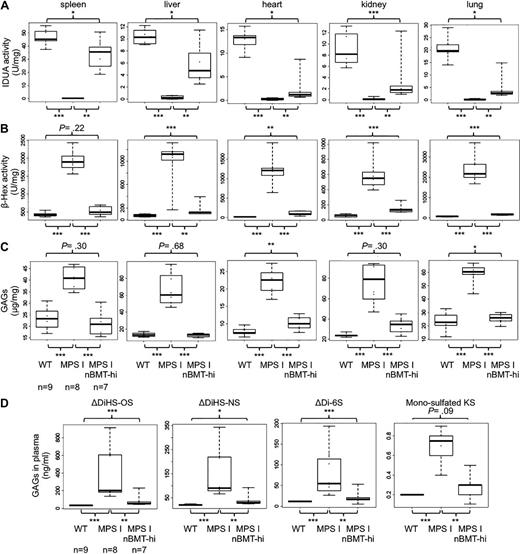
IDUA activity markedly increases in peripheral organs of nBMT MPS I mice, resulting in reduction of GAG levels
The tissues (spleen, liver, heart, kidney, and lung) harvested from MPS I nBMT mice were evaluated for IDUA activity compared with those from 37-week-old WT and untreated MPS I mice. All homogenates from MPS I mice had no IDUA activity, as shown in Figure 2A. MPS I nBMT-hi mice displayed partial restoration of IDUA activity in all evaluated tissues, particularly high in spleen (70% of WT mice) (Figure 2A). IDUA activity in liver and kidney in MPS I nBMT-hi mice increased to up to 40% of values found in WT mice. IDUA activity in the heart and the lung of MPS I nBMT-hi mice was 20% of the enzyme activity in WT mice. Furthermore, we evaluated IDUA activity levels in each organ compared with the percentage of donor engraftment in PB for all MPS I nBMT mice. Enzyme activity in all the tissues, except the heart, significantly correlated with the levels of donor cells in PB (supplemental Figure 1). In addition, the levels of the lysosomal enzyme β-hexosaminidase, which results elevated in MPS I, were significantly reduced in the same tissues after nBMT (Figure 2B).
Lysosomal IDUA enzyme activity, β-hexosaminidase enzyme activity, and GAG levels. (A) IDUA activity was measured in spleen, liver, heart, kidney, and lung of WT (n = 9), MPS I (n = 8), and MPS I nBMT-hi mice (n = 7) at 37 weeks of life. (B) The β-hexosaminidase activity was measured in the same organs of WT (n = 9), MPS I (n = 8), and MPS I nBMT-hi mice (n = 7) at 37 weeks of life. (C) At 37 weeks of age, the level of sulfated GAGs was determined, using the Blyscan assay in the indicated organs of WT (n = 9), MPS I (n = 8), and MPS I nBMT-hi (n = 7). (D) At 37 weeks of age, the levels of ΔDiHS-0S, ΔDiHS-NS, ΔDi-6S, and mono-sulfated Galβ1-4GlcNAc (6S) (mono-sulfated KS) were determined using liquid chromatography tandem mass spectrometry in the plasma of WT (n = 9), MPS I (n = 8), and MPS I nBMT-hi (n = 7). Median, mean, and minimum/maximum values are shown. Statistical comparison between groups was performed using Wilcoxon nonparametric unpaired test, 2 sides.
Lysosomal IDUA enzyme activity, β-hexosaminidase enzyme activity, and GAG levels. (A) IDUA activity was measured in spleen, liver, heart, kidney, and lung of WT (n = 9), MPS I (n = 8), and MPS I nBMT-hi mice (n = 7) at 37 weeks of life. (B) The β-hexosaminidase activity was measured in the same organs of WT (n = 9), MPS I (n = 8), and MPS I nBMT-hi mice (n = 7) at 37 weeks of life. (C) At 37 weeks of age, the level of sulfated GAGs was determined, using the Blyscan assay in the indicated organs of WT (n = 9), MPS I (n = 8), and MPS I nBMT-hi (n = 7). (D) At 37 weeks of age, the levels of ΔDiHS-0S, ΔDiHS-NS, ΔDi-6S, and mono-sulfated Galβ1-4GlcNAc (6S) (mono-sulfated KS) were determined using liquid chromatography tandem mass spectrometry in the plasma of WT (n = 9), MPS I (n = 8), and MPS I nBMT-hi (n = 7). Median, mean, and minimum/maximum values are shown. Statistical comparison between groups was performed using Wilcoxon nonparametric unpaired test, 2 sides.
To confirm these data, we also quantified GAG levels in spleen, liver, heart, lung, and kidney from WT, MPS I, and MPS I nBMT-hi mice (Figure 2C). MPS I mice exhibited higher levels of GAGs storage in all organs, in comparison with WT mice (P < .0001 for all organs). In addition, MPS I nBMT-hi animals exhibited a statistically significant reduction in GAGs storage material in the spleen, liver, heart, kidney, and lung (MPS I nBMT-hi vs MPS I; P = .0003) (Figure 2C). GAG levels in spleen, liver, and lung of MPS I nBMT-hi mice were normalized (MPS I nBMT-hi vs WT, respectively, P = .30, P = .68, and P = .30), suggesting that nBMT-hi completely corrected an error of metabolism at these tissues.
Levels of plasma GAGs [ΔDiHS-0S, ΔDiHS-NS, ΔDi-6S, and mono-sulfated-Galβ1-4GlcNAc(6S) (mono-sulfated keratan sulfate [KS])] in untreated MPS I mice were significantly higher compared with those in WT mice (P < .0006 for all GAGs) (Figure 2D). The levels of these GAGs in MPS I nBMT-hi mice followed-up for 37 weeks were significantly reduced compared with untreated MPS I mice (MPS I nBMT-hi vs MPS I; P < .002) and were normalized in mono-sulfated KS (MPS I nBMT-hi vs WT; P = .09). Elevation of ΔDiHS-0S, ΔDiHS-NS, and ΔDi-6S derived from HS was a result of primary storage substrate, whereas KS was elevated secondarily because of the magnitude of skeletal dysplasia.
An important factor contributing to the reduction of GAG levels in the examined organs and plasma was the magnitude of engraftment. We observed an inverse correlation between the extent of hematopoietic chimerism and GAG levels (data not shown).
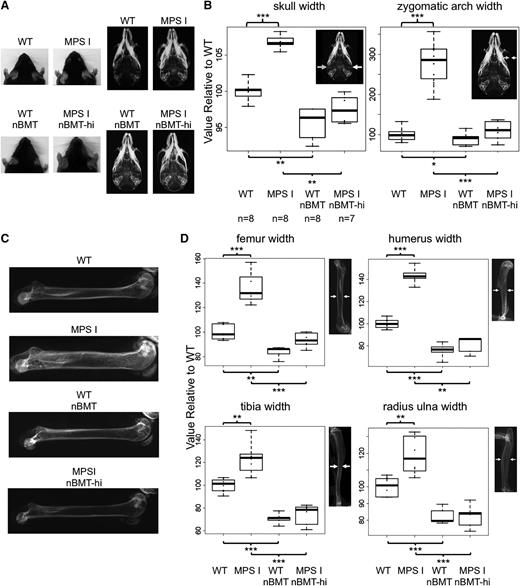
Correction of skeleton deformities in MPS I mice after nBMT
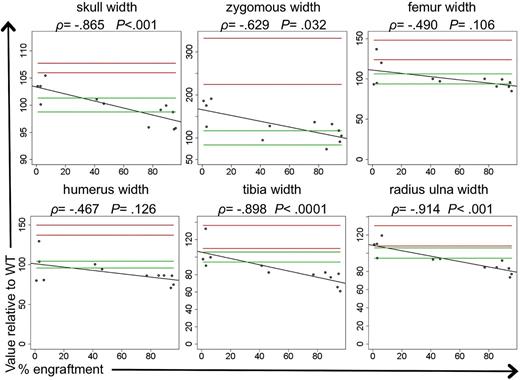
Marked skeletal deformities in the MPS I mouse model began at 16 to 24 weeks of age and included craniofacial abnormalities and thickening of the zygomatic arches and the long bones.19 At 37 weeks, the MPS I mice manifested an evident skeletal dysplasia. At this age, untreated MPS I mice had a short, broad face (Figure 3A). In contrast, the facial morphology of the MPS I nBMT-hi mice was overall normal and was similar to that of WT siblings (Figure 3A). Mice with lower engraftment presented an intermediate phenotype (data not shown). In agreement with the macroscopic features, radiograph analysis demonstrated that the width of the skull and the zygomatic arches was significantly higher in MPS I mice in comparison with WT mice, whereas a significant reduction in both parameters was observed in MPS I nBMT-hi mice (skull width, P = .0014; zygomatic arch width, P = .0003; vs untreated MPS I mice) (Figure 3A-B). In addition, radiographs of MPS I mice showed that long bones of the fore- and hind-limbs were thickened and sclerotic, whereas these features were consistently reduced in MPS I nBMT-hi mice, as shown in Figure 3C. As expected, the width of the humerus, radius/ulna, femur, and tibia of MPS I mice was also significantly larger than in WT littermates (Figure 3D). For MPS I nBMT-hi mice, the width of long bones, including the humerus (P = .0014 vs untreated MPS I mice), the radius/ulna (P = .0003 vs untreated MPS I mice), the femur (P = .0003 vs untreated MPS I mice), and the tibia (P = .0003 vs untreated MPS I mice) was significantly decreased compared with untreated MPS I mice (Figure 3D). Improvement of bone measurements evaluated in MPS I nBMT mice was proportional to the percentage of donor engraftment (Figure 4).
nBMT prevents bone defects in MPS I mice. (A) Skull morphology (on the left) and radiographs (on the right) of 37-week-old WT, MPS I, WT nBMT, and MPS I nBMT-hi mice. Signs of skull abnormalities include blunted snouts with a loss of the fine taper to the face. (B) Measurements of maximum skull width and zygomatic arch width. All measures were performed on radiographic images of WT (n = 8; 4 males and 4 females), MPS I (n = 8; 4 males and 4 females), WT nBMT (n = 8; 5 males and 3 females), and MPS I nBMT-hi mice (n = 7; 4 males and 3 females), as shown on the right side of each chart. The median values relative to WT mice and minimum/maximum values are shown. *P < .05; **P < .01; ***P < .001 with Wilcoxon nonparametric unpaired test, 2 sides. (C) Representative examples of femur radiographs of WT, MPS I, WT nBMT, and MPS I nBMT-hi mice. (D) Measurements of femur, humerus, tibia, and radius-ulna thicknesses. The pictures on the right side of each graph indicate how measures were calculated. The median values relative to WT mice and minimum/maximum values are shown. *P < .05; **P < .01; ***P < .001 with Wilcoxon nonparametric unpaired test, 2 sides.
nBMT prevents bone defects in MPS I mice. (A) Skull morphology (on the left) and radiographs (on the right) of 37-week-old WT, MPS I, WT nBMT, and MPS I nBMT-hi mice. Signs of skull abnormalities include blunted snouts with a loss of the fine taper to the face. (B) Measurements of maximum skull width and zygomatic arch width. All measures were performed on radiographic images of WT (n = 8; 4 males and 4 females), MPS I (n = 8; 4 males and 4 females), WT nBMT (n = 8; 5 males and 3 females), and MPS I nBMT-hi mice (n = 7; 4 males and 3 females), as shown on the right side of each chart. The median values relative to WT mice and minimum/maximum values are shown. *P < .05; **P < .01; ***P < .001 with Wilcoxon nonparametric unpaired test, 2 sides. (C) Representative examples of femur radiographs of WT, MPS I, WT nBMT, and MPS I nBMT-hi mice. (D) Measurements of femur, humerus, tibia, and radius-ulna thicknesses. The pictures on the right side of each graph indicate how measures were calculated. The median values relative to WT mice and minimum/maximum values are shown. *P < .05; **P < .01; ***P < .001 with Wilcoxon nonparametric unpaired test, 2 sides.
Correlation between donor engraftment and bone radiographic measurements. Relationship between percentage of donor engraftment and cranium and long bones measurements. For MPS I nBMT mice (n = 13), the percentage of donor engraftment (x-axis, % human CD45.1+ cells) was plotted against the ratio of bone measurements with respect to that in WT mice. For all graphics, the linear regression line, the ρ value, and the statistical likelihood that there is a correlation between the 2 variables are shown. Green lines indicated WT values, and red lines MPS I untreated values.
Correlation between donor engraftment and bone radiographic measurements. Relationship between percentage of donor engraftment and cranium and long bones measurements. For MPS I nBMT mice (n = 13), the percentage of donor engraftment (x-axis, % human CD45.1+ cells) was plotted against the ratio of bone measurements with respect to that in WT mice. For all graphics, the linear regression line, the ρ value, and the statistical likelihood that there is a correlation between the 2 variables are shown. Green lines indicated WT values, and red lines MPS I untreated values.
Comparison of untreated WT mice with transplanted WT nBMT mice showed a significant decrease in all the analyzed bone measurements of treated mice (WT vs WT nBMT; P < .05 for all bones). This finding agrees with the fact that busulfan toxicity per se causes reduction in bone dimensions of treated mice.28 Therefore, to separate the adverse effect of busulfan treatment from the therapeutic effect of BMT on MPS I, we studied the interaction between treatment and disease, using an analysis of variance regression model on the 4 groups (WT, MPS I, WT nBMT, and MPS I nBMT-hi), considering the presence/absence of disease and the presence/absence of treatment and their interaction. Results of analysis of variance models are represented in supplemental Table 1, where β1 is the change in the average of the parameter resulting from disease, β2 is the nBMT effect on WT mice, and β2+γ is the nBMT effect on MPS I mice. The analysis of γ reveals the differential effect of treatment on MPS I attributable to BMT only. A significant interaction was found in the measures of all bones examined (skull width, P = .0008; zygomatic arch width, P < .00001; femur width, P = .0005; humerus width, P < .00001; tibia width, P = .014; and radius/ulna width, P = .0054). The groups of WT nBMT and MPS I nBMT-hi provided comparable values.
To investigate the effect of nBMT on the skeletal phenotype of MPS I mice, micro-CT scan was performed on the right femur of untreated WT and MPS I mice compared with MPS I nBMT-hi mice. To avoid sex biases, the femurs were analyzed only in the male mice. Micro-CT reconstructions of the 2- and 3-dimensional architecture of femurs from 37-week-old MPS I mice indicated that skeletal abnormalities in both the cortical and trabecular bone (Figure 5A) were consistent with the data described previously in MPS I and other MPS mouse models.21 In particular, the trabecular density was exceptionally higher in the affected bones compared with the WT samples. In contrast to WT mice, the cortical bone of MPS I mice was abnormally thick and irregular in structure (Figure 5A).
nBMT enhances cortical and trabecular bone architecture in MPS I mice. Micro-CT evaluation of femurs from 37-week-old male WT (n = 3), MPS I (n = 3), and MPS I nBMT-hi (n = 5) mice. (A) Representative 2D and 3D reconstructed images of trabecular bone and of midshaft cortical bone (transaxial section). (B) Bone mineral volume (BV/TV), trabecular separation (Tb. Sp.), trabecular number (Tb. N.), and cortical bone thickness (Cort. Thick.) were measured using Skyscan CT-analyzer software and the data presented as dot plot. *P < .05 with Wilcoxon nonparametric unpaired test, 1 side. (C) Representative pictures of the femur cortical bones of MPS I and MPS I nBMT-hi mice (hematoxylin and eosin staining), as indicated. The inner surface of the cortex is on the left. Magnifications, ×20 and ×40. (D) Representative pictures of the proximal tibia and distal femoral growth plate of MPS I, WT nBMT, and MPS I nBMT-hi mice (Toluidine blue stain, ×40).
nBMT enhances cortical and trabecular bone architecture in MPS I mice. Micro-CT evaluation of femurs from 37-week-old male WT (n = 3), MPS I (n = 3), and MPS I nBMT-hi (n = 5) mice. (A) Representative 2D and 3D reconstructed images of trabecular bone and of midshaft cortical bone (transaxial section). (B) Bone mineral volume (BV/TV), trabecular separation (Tb. Sp.), trabecular number (Tb. N.), and cortical bone thickness (Cort. Thick.) were measured using Skyscan CT-analyzer software and the data presented as dot plot. *P < .05 with Wilcoxon nonparametric unpaired test, 1 side. (C) Representative pictures of the femur cortical bones of MPS I and MPS I nBMT-hi mice (hematoxylin and eosin staining), as indicated. The inner surface of the cortex is on the left. Magnifications, ×20 and ×40. (D) Representative pictures of the proximal tibia and distal femoral growth plate of MPS I, WT nBMT, and MPS I nBMT-hi mice (Toluidine blue stain, ×40).
Quantitative analyses demonstrated that several cortical and trabecular bone morphometric parameters were significantly altered in the affected MPS I mice in comparison with those in WT siblings. Consistent with the high donor engraftment level, these parameters showed a 40% to 80% improvement in MPS I nBMT-hi with respect to untransplanted MPS I mice, approaching the values observed in WT mice (Figure 5B). Quantitative analysis demonstrated a significant increase in bone mineral volume in untreated MPS I mice in comparison with WT mice (median, 21.88% vs 10.73%, respectively) (Figure 5B). A decrease in bone mineral volume, although not significant, was observed in MPS I nBMT-hi mice (median, 7.58%) compared with untreated MPS I animals. Trabecular separation was significantly reduced in MPS I untreated mice in comparison with WT animals (median, 0.18 mm in MPS I vs 0.25 mm in WT). However, BMT treatment significantly increased trabecular separation in MPS I nBMT-hi mice (median, 0.26 mm) toward WT mice. In addition, trabecular number significantly increased in untreated MPS I mice in comparison with WT mice (median, 3.97/mm vs 2.04/mm, respectively), whereas a significant decrease in trabecular number was observed in treated MPS I nBMT-hi mice (median, 1.52/mm) with respect to WT animals. Trabecular thickness of untreated MPS I mice was unchanged from WT (P = .2) (data not shown) and was not affected by BMT. Cortical thickness increased in untreated MPS I mice in comparison with WT mice (median, 0.25 vs 0.15 mm, respectively) and decreased to normal levels after BMT in MPS I nBMT-hi mice (0.19 mm). Further parameters in which a significant improvement in MPS I nBMT-hi mice was detected are reported in supplemental Table 2.
Histopathologic evaluation of long bones from MPS I and treated MPS I nBMT-hi mice confirmed the micro-CT findings. Hematoxylin and eosin-stained sections of long bones showed increased number and vacuolization (likely reflecting the lysosomal storage) of osteocytes in the cortical bone of MPS I mice. Both these features were reduced in cortical bone osteocytes of MPS I nBMT-hi mice (Figure 5C). In addition, the analysis of the femurs has shown an evident improvement in chondrocyte orientation and growth plate organization in MPS I nBMT-hi mice compared with untreated MPS I mice, in which we could observe a disorganization of the growth plate (Figure 5D).
Discussion
The relevance of hematopoietic stem cell transplantation with either BM or umbilical cord blood29 in the treatment of MPS IH is well established, together with enzyme replacement therapy. However, both approaches do not provide complete resolution in the clinical history of skeletal dysplasia, one of the most severe complication of this disease. The most recent international retrospective studies on patients with MPS IH transplanted in European and American centers have demonstrated that the decrease of the age at hematopoietic stem cell transplantation through earlier diagnosis and the achievement of complete donor chimerism can favorably affect patient outcomes after hematopoietic stem cell transplantation.8,12
We demonstrated that robust hematopoietic repopulation of MPS I mice in the neonatal period results in the restoration of IDUA enzyme activity, the clearance of GAGs storage, and significant pathological and structural improvement of the bones, with normalization of the skeletal phenotype.
The more than 50% replacement of the hematopoiesis resulted in a measurable increase in IDUA activity and a consequent decrease in β-hexosaminidase activity in visceral organs, especially in the spleen, showing a correlation between engraftment levels and enzyme activity with clearance of GAGs from blood and tissues. We found that even if IDUA activity in all tissues was only partially restored by nBMT, GAG levels in the majority of the tissues investigated were completely normalized, suggesting that if BMT in MPS I mice is conducted in neonates, in contrast to adults,22 subnormal levels of enzyme activity are sufficient to normalize GAGs storage and minimize the skeletal phenotype. The progressive skeletal dysplasia remains unsolved after BMT on patients with MPS IH.30 Likewise, BMT ameliorates, but does not prevent, cardiac, skeletal, corneal, or neurologic disease in small and large animal models of MPS I. In these studies, animals were transplanted after the neonatal period, and in some of them, engraftment levels were suboptimal.22,31-34 MPS VII mice treated with BMT in neonatal life showed pathological and clinical improvements by clearing lysosomal storage in bones, joints, and visceral organs, even though engraftment achieved was low (15% to 20%).16,17 To achieve a more complete donor-derived engraftment, we decided to use a busulfan-mediated preconditioning regimen, which was previously reported to result in high levels of hematopoietic engraftment after nBMT, and a complete hepatic correction in the erythropoietic protoporphyria mouse model.23 Different from BMT in patients with MPS IH, in whom a significant amount of primary and secondary graft rejection has been observed,12,35 we here demonstrate that more than 50% of transplanted MPS I mice developed complete, lifelong chimerism, similar to their WT counterparts. No significant acute toxicity was observed in transplanted mice. Spleen, PB, and thymus cells of nBMT MPS I mice were repopulated with committed lymphoid and myeloid populations similar to the transplanted WT mice. These findings demonstrate that the combination of a myeloreductive preconditioning regimen with busulfan and subsequent BMT in newborn mice is effective, creating a good model for the study of neonatal cell therapy in MPS I and other MPS mouse models.
We focused on the skeletal abnormalities that develop in MPS I mice and evaluated the effect of nBMT on these aberrations at 37 weeks of age. First, MPS I and WT mice grew normally after transplantation, with the exception of decreased body weight and size secondary to busulfan treatment.28 At the time of euthanasia (37 weeks old), reconstitution of normal hematopoiesis in MPS I mice was associated with a consistent amelioration of bone pathology, as revealed by radiographic skeletal examination. We found that nBMT reduced bone thickening in the skull, zygomatic arches, and long bone segments. As busulfan treatment per se causes a reduction in bone dimension, we also analyzed the radiographic measurements with a statistical model that separates the therapeutic effects of BMT on MPS I bones from the adverse effect of busulfan treatment on bones of transplanted MPS I or WT mice. This demonstrated a therapeutic effect on MPS I mice exclusively attributable to nBMT.
We also measured several 2- and 3-dimensional architectural parameters of the femurs, such as trabecular number and separation, cortical thickness, and bone mineral volume by micro-CT. This revealed significant differences between untreated and nBMT MPS I mice. All examined nBMT MPS I mice displayed bone parameter values comparable to those of WT mice, confirming that nBMT mice had significant improvements in skeletal phenotype approaching complete normalization of each parameter tested. Histologically, in MPS I cortical bone, osteocytes were increased and contained vacuoles, likely reflecting GAGs storage, as also observed in other studies.36 Histological amelioration of these features was consistently observed in femurs of all nBMT mice, with a definite reduction in both hyperosteocytosis and lysosomal vacuolization in the cortical bone and an evident improvement in the growth plate organization, confirming that the perinatal treatment of the disease can positively affect the skeletal phenotype in MPS I.
It is noteworthy that KS level was normalized after nBMT in MPS I mice. Elevation of KS in MPS I is probably a secondary consequence resulting from the skeletal dysplasia, possibly be released from cartilage damaged by accumulated GAGs and subsequent inflammation.37,38 Therefore, we also evaluated KS levels in the blood as a biomarker of MPS with skeletal dysplasia. Normalization of blood KS level strongly supports the notion that nBMT corrects the pathological and clinical bone lesions in nBMT MPS I mice.
Taken together, radiologic, histopathologic, and biochemical findings demonstrated that nBMT can prevent progression of the skeletal phenotype in MPS I mice. Previous works in MPS I animal models and patients have shown improvements in bone and/or joint disease after early initiation of intravenous enzyme replacement therapy.39 Furthermore, gene therapy at birth in MPS I and MPS VII mice and dogs also resulted in significant benefits on the phenotypic manifestations of the disease, including skeletal anomalies.40-44 Until now, only a few reports described the skeletal outcome of nBMT in mouse models with MPS.
Our findings demonstrate that nBMT prevents some of the relevant abnormalities of the skeletal pathology in the MPS I mouse model. Moreover, improvements in bone parameters correlated with high levels of BM-derived cell engraftment in multiple hematopoietic compartments, suggesting that the early and complete restoration of normal hematopoiesis can have a significant effect on the bone development of newborn MPS I mice. Overall, our study supports the notion that hematopoietic transplantation from a healthy donor can be an effective strategy to restore the missing or defective protein underlying the genetic disorder. However, the clinical efficacy is strictly dependent on providing the missing protein at a very early stage, before symptoms become apparent.
This is a proof-of-concept study that advocates nBMT as a highly effective therapeutic approach for Hurler syndrome, demonstrating that an early treatment may further affect the clinical outcome of these patients and strongly supporting the importance of the implementation of newborn screening procedures to allow an early diagnosis and immediate treatment of affected children.
In particular, unrelated umbilical cord blood may be particularly fascinating, as it would allow a rapid transplantation immediately after the newborn screening. Moreover, cord blood from unrelated donors appears to be an excellent source of hematopoietic stem cells for transplantation in patients with Hurler syndrome, resulting in full-donor chimerism and normal enzyme levels in almost all the transplanted patients.12,29
Future clinical trials are needed to confirm our findings in patients.
The online version of this article contains a data supplement.
There is an Inside Blood Commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank A. Rovelli (Fondazione Monza e Brianza per il Bambino e la sua Mamma–San Gerardo Hospital) and C.M. Verfaillie (KU Leuven) for advice and comments on the manuscript and C. Viscomi and I. Di Meo (The Foundation “Carlo Besta” Institute of Neurology Istituto di Ricovero e Cura a Carattere Scientifico) for expert technical assistance. We also are indebted to E. Richard (Université de Bordeaux) for general advice and help for the initial setting up of the transplantation experimental method.
This work was supported by the Italian Telethon Foundation (TCP 07004) and Progetto ARTEVITA (to M.S.). M.S. is assistant telethon scientist at the Dulbecco Telethon Institute. S.T. was supported by an Institutional Development Award from the National Institute of General Medical Sciences of the National Institutes of Health under grant number P20GM103464.
Authorship
Contribution: A.P. performed research, analyzed the data, and wrote the manuscript; L.A. performed statistical analysis; I.A., C.R., and B.R. performed research; T.S. and P.P. performed micro-CT analysis and GAG assay; M.G.V. revised the statistical plan and the manuscript; M.R. interpreted the data and edited the manuscript; A.B. edited the manuscript; S.T. performed micro-CT analysis and GAG assay by tandem mass spectrometry, interpreted the data, and edited the manuscript; and M.S. designed research, interpreted the data, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Marta Serafini, Dulbecco Telethon Institute at Centro Ricerca M. Tettamanti, Department of Pediatrics, University of Milano-Bicocca, San Gerardo Hospital/Fondazione MBBM, via Pergolesi, 33, 20900 Monza, Italy; e-mail: serafinim72@gmail.com.

![Figure 1. Donor hematopoietic engraftment into newborn transplanted MPS I mice. (A) Experimental scheme. Newborn WT and MPS I (CD45.2) mice were conditioned with busulfan (20 mg/kg) on day 1 to 2 after birth and transplanted with 2 × 106 adult BM nucleated cells (CD45.1) on the next day, as indicated. Groups were WT untreated (WT), MPS I untreated (MPS I), MPS I mice transplanted with CD45.1 donor BM cells (MPS I nBMT), and WT mice transplanted with CD45.1 donor BM cells (WT nBMT). Chimerism was determined at 4 weeks of age, and at 37 weeks of age, mice were killed for detection of long-term engraftment, biochemical, radiographic, and histological analyses. (B) Long-term donor chimerism (engraftment of CD45.1+ cells) was determined using flow cytometry in PB and spleen at 37 weeks of age. Upper horizontal line of box represents the 75th percentile, the lower horizontal line of box represents the 25th percentile, the horizontal bar within the box represents the median, the square within box represents the mean, and vertical lines outside the box represent the minimum and maximum. P value was calculated using Wilcoxon nonparametric unpaired test, 2 sides. (C) Representative multilineage donor-derived reconstitution was analyzed, using flow cytometry in spleen (macrophages [MAC], granulocytes [GRAN], B and T lymphoid cells) and thymus (T lymphoid cells) of recipient WT nBMT and MPS I nBMT mice.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/125/10/10.1182_blood-2014-06-581207/4/m_1662f1.jpeg?Expires=1767721662&Signature=vWCMgFaprroEWSWQYugRT2MtpZY-ARrBWmRVIAtMadrAL0nko~sKG0yzPaS908zYKKRKZSbXZ0FU1svWya3RV2sIaffd7hOa~kHkgMfp~dE2i3IsusZw35GUd0HvTms4yYUT5Klz-1pXZ7~JCqEfsDxuxZNdz3AloeIvOFf6ADtq3Sl08RwzBuQX-foW5pGeYRwhN5EC85C1vRuMKLtsgNJ6k~UJzWwSkO1MY~5OJbDHGmQ~sSSSgjvh9TVSfTMgvjeqKSZt8IVndavGaP6w9k70-fk5Ytb8kt2JWh9X1RJaRXQ8N~j5nmmkWmBnmYbSSB2XCOoGiqakC4UHGXx~Lg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)