Abstract
Introduction: The MLL gene on located on 11q23 plays an essential role in positive regulation of gene expression in early embryonic development and hematopoiesis. Fusion genes, such as MLL-AF4 resulting from t(4:11)(q21;q23), alter normal cellular proliferation and differentiation, favoring leukemogenesis. The DOT1L histone methyltransferase associated with MLL appears to be required for maintenance of ALL. MLL-AF4 is detected in about 10% of de novo B-lymphoblastic leukemia or 30=40% of pro-B ALL subtypes. The 11q23/MLL subtype of ALL has been associated with extremely poor outcomes. We conducted a retrospective analysis of de novo adult ALL with 11q23/MLL gene rearrangements.
Methods: Overall the database included 74 pts with 11q23/MLL gene rearrangements referred to our institution between 1980 and 2014. Of these, 20 (27%) pts were relapsed/refractory, 4 (5%) were minimally pretreated, 5 (7%) were inevaluable for response, 3 (4%) had concomitant Philadelphia chromosome, 2 (3%) were T-lineage, 2 (3%) were mature B-ALL. The remaining 38 cases comprised the study cohort evaluated with respect to pretreatment characteristics and outcome measures such as response to therapy, remission duration (CRD), and survival (OS).
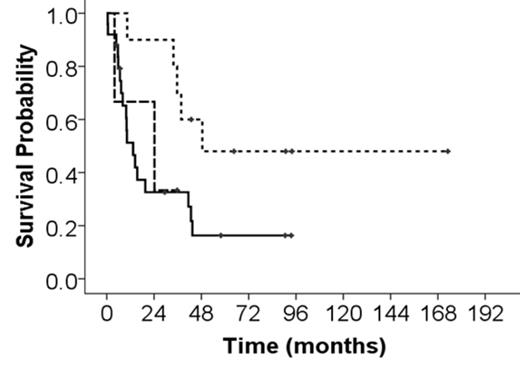
Results: Baseline characteristics of the cohort included median age 44 yrs (range, 20-75); 26% were older than 60 yrs. Ten (26%) pts had a prior malignancy and were designated secondary ALL. Five (13%) pts had CNS disease at presentation. Median WBC count was 69.8 K/uL (range, 0.5-612); 24 (63%) pts had WBC > 30 K/uL. Nineteen (50%) pts had serum LDH > 1400 U/L. Co-expression of myeloid markers (CD13, CD33 +/- CD117) was noted in 6 (16%) pts. Distribution of the 11q23/MLL gene aberrancies were: t(4;11) (q21; q23) in 25 (66%) pts, 11q23 without translocation partner in 10 (26%) pts, and t(11;19)(q23;p13.1) in 3 (8%) pts. Thirty two (84%) pts were treated per the hyper-CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone alternating with high dose methotrexate and cytarabine) regimen (3 [10%] received concurrent rituximab) and 6 (16%) pts were treated per the augmented BFM regimen. Overall response rate was 95%; complete remission (CR) in 92% and CR without platelet recovery (CRp) in 3%. Overall median CRD was 26.3 mos (range 0.2-93+ mos); median OS was 24.2 mos. Overall, the 5-yr CRD and OS rates were 19% and 26%, respectively, with a median follow-up of 60 mos (range, 4.8-173+ mos). Median OS in pts with 11q23 without chromosomal translocation was 48.5 mos, compared with 24 mos for t(11; 19) and 13.3 mos for t(4; 11) (p= 0.07) (Fig. 1). There were no differences in outcomes by older age or designation as secondary ALL.
Conclusion: The 11q23/MLL positive B-lymphoblastic subsets are associated with differentially inferior outcomes, although MLL-AF4 remains the ALL subset associated with highest risk of disease recurrence particularly in the absence of allogeneic stem cell transplantation; the relatively rarity of these subsets poses challenges in establishing the optimal treatment strategies. Therapeutic approaches incorporating hypomethylating agents, histone deacetylase inhibitors, and CAR-T cells could improve these dismal outcomes; targeted agents such as DOT1L inhibitors are under investigation in clinical trials.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal