Abstract
Background:
Complex karyotypes in patients with myelodysplastic syndromes (MDS) are defined by the presence of 3 or more cytogenetic abnormalities and are considered indicators of a poor prognosis by nearly all models in clinical use. There is evidence that the prognostic significance of complex karyotypes in MDS can be refined by considering the number of cytogenetic abnormalities or the presence of specific lesions, the presence of monosomy, and the mutation status of the TP53 gene. Mutations of TP53 are strongly associated with adverse clinical features including complex karyotypes, yet still have independent prognostic significance. Whether these mutations or other elements associated with complex karyotypes carry the greatest prognostic significance is unknown and has been the subject of recent contradictory findings. Here we examine the relationship between TP53 mutations, the number and type of chromosomal abnormalities, and clinical features including overall survival in a combined analysis of MDS patients with complex karyotypes.
Methods:
Data on 258 complex karyotype MDS patients from the US and Europe gathered by members of the International Working Group for Prognosis in MDS-Molecular Committee were combined for this analysis. Patients gave informed consent to have their data and clinical samples collected at their respective institutions in accordance with the Declaration of Helsinki. Tumor samples were examined for TP53 mutations primarily with next generation sequencing techniques. Categorical variables were compared using a Fisher exact test or Kruskal-Wallis test as appropriate, while continuous variables were compared using a Wilcoxon rank-sum test. All p-values reported are two-sided, unadjusted for multiple testing, and considered significant at the 0.05 level.
Results:
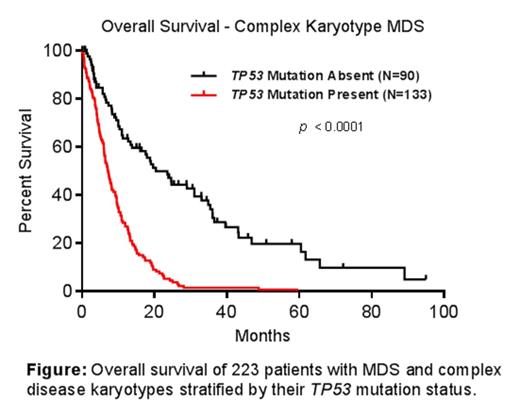
Of the 258 complex karyotype MDS samples examined, TP53 mutation status was determined in 223, of which 133 (60%) carried a TP53 mutation. Patients with TP53 mutations were slightly older than unmutated patients (median age 70.8 vs. 65.5 years, p=0.055), were more thrombocytopenic (median platelet count 42 vs. 78 x109/L, p=0.002), and had a greater percentage of bone marrow blasts (7.75% vs 4%, p=0.03). Mutated patients were also more likely to have a monosomal karyotype (85% vs. 59%, p<0.0001), have 5 or more chromosomal abnormalities (85% vs. 51%, p<0.0001), and have abnormalities of chromosome 17 (38% vs. 23%, p=0.03).
Patients with TP53 mutation had a significantly shorter median overall survival of 7.7 months compared to 23.4 months for patients with unmutated TP53 (p<0.0001, see figure). Multivariate analysis that considered potential confounders such as monosomal karyotypes, number of abnormalities, blast proportions and platelet count identified TP53 mutation status as the most significant prognostic marker for overall survival (hazard ration [HR] 2.12, p<0.0001). The presence of only 3 or only 4 karyotype abnormalities was protective compared with 5 or more such lesions (HR 0.385, p=0.0005 for 3 lesions and HR 0.505, p=0.0083 for 4 lesions).
Discussion:
Despite strong associations with adverse clinical and cytogenetic abnormalities incorporated into existing prognostic scoring systems, TP53 mutations carry significant independent prognostic value for patients with MDS. In our multivariable analyses, TP53 mutation appears to dominate over monosomal karyotype as an adverse prognostic marker in MDS patients with complex cytogenetics. Many of the TP53 mutations identified had a small variant allele fraction suggesting that they were present in a disease subclone. The small number of mutant cells in these cases may be insufficient to alter clinical measures, but could still indicate a poor prognosis if they represent a clone capable of treatment resistance and rapid disease progression.
This combined analysis is a work in progress that will include data from additional groups and explore mutation status of other MDS-related genes, TP53 variant allele fraction, clinical risk scores, and data from patients without complex karyotypes.
Conclusions:
Somatic TP53 mutations are highly enriched in MDS patients with complex karyotypes and identify a group with significantly shortened overall survival. Sequencing of TP53 can improve the prediction of prognosis in MDS patients with 3 or more chromosomal abnormalities.
Bejar:Genoptix Medical Laboratory: Consultancy, Honoraria, Licensed IP, no royalties Patents & Royalties, Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees. Haferlach:MLL Munich Leukemia Laboratory: Other. Garcia-Manero:Celgene: Research Funding. Sekeres:Celgene: Membership on an entity's Board of Directors or advisory committees; Amgen Corp: Membership on an entity's Board of Directors or advisory committees; Boehringer-Ingelheim Corp: Membership on an entity's Board of Directors or advisory committees. Campbell:14M Genomics Limited: Consultancy, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal