Abstract

Background: Although the prognosis of patients with hematological malignancies admitted to the intensive care unit (ICU) has improved over the past years, it remains poor in allogeneic stem cell transplantation (SCT) recipients and thus admission of these patients to the ICU remains controversial. Our center has flexible admission criteria, especially regarding graft-versus-host disease (GVHD). We thus performed a retrospective study to assess prognostic factors of survival in allogeneic SCT recipients who are admitted according to this policy.
Methods: All allogeneic SCT recipients between 2002 and 2013 who were admitted to the medical ICU in our center were included. Details on patients, graft procedures, GVHD, ICU admission, and outcome were collected from individual medical records. Potential prognostic factors were explored by logistic regression analysis for ICU and hospital discharge. Cox regression analysis was performed for overall survival.
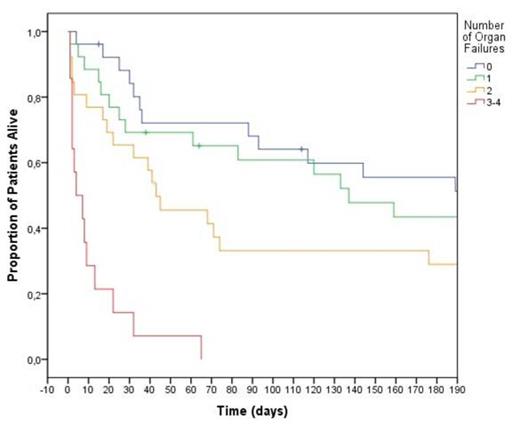
Results: Of 344 patients who underwent allogeneic SCT during the study period, 92 patients (27%) were admitted to the ICU. Median time from transplantation to ICU admission was 53 days (range: -4 to 2273 days). Median age was 52 (range: 20-69). They received myeloablative (27%), sequential treatment with chemotherapy and reduced-intensity conditioning (RIC) (27%) or RIC (46%). Donors were mostly unrelated donors (59%) while graft source was mostly peripheral blood stem cells (78%) (bone marrow: 13%, cord blood: 9%). 66% patients could be discharged from the ICU and 46% from hospital whereas one year survival was 24%. No demographic or SCT parameter was associated with ICU or hospital discharge, or with overall survival. Grade 2-4 acute GVHD (34 patients, 37%) and refractory acute GVHD (12 patients, 13%) had a significant impact on hospital discharge (11/34 patients alive, OR: 2.4, 95% CI: 1-5.8, p=0.05; 2/12 patients alive, OR: 5, 95% CI: 1-24, p=0.05, respectively) but not with ICU discharge (20/34 patients alive, p=0.25; 7/12 patients alive, p=0.53, respectively). Chronic GVHD was present in 11 patients (12%) without impact on survival. At admission to the ICU, patients had a median SOFA (Sequential Organ Failure Assessment) of 7 (range 1-16), a median LODS (Logistic Organ Dysfunction System) of 4 (range 0-17), and a median APACHE II (Acute Physiology And Chronic Health Evaluation II) of 19 (range 8-42). The SOFA and LODS are efficient for determining ICU discharge (OR: 1.3, 95% CI: 1.1-1.5, p=0.003; OR: 1.3, 95% CI: 1.1-1.5, p=0.002, respectively). 46 patients (50%) required invasive mechanical ventilation, 28 patients (30%) required vasopressors, 16 patients (17%) required renal replacement therapy, and 26 patients (28%) had liver failure (bilirubin >34µmol/l). Mortality was greatly associated with the number of organ failures: each new organ failure worsens the prognosis (Figure). One year OS rates were 31%, 27%, 23%, and 0% among patients with 0 (26 patients, 28%), 1 (26 patients, 28%), 2 (26 patients, 28%), and 3 to 4 (14 patients, 15%) organ failures, respectively (HR: 1.7, 95% CI: 1.4-2.1, p<0.001).
Conclusion: Allogeneic SCT recipients with 3 or 4 organ failures require further improvement of care. GVHD cannot be considered as a contraindication for transfer in the ICU per se, even with 2 organ failures.
Overall survival according to the number of organ failures
Overall survival according to the number of organ failures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal