Abstract
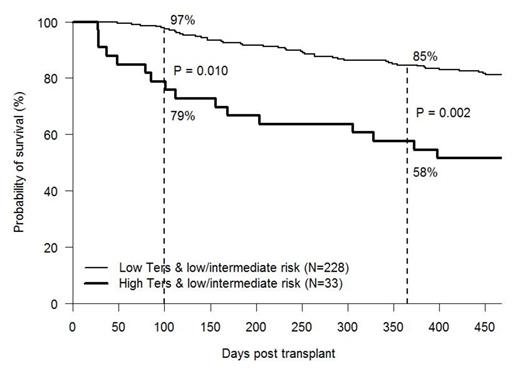
Several studies have begun to examine the relationship between psychosocial variables and outcome in hematopoietic stem cell transplantation (HSCT). Previous studies have also looked at the relationship between the Hematopoietic Cell Transplantation Comorbidity Index (HCT-CI) and disease risk on overall survival in HSCT. Research has shown that disease risk and HCT-CI may have a negative relationship with outcome in HSCT. In this study, psychosocial data was collected prospectively on 437 patients undergoing related and unrelated allogeneic HSCT. All patients were assessed using the Transplant Evaluation Rating Scale (TERS). Based on the patient’s TERS score, each patient was stratified into one of two groups (low/moderate risk (n=371) vs. high risk (n=66)) based on their predicted psychosocial risk for problems during transplant. The 1-year overall survival (OS) for the low/mod risk TERS group versus the high TERS risk group was 78% and 61%, respectively (p=.005). Stratification by CIBMTR disease risk identified 261 patients with low and intermediate risk disease of which 228 had low/mod risk TERS score and 33 had high risk TERS score. The is a significant survival advantage for Low/Mod Risk TERS patients vs. High Risk TERS patients at 100 day, 1 year and overall survival being 97% vs 79% (P=.01), 85% vs 58% (P=.002) and 68% vs 42% (P=.002) with a median follow up of 48 months (graph attached). An adjusted logistic regression analysis showed that psychosocial factors have a significant impact on overall survival despite all patients being required to have 24 hour caregiver support, a pre-transplant psychosocial evaluation and post-transplant psychosocial intervention. The analysis controlled for other variables such as age, gender, performance status, disease risk and transplant type. These results highlight the impact of psychosocial factors on HSCT outcome, as those patients who are expected to do well based on their low/intermediate disease risk may not perform as expected due to psychosocial risk factors. These results suggest the need to perform careful psychosocial assessments on all HSCT patients in order to predict mortality risks for the individual patient and to help the transplant team strategize how to better manage the high risk psychosocial patient.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal