Abstract
Reliable biomarkers of primary central nervous system lymphoma (PCNSL) are needed to support the magnetic resonance imaging (MRI) findings especially when the cerebral biopsy cannot be performed for pathologic examination. Biomarkers are also needed to optimize the assessment of therapeutic response, which so far relies only on gadolinium uptake on MRI, although large discrepancies of outcomes are observed in patients in complete remission assessed by MRI criteria.
The aim of the present study was to evaluate the diagnostic and prognostic values of the cerebrospinal fluid (CSF) concentrations of interleukin (IL)-10 and IL-6 and of the IL-10:IL-6 ratio in patients with diffuse large B-cell type (DLBCL) PCNSL, at time of diagnosis and after treatment.
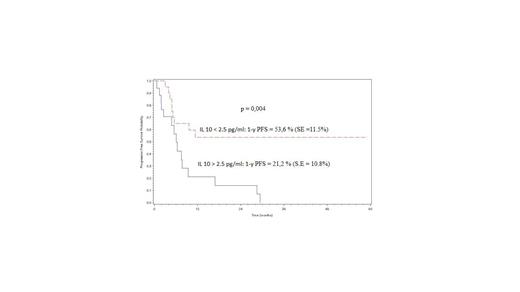
IL-10 and IL-6 levels were measured in 120 patients with DLBCL-PCNSL and 36 control patients with other brain tumor or inflammatory neurologic diseases, using the quantitative Cytometric Bead Array® technique (human IL-10 CBA kit and human IL-6 CBA kit; BD BiosciencesTM) on a FACSCanto II cytometer (BD BiosciencesTM) according to the manufacturer’s recommendations. Serial measures of cytokines were performed in 57 patients. The IL-10:IL-6 ratio distinguishes PCNSL from other neurological diseases. Using a cutoff level of 1.0, the sensitivity and specificity are 94% and 80% respectively. Meningeal dissemination defined by cytological examination and/or flow cytometry analysis, is significantly associated with a higher IL-10 concentration (417 pg/ml vs 22 pg/ml; p = 0.0024) and a higher IL-10:IL-6 ratio (32 vs 6 ; p = 0.0011). Previous treatment with corticosteroids significantly reduces the IL-10:IL-6 ratio (ratio=7.6 with corticosteroids vs 21.9 without corticosteroids; p= 0.02). With a median follow-up of 25 months, the pre-therapeutic concentration of IL-10 has no prognostic value on overall and progression free survivals. After treatment, the median concentration of IL-10 is significantly decreased in patients entering complete (CR) or partial response (PR) compared to non-responder patients (median = 35.9 pg/ml and 235.5 pg/ml respectively, p = 0.01). We demonstrate for the first time that among patients in CR or PR (as per MRI criteria), a persistent detectable IL-10 level in CSF (> 2,5 pg/ml) has an impact on the progression free survival (1 year PFS: 21.2 % vs 53.6%; p= 0,004) (figure 1).
Our study shows that IL-10:IL-6 ratio can be used as a diagnostic biomarker for PCNSL of DLBCL type . Analysis will be done to determine the cut off values of IL10 and IL-10:IL-6 ratio in a predictive model of meningeal dissemination. We also provide evidence that IL-10 concentration may be useful to complete the assessment of therapeutic response in PCNSL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal