Abstract
Introduction
Sepsis is the result of an uncontrolled inflammatory response to various stimuli such as bacterial infections. Sepsis can be complicated by hemodynamic instability, multi-organ dysfunction and hematological abnormalities. Patients with severe sepsis usually develop thrombocytopenia due to various reasons, and the presence of thrombocytopenia is considered as a negative prognostic marker. The aim of the present study was to determine the cytokine profile in serum of patients with severe sepsis and thrombocytopenia.
Patients and Methods
Serum cytokine profile was analyzed in a cohort of 112 consecutive patients with severe sepsis and/or septic shock treated in the intensive care unit (ICU) of our institute from October/2009 to September/2012. Patients were divided in two groups (A and B). Group A consisted of 43 patients with severe sepsis and thrombocytopenia (platelet count below 70X103/ìl), while group B consisted of 69 patients without thrombocytopenia. Patients with thrombocytopenia due to disseminated intravascular coagulation (DIC), suspected drug etiology, or due to any obvious etiology such as hematologic malignancy were excluded from our analysis. A cohort of 10 healthy volunteers served as control group.
Serum levels of IFNã, IL-8, ICAM, VCAM, and SUPAR (soluble urokinase plasminogen activation receptor) were estimated by using Luminex xMAP technology. Statistical analyses were performed using NCSS software. The following variables were entered in a multiple logistic regression model: 1) age and sex, 2) active malignancy vs. not, 3) septic shock vs. severe sepsis, 4) APACHEII score, 5) SOFA score, 6) serum IFNã, ICAM, VCAM, IL-8, and SUPAR levels, and 7) platelet number. All parameters were estimated on day of admission.
Results
Hospital Mortality: Overall 65 out of 112 patients died during their hospital stay. The overall hospital mortality was 58%. In multivariate analysis non-survivors had higher APACHE score (p=0.01) and had lower platelet counts (p<0.001) as compared with survivors.
Plasma cytokine levels in patients with and without thrombocytopenia: Patients in group A had a different cytokine profile as compared with patients in group B. Serum levels of VCAM and IFNã were not different between group A and B. However, patients with sepsis and thrombocytopenia had statistically significantly higher serum levels of ICAM, IL-8 and SUPAR (p<0.0001) in comparison with patients with severe sepsis and normal PLT count.
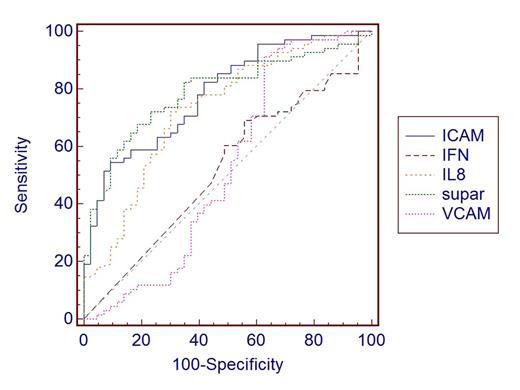
Predictive value of serum cytokine for thrombocytopenia: Serum levels of ICAM, IL-8, and SUPAR were good predictors of the presence of thrombocytopenia in patients with sepsis. The ROC curves of ICAM, IL-8, and SUPAR serum levels in predicting thrombocytopenia in patients with sepsis are shown in Figure 1. The AUCs were 0.785 (95% CI, 0.696 – 0.857, p<0.001), 0.729 (95% CI, 0.637 – 0.809, p<0.001), 0.789 (95% CI, 0.701 – 0.861, p<0.001) for ICAM, IL-8 and SUPAR levels respectively. However in multiple logistic regression analysis serum levels of ICAM was the most powerful predictor of thrombocytopenia.
Conclusion
Thrombocytopenia is not an uncommon finding in patients with severe sepsis. Although DIC or drug reactions are well known causes of low PLT counts, the pathogenesis of thrombocytopenia in patients with sepsis remains poorly understood. High levels of ICAM, IL-8 and SUPAR are usually associated with severe endothelial dysfunction. In our study, we showed that patients with thrombocytopenia have a specific serum cytokine profile expression consistent with the presence of endothelial damage.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal