Key Points
The duration of anticoagulation after VTE is uncertain; this management study intended to identify patients with low/high recurrence risk.
Patients with persistently negative D-dimers after stopping standard therapy have a low recurrence risk and can stop anticoagulation.
Abstract
The optimal duration of anticoagulation in patients with venous thromboembolism (VTE) is uncertain. We investigated whether persistently negative D-dimers in patients with vein recanalization or stable thrombotic burden can identify subjects at low recurrence risk. Outpatients with a first VTE (unprovoked or associated with weak risk factors) were eligible after at least 3 months (12 in those with residual thrombosis) of anticoagulation. They received serial D-dimer measurements using commercial assays with predefined age/sex-specific cutoffs and were followed for up to 2 years. Of 1010 patients, anticoagulation was stopped in 528 (52.3%) with persistently negative D-dimer who subsequently experienced 25 recurrences (3.0% pt-y; 95% confidence interval [CI], 2.0-4.4%). Of the remaining 482 patients, 373 resumed anticoagulation and 109 refused it. Recurrent VTE developed in 15 patients (8.8% pt-y; 95% CI, 5.0-14.1) of the latter group and in 4 of the former (0.7% pt-y; 95% CI, 0.2-1.7; hazard ratio = 2.92; 95% CI, 1.87-9.72; P = .0006). Major bleeding occurred in 14 patients (2.3% pt-y; 95% CI, 1.3-3.9) who resumed anticoagulation. Serial D-dimer measurement is suitable in clinical practice for the identification of VTE patients in whom anticoagulation can be safely discontinued. This study was registered at clinicaltrials.gov as #NCT00954395.
Introduction
Venous thromboembolism (VTE), encompassing deep vein thrombosis (DVT) and pulmonary embolism (PE), tends to recur, especially when the event is idiopathic or associated with a permanent prothrombotic conditions.1 The cumulative rate of recurrence 10 years after withdrawal of anticoagulation was reported to be ∼50% in patients with a first unprovoked VTE and ∼20% after a provoked event.2 Anticoagulation for 3 months is recommended in all VTE patients, whereas indefinite anticoagulation is suggested3 in patients with idiopathic VTE and without high bleeding risk, because the recurrence rate after stopping anticoagulation is independent of the duration of initial treatment.4,5
Altered D-dimer levels after anticoagulation is stopped in patients with a first VTE6 and the persistence of residual vein thrombosis (RVT) after DVT7 have been shown to be a risk factor for recurrence.
We performed a prospective cohort study in outpatients with a single episode of proximal DVT of the lower limbs and/or PE who had received a standard course of anticoagulation (>3 months), or at least 12 months in case of RVT. We sought to assess whether a management procedure involving serial D-dimer testing and RVT assessment can identify a subset of subjects at low risk of recurrence in whom anticoagulation can be safely discontinued.
Methods
Study patients
This was a multicenter, prospective cohort study involving patients of both sexes aged ≥18 years who had experienced a first symptomatic VTE episode, including proximal DVT of the legs, PE, or both, that was either idiopathic or associated with weak risk factors (WRFs; Table 1). The index event was objectively confirmed by compression ultrasonography (CUS), ventilation-perfusion lung scan, or computed tomographic pulmonary angiography (CTPA), as appropriate, and treated according to international guidelines, including acute and long-term anticoagulant therapy and, in the case of DVT, compression elastic stockings (30-40 mm Hg at the ankle). All screened patients were examined to assess for the presence of criteria for exclusion, for short or extended anticoagulation, and finally for inclusion in the study (see detailed criteria in Table 1). Patients were eligible if they had completed at least 3 months of therapy with a vitamin K antagonist (VKA, either warfarin [Coumadin, Bristol-Myers Squibb] or acenocoumarol [Sintrom, Novartis Pharma]), with a target INR of 2.5 (range, 2.0-3.0).
Criteria for exclusion/inclusion in the study
| Inclusion criteria |
| Age ≥18 y |
| First episode of proximal VTE of lower limbs and/or PE that was: |
| idiopathic or associated with one or more of following factors: |
| minor, arthroscopic, or laparoscopic general surgery |
| pregnancy or puerperium |
| contraceptive or replacement hormonal therapy |
| long trip (>6 h) |
| minor trauma (not requiring hospitalization, plaster casting, or immobilization) |
| hospitalization in a medical hospital |
| reduced mobility (not complete immobilization) |
| Anticoagulation therapy (VKA, INR 2.0-3.0) for at least 3 mo |
| Ability to provide informed consent |
| Prespecified criteria for exclusion |
| Age <18 y |
| Duration of anticoagulation <3 mo |
| Inability or refusal to give consent |
| Limited life expectation (<1 y) |
| Increased systolic pulmonary arterial pressure (values ≥35 mm Hg [or ≥40 mm Hg if BMI ≥30 or age ≥75 y] estimated with echocardiography) |
| Geographical inaccessibility |
| Venous thrombosis in different sites (upper limbs, splanchnic veins, jugular or cerebral veins) |
| Pregnancy or puerperium (first 6 weeks after birth) at the time of screening examination |
| Severe renal (creatinine level >2 mg/dL [177 μmol/L]) or liver failure (eg, acute hepatitis, chronic active hepatitis, or cirrhosis; or an alanine aminotransferase level that was 3 times the upper limit of the normal range or higher) |
| Criteria for short anticoagulation |
| VTE post major surgery (within 3 mo) |
| VTE post bed resting (≥4 d) |
| VTE post major trauma (within 3 mo) |
| VTE post plasters or immobilization (within 3 mo) |
| High bleeding risk |
| Criteria for extended anticoagulation |
| >1 documented VTE episode (proximal DVT and/or PE) |
| Active cancer or hematologic disease |
| Antithrombin deficiency |
| Antiphospholipid antibody syndrome (Sydney criteria) |
| PE with shock or life-threatening prolonged hypotension |
| Different indications for anticoagulation |
| Severe cardiorspiratory insufficiency (NYHA 3 or 4) |
| Inclusion criteria |
| Age ≥18 y |
| First episode of proximal VTE of lower limbs and/or PE that was: |
| idiopathic or associated with one or more of following factors: |
| minor, arthroscopic, or laparoscopic general surgery |
| pregnancy or puerperium |
| contraceptive or replacement hormonal therapy |
| long trip (>6 h) |
| minor trauma (not requiring hospitalization, plaster casting, or immobilization) |
| hospitalization in a medical hospital |
| reduced mobility (not complete immobilization) |
| Anticoagulation therapy (VKA, INR 2.0-3.0) for at least 3 mo |
| Ability to provide informed consent |
| Prespecified criteria for exclusion |
| Age <18 y |
| Duration of anticoagulation <3 mo |
| Inability or refusal to give consent |
| Limited life expectation (<1 y) |
| Increased systolic pulmonary arterial pressure (values ≥35 mm Hg [or ≥40 mm Hg if BMI ≥30 or age ≥75 y] estimated with echocardiography) |
| Geographical inaccessibility |
| Venous thrombosis in different sites (upper limbs, splanchnic veins, jugular or cerebral veins) |
| Pregnancy or puerperium (first 6 weeks after birth) at the time of screening examination |
| Severe renal (creatinine level >2 mg/dL [177 μmol/L]) or liver failure (eg, acute hepatitis, chronic active hepatitis, or cirrhosis; or an alanine aminotransferase level that was 3 times the upper limit of the normal range or higher) |
| Criteria for short anticoagulation |
| VTE post major surgery (within 3 mo) |
| VTE post bed resting (≥4 d) |
| VTE post major trauma (within 3 mo) |
| VTE post plasters or immobilization (within 3 mo) |
| High bleeding risk |
| Criteria for extended anticoagulation |
| >1 documented VTE episode (proximal DVT and/or PE) |
| Active cancer or hematologic disease |
| Antithrombin deficiency |
| Antiphospholipid antibody syndrome (Sydney criteria) |
| PE with shock or life-threatening prolonged hypotension |
| Different indications for anticoagulation |
| Severe cardiorspiratory insufficiency (NYHA 3 or 4) |
BMI, body mass index; INR, international normalized ratio; NYHA, New York Heart Association.
Management procedures
All eligible patients were examined after at least 3 months of anticoagulation to assess their conditions for study enrollment. Before inclusion, all patients received a bilateral CUS examination of the proximal deep veins (common femoral, superficial femoral, and popliteal), and those presenting with RVT (>4-mm vein diameter at probe compression in the transverse section8 ) in at least one of the aforementioned veins were included in the study only after completing a total of 12 months of VKA therapy.
All included patients underwent a serial D-dimer assessment starting at baseline during anticoagulation (T0). Patients with positive baseline D-dimer (adopting the criteria indicated next) were instructed to continue anticoagulation, whereas those with negative D-dimer were recommended to stop VKA and to repeat D-dimer testing after 15 to 18 days (T15), 25 to 35 (T30), 55 to 65 (T60), and 85 to 95 (T90) days from T0. Patients were recommended to resume anticoagulation at the first positive D-dimer result.
D-dimer assays and prespecified cutoff values
D-dimer levels were assessed with the quantitative assay routinely used in each participating center, provided that it was one of the following: (1) VIDAS D-dimer Exclusion (bioMerieux, Lyon, France), (2) Innovance D-DIMER (Siemens, Deerfield, IL), (3) HemosIL D-dimer HS (Instrumentation Laboratory, Milan, Italy), (4) HemosIL D-dimer (Instrumentation Laboratory), and (5) STA Liatest D-dimer (DiagnosticaStago, Asnieres-sur-Seine, France). As discussed elsewhere,9 age and sex specific cutoff values were calculated for risk of recurrence and used in the aforementioned tests, instead of those recommended by the manufacturers for VTE exclusion. These specific cutoff values were determined by using stored frozen plasma aliquots collected from the patients included in the Prolong6 and Prolong II10 studies. These aliquots were centralized in the coordinating center laboratory. Two predefinite criteria were adopted to select cutoff values for the assays: (1) the percentage of patients with above cutoff D-dimer after one month from anticoagulation was stopped had to be as close as possible to that obtained in the Prolong study at the same timing (36.7%) and within 95% confidence interval (CI, 32.8-40.6), and (2) the percentage of VTE recurrence in patients with below cutoff D-dimer had to be as low as possible.
The adopted D-dimer cutoffs (Table 2) differed markedly in relation to age and sex. The adopted cutoffs for young males were similar or even lower than those recommended for VTE exclusion; they were slightly higher for young females but noticeably higher for males and females over 70 years.
Age- and sex-specific cutoff levels for the different D-dimer assays adopted in the study
| Commercial D-dimer assay (manufacturer) ng/mL . | Males ≤70 y . | Males >70 y . | Females ≤70 y . | Females >70 y . | Cutoff values currently recommended by manufacturers for VTE exclusion . |
|---|---|---|---|---|---|
| VIDAS D-dimer Exclusion (bio-Merrieux) | 490 | 1050 | 600 | 1300 | 500 |
| Innovance D-DIMER (Siemens) | 500 | 950 | 550 | 1150 | 500 |
| HemosIL D-dimer HS (Instrumentation Laboratory) | 170 | 345 | 215 | 430 | 230 |
| HemosIL D-dimer (Instrumentation Laboratory) | 205 | 300 | 225 | 330 | 230 |
| STA Liatest D-dimer (Diagnostica Stago) | 340 | 700 | 450 | 1050 | 500 |
| Commercial D-dimer assay (manufacturer) ng/mL . | Males ≤70 y . | Males >70 y . | Females ≤70 y . | Females >70 y . | Cutoff values currently recommended by manufacturers for VTE exclusion . |
|---|---|---|---|---|---|
| VIDAS D-dimer Exclusion (bio-Merrieux) | 490 | 1050 | 600 | 1300 | 500 |
| Innovance D-DIMER (Siemens) | 500 | 950 | 550 | 1150 | 500 |
| HemosIL D-dimer HS (Instrumentation Laboratory) | 170 | 345 | 215 | 430 | 230 |
| HemosIL D-dimer (Instrumentation Laboratory) | 205 | 300 | 225 | 330 | 230 |
| STA Liatest D-dimer (Diagnostica Stago) | 340 | 700 | 450 | 1050 | 500 |
For comparison, the cutoff values recommended by manufacturers for VTE exclusion are also shown.
Study outcomes and follow-up
Patients were followed for a maximum of 2 years, and were seen at the clinical centers at intervals of 3 to 6 months, or they were monitored for VKA dosing. Patients were instructed to contact the clinical center immediately in case of symptoms suggestive of VTE or bleeding.
The main study outcome was the composite of confirmed recurrent VTE and death caused by VTE. In cases of suspected DVT recurrence, CUS results were compared with those of the last available previous examination. Any recurrent DVT was adjudicated if a previously fully compressible segment (contralateral or ipsilateral) was no longer compressible or if an increase of at least 4 mm in the diameter of the residual thrombus during compression was detected.8 In patients with suspected PE, recurrence was diagnosed on the basis of objective algorithms11,12 incorporating clinical probability; ventilation-perfusion lung scanning; or CTPA, CUS, and/or D-dimer testing as appropriate. Major bleeding events, defined by the International Society of Thrombosis and Haemostasis,13 were also recorded.
All suspected outcome events and deaths were evaluated by a central adjudication committee whose members were unaware of patient name, D-dimer testing results at inclusion, management, or enrolling center. All patients gave their written informed consent for participation. The institutional review boards of all participating centers approved the study, which was conducted in accordance with the Declaration of Helsinki.
Statistical analysis and sample size
On the basis of a cumulative recurrence rate in patients with provoked VTE of 6.7% after 24 months from VKA suspension,14 we designed the study to have an 80% power to detect a recurrence rate below a clinically acceptable incidence of 9% of the composite end point after 24 months. According to Shen,15 the required sample size in those suspending VKA was 530.
Differences between groups were assessed using the χ2 test with Yates’ correction for categorical variables and the Mann-Whitney U test for continuous variables. Kaplan-Meier survival curves were plotted to estimate the cumulative incidence of symptomatic recurrent VTE; hazard ratios (HR) and their 95% CIs were calculated. The data were analyzed with the use of Prism software (Version 3.0, GraphPad Software Incorporated, San Diego, CA) and SPSS software (version 11.0 SPSS Inc., IBM, Armonk, NY).
Results
Patients and management
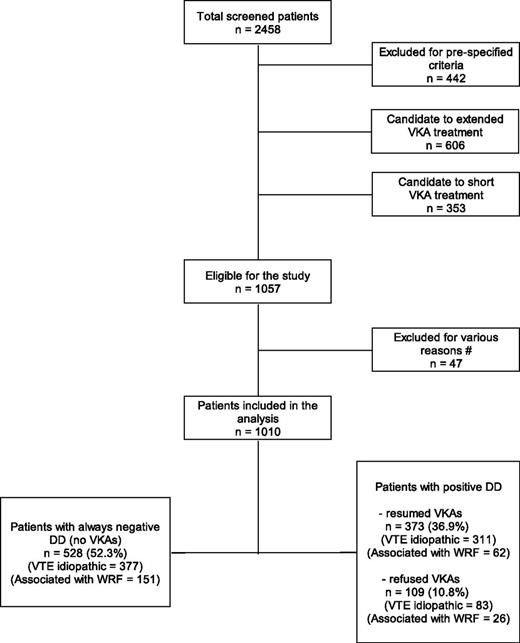
Figure 1 shows the study flow chart. In the 18 participating centers, 2458 patients with a first episode of VTE were screened between July 2008 and December 2011. Of these patients, 1401 (57.0%) were excluded for predefined criteria (442) or for criteria leading to short (353) or extended anticoagulation (606). A total of 1057 patients (43.0% of the screened population) were eligible. Forty-seven (4.4%) patients were then excluded from the study because of consent withdrawal (16) or for conditions requiring continued anticoagulation (27), or they were lost to follow-up after the first D-dimer test (4). The remaining 1010 patients (560 males) followed the management procedure and were analyzed; the index event was idiopathic in 771 (76.3%) patients and was associated with WRF in the remaining 239 (23.7%).
Flow chart of the DULCIS study. The prespecified criteria for exclusion from the study and for short or extended anticoagulant treatment are reported in Table 1. #Patients were excluded for the following reasons: consent withdrawal (16), presented conditions requiring anticoagulation (27), had only the first D-dimer testing, were then lost to follow up (4).
Flow chart of the DULCIS study. The prespecified criteria for exclusion from the study and for short or extended anticoagulant treatment are reported in Table 1. #Patients were excluded for the following reasons: consent withdrawal (16), presented conditions requiring anticoagulation (27), had only the first D-dimer testing, were then lost to follow up (4).
Table 3 shows the characteristics of the analyzed patients. D-dimer was persistently negative (below cutoff levels) in 528 patients (52.3%; 277 males) who stopped anticoagulation and included 15 patients (as intention-to-treat analysis) with incomplete serial D-dimer testing and/or a short follow-up. D-dimer was positive (above cutoffs) in 482 (47.7%) patients (significantly older than those with normal D-dimer) who were advised to resume VKAs at the first positive D-dimer result. However, 109 of these (10.8%, 70 males; 22.6% of all the subjects with positive D-dimer) refused to do so and continued follow-up, whereas the remaining 373 (36.9%; 213 males), significantly older than those who refused, resumed anticoagulation therapy. The prevalence of positive D-dimer was significantly higher in patients with an idiopathic index event (51.1%) than in those with events associated with WRF (36.8%, P < .0001); it was lower (P < .01) in young females (38.3%) than in the other subgroups in which the prevalence ranged between 50.4% and 53.7%. As is shown in Figure 2, the highest rate of positive D-dimer in the whole study population was detected at 15 days (20.8%) after stopping anticoagulation, with an overall positivity of 48.8% at the end of serial testing (at 90 days). A persistent RVT was detected in 119 patients, of whom 56 had negative D-dimer (10.6% of the 528 total patients with persistently negative assay), and 63 had positive D-dimer (13.1% of the 482 patients with positive assay).
Baseline characteristics of the 1010 study patients
| Characteristic . | Negative D-dimer (N = 528) . | Positive D-dimer (N = 482) . | P value . | Positive D-dimer without anticoagulation (N = 109) . | Positive D-dimer with anticoagulation (N = 373) . | P value . |
|---|---|---|---|---|---|---|
| Male sex, n (%) | 277 (52.5) | 283 (58.7) | .055 | 70 (64.2) | 213 (57.1) | .230 |
| Age (y), median (IQ) | 63 (45-75) | 69 (58-79) | <.0001 | 64 (49-72) | 71 (61-80) | <.0001 |
| Age >70 y, n (%) | 201 (38.1) | 223 (46.3) | .011 | 32 (29.3) | 191 (51.2) | <.0001 |
| Type of VTE, n (%) | ||||||
| Proximal DVT with no PE | 285 (54.5) | 244 (51.4) | .384 | 53 (49.1) | 191 (52.0) | .677 |
| DVT plus symptomatic PE | 97 (18.5) | 113 (23.8) | .037 | 26 (24.1) | 87 (23.7) | .968 |
| Isolated PE | 141 (27.0) (5 NA) | 118 (24.8) (7 NA) | .379 | 29 (26.8) (1 NA) | 89 (24.3) (6 NA) | .689 |
| Type of risk factors, n (%) | ||||||
| Idiopathic | 377 (71.4) | 394 (81.7) | <.0001 | 83 (76.1) | 311 (83.4) | |
| WRFs | 151 (28.6) | 88 (18.3) | <.0001 | 26 (23.9) | 62 (16.6) | .115 |
| Minor general, laparoscopic, or arthroscopic surgery | 7 | 2 | 1 | 1 | .115 | |
| Pregnancy or puerperium | 3 | 1 | 1 | 0 | ||
| Hormonal contraceptive replacement therapy | 90 | 30 | 11 | 19 | ||
| 8 | 2 | 1 | 1 | |||
| Long travel | 5 | 8 | 3 | 5 | ||
| Minor trauma, leg injury, reduced mobility | 17 | 20 | 8 | 13 | ||
| Hospitalization in a medical ward | 21 | 27 | 1 | 23 | ||
| Duration of previous anticoagulation, n (%) | ||||||
| ≤6 mo | 160 (30.3) | 141 (29.3) | .784 | 29 (26.6) | 112 (30.0) | .574 |
| 7-12 mo | 297 (56.2) | 272 (56.4) | 1.000 | 61 (56.0) | 211 (56.6) | .999 |
| >12 mo | 71 (13.5) | 69 (14.3) | .786 | 19 (17.4) | 50 (13.4) | .375 |
| Total duration of FU for all patients, y | 829 | 772 | 171 | 601 | ||
| FU, y, median (IQ) | 1.93 (1.25-2.00) | 1.90 (1.29-2.00) | .508 | 1.97 (1.23-2.00) | 1.88 (1.29-2.00) | .990 |
| Duration of FU, n | ||||||
| 2 y | 266 | 239 | 59 | 180 | ||
| 1-2 y | 169 | 165 | 29 | 136 | ||
| <1 y | 57* | 49 | 7 | 42 | ||
| Patients censored during FU, n (%) | 36 (6.8) | 29 (6.0) | .697 | 14 (12.8) | 15 (4.0) | .002 |
| Lost to FU, n (%) | 6 (1.1) | 1 (0.2) | .179 | 1 (0.9) | 0 | .535 |
| Presence of RVT (>4 mm), n (%) | 56 (10.6) | 63 (13.1) | .263 | 5 (4.6) | 58 (15.5) | .005 |
| Associated antiplatelet treatment, n (%) | 53 (10.0) | 42 (8.7) | .553 | 10 (9.2) | 32 (8.6) | .999 |
| Characteristic . | Negative D-dimer (N = 528) . | Positive D-dimer (N = 482) . | P value . | Positive D-dimer without anticoagulation (N = 109) . | Positive D-dimer with anticoagulation (N = 373) . | P value . |
|---|---|---|---|---|---|---|
| Male sex, n (%) | 277 (52.5) | 283 (58.7) | .055 | 70 (64.2) | 213 (57.1) | .230 |
| Age (y), median (IQ) | 63 (45-75) | 69 (58-79) | <.0001 | 64 (49-72) | 71 (61-80) | <.0001 |
| Age >70 y, n (%) | 201 (38.1) | 223 (46.3) | .011 | 32 (29.3) | 191 (51.2) | <.0001 |
| Type of VTE, n (%) | ||||||
| Proximal DVT with no PE | 285 (54.5) | 244 (51.4) | .384 | 53 (49.1) | 191 (52.0) | .677 |
| DVT plus symptomatic PE | 97 (18.5) | 113 (23.8) | .037 | 26 (24.1) | 87 (23.7) | .968 |
| Isolated PE | 141 (27.0) (5 NA) | 118 (24.8) (7 NA) | .379 | 29 (26.8) (1 NA) | 89 (24.3) (6 NA) | .689 |
| Type of risk factors, n (%) | ||||||
| Idiopathic | 377 (71.4) | 394 (81.7) | <.0001 | 83 (76.1) | 311 (83.4) | |
| WRFs | 151 (28.6) | 88 (18.3) | <.0001 | 26 (23.9) | 62 (16.6) | .115 |
| Minor general, laparoscopic, or arthroscopic surgery | 7 | 2 | 1 | 1 | .115 | |
| Pregnancy or puerperium | 3 | 1 | 1 | 0 | ||
| Hormonal contraceptive replacement therapy | 90 | 30 | 11 | 19 | ||
| 8 | 2 | 1 | 1 | |||
| Long travel | 5 | 8 | 3 | 5 | ||
| Minor trauma, leg injury, reduced mobility | 17 | 20 | 8 | 13 | ||
| Hospitalization in a medical ward | 21 | 27 | 1 | 23 | ||
| Duration of previous anticoagulation, n (%) | ||||||
| ≤6 mo | 160 (30.3) | 141 (29.3) | .784 | 29 (26.6) | 112 (30.0) | .574 |
| 7-12 mo | 297 (56.2) | 272 (56.4) | 1.000 | 61 (56.0) | 211 (56.6) | .999 |
| >12 mo | 71 (13.5) | 69 (14.3) | .786 | 19 (17.4) | 50 (13.4) | .375 |
| Total duration of FU for all patients, y | 829 | 772 | 171 | 601 | ||
| FU, y, median (IQ) | 1.93 (1.25-2.00) | 1.90 (1.29-2.00) | .508 | 1.97 (1.23-2.00) | 1.88 (1.29-2.00) | .990 |
| Duration of FU, n | ||||||
| 2 y | 266 | 239 | 59 | 180 | ||
| 1-2 y | 169 | 165 | 29 | 136 | ||
| <1 y | 57* | 49 | 7 | 42 | ||
| Patients censored during FU, n (%) | 36 (6.8) | 29 (6.0) | .697 | 14 (12.8) | 15 (4.0) | .002 |
| Lost to FU, n (%) | 6 (1.1) | 1 (0.2) | .179 | 1 (0.9) | 0 | .535 |
| Presence of RVT (>4 mm), n (%) | 56 (10.6) | 63 (13.1) | .263 | 5 (4.6) | 58 (15.5) | .005 |
| Associated antiplatelet treatment, n (%) | 53 (10.0) | 42 (8.7) | .553 | 10 (9.2) | 32 (8.6) | .999 |
FU, follow-up; IQ, interquartile range; NA, not available.
Fifteen of these patients were included in the analysis (as intention-to-treat), though their serial D-dimer testing was still incomplete (being enrolled late) and/or had a short follow-up.
Prevalence of first-time-ever D-dimer result above the predefined cutoff levels in the investigated study population at the serial measurement days after VKA withdrawal. The percentages are calculated vs the total number of patients included.
Prevalence of first-time-ever D-dimer result above the predefined cutoff levels in the investigated study population at the serial measurement days after VKA withdrawal. The percentages are calculated vs the total number of patients included.
Outcomes
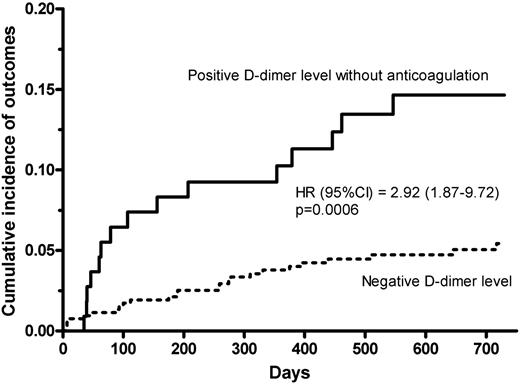
Primary outcomes (Table 4) occurred in 25 of 528 patients with negative D-dimer (4.7%; 95% CI, 3.2-6.9; 3.0 per 100 pt-y, 95% CI, 2.0-4.4) and in 15 of 109 patients who had positive D-dimer results but refused to resume anticoagulation (13.8%; 95% CI, 7.9-21.7; 8.8 per 100 pt-y; 95% CI, 5.0-14.1). The HR of outcome incidence of the latter vs the former was 2.92 (95% CI, 1.87-9.72; P = .0006). The effect of age, sex, and type of index event on the occurrence of primary outcomes in patients who did not resume anticoagulation is shown in Table 5. In patients with negative D-dimer, events were significantly more frequent in those aged >70 years than in younger patients (8.9% vs 2.1%; P = .0008), and in patients with idiopathic than in those with secondary VTE (6.1% vs 1.3%; P = .036), although no differences were present in relation to age and type of index event in patients with positive D-dimer. No difference was detected between males and females, either with negative or positive D-dimer. Thirty of 120 women who received hormonal contraception at the moment of the event (included in the study for this WRF) had positive D-dimer. However, 11 of them refused to resume anticoagulation and there was subsequently one recurrent event in this subgroup (9.1%; 4.9% per 100 pt-y), whereas only one event occurred in the remaining 90 women who always had negative D-dimer (1.1%; 0.65 per 100 pt-y). Four events (1 young male and 3 elderly women, all with negative D-dimer at T0) occurred during the interval before the T15 D-dimer control. In patients with positive D-dimer, there were no differences in age, sex, or type of index event. Among all patients who did not resume anticoagulation, there was no difference in recurrence in those either with or without RVT (5.3% vs 6.3%, respectively) or in those who either received aspirin or did not (6.3% vs 6.2%, respectively).
Clinical events occurred in the investigated patients
| . | Negative D-dimer, no anticoagulation (n = 528; 829 y)* . | Positive D-dimer, anticoagulation refused (n = 109; 171 y)* . | Positive D-dimer, anticoagulation resumed (n = 373; 601 y)* . |
|---|---|---|---|
| Primary outcomes, n, % (95% CI) | 25 (4.7%; 3.2-6.9) | 15 (13.8%; 7.9-21.7)§ | 4 (1.1%; 0.3-2.7) |
| Incidence per 100 pt-y, % (95% CI) | 3.0% (2.0-4.4) | 8.8% (5.0-14.1)¶ | 0.7% (0.2-1.7) |
| Type of event (idiopathic), n | |||
| DVT | 16 (14) | 8 (6) | 1 |
| PE | 5 (5) | 3 (3) | 2 (1) |
| DVT+PE | 4 (3) | 4 (2) | 1 |
| Other outcomes, n | |||
| Death† | 1 | 0 | 5 |
| Isolated distal DVT | 9 | 2 | 0 |
| SVT | 19 | 2 | 2 |
| Arterial vascular event | 3 | 0 | 1 |
| Major bleeding, n, % (95% CI) | 0 | 0 | 14‡ (3.7%; 2.1-6.2) |
| Incidence per 100 pt-y, % (95% CI) | 2.3% (1.3-3.9) |
| . | Negative D-dimer, no anticoagulation (n = 528; 829 y)* . | Positive D-dimer, anticoagulation refused (n = 109; 171 y)* . | Positive D-dimer, anticoagulation resumed (n = 373; 601 y)* . |
|---|---|---|---|
| Primary outcomes, n, % (95% CI) | 25 (4.7%; 3.2-6.9) | 15 (13.8%; 7.9-21.7)§ | 4 (1.1%; 0.3-2.7) |
| Incidence per 100 pt-y, % (95% CI) | 3.0% (2.0-4.4) | 8.8% (5.0-14.1)¶ | 0.7% (0.2-1.7) |
| Type of event (idiopathic), n | |||
| DVT | 16 (14) | 8 (6) | 1 |
| PE | 5 (5) | 3 (3) | 2 (1) |
| DVT+PE | 4 (3) | 4 (2) | 1 |
| Other outcomes, n | |||
| Death† | 1 | 0 | 5 |
| Isolated distal DVT | 9 | 2 | 0 |
| SVT | 19 | 2 | 2 |
| Arterial vascular event | 3 | 0 | 1 |
| Major bleeding, n, % (95% CI) | 0 | 0 | 14‡ (3.7%; 2.1-6.2) |
| Incidence per 100 pt-y, % (95% CI) | 2.3% (1.3-3.9) |
SVT, superficial vein thrombosis.
Total follow-up.
No death could be attributed to thrombotic event.
1 major bleeding was fatal.
P = .0008 patients with negative D-dimer.
P < .0009 vs patients with negative D-dimer.
Cumulative rates (no. per 100 patient-years) of primary study outcomes in relation to age, sex, and type of index event in patients who did not resume anticoagulation
| . | Age . | Sex . | Type of index event . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| . | ≤70 y . | >70 y . | P value . | Males . | Females . | P value . | Idiopathic . | WRF . | P value . |
| Patients with negative D-dimer, n (%) | 327 (61.9) | 201 (38.1) | 277 (52.2) | 251 (47.8) | 377 (71.4) | 151 (28.6) | |||
| Primary outcomes, % (95% CI) | 2.1 (0.9-4.4) | 8.9 (5.4-13.8) | .0008 | 4.7 (2.5-7.9) | 4.8 (2.5-8.2) | .886 | 6.1 (3.9-9) | 1.3 (0.2-4.7) | .036 |
| Patients with positive D-dimer who did not resume anticoagulation n (%) | 77 (70.6) | 32 (29.4) | 70 (64.2) | 39 (35.8) | 83 (76.1) | 26 (23.9) | |||
| Primary outcomes, % (95% CI) | 14.3 (7.4-24.1) | 12.5 (3.5-29.0) | .956 | 10.0 (4.1-19.5) | 20.5 (9.3-36.5) | .220 | 15.7 (8.6-25.3) | 7.7 (1.0-25.1) | .483 |
| . | Age . | Sex . | Type of index event . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| . | ≤70 y . | >70 y . | P value . | Males . | Females . | P value . | Idiopathic . | WRF . | P value . |
| Patients with negative D-dimer, n (%) | 327 (61.9) | 201 (38.1) | 277 (52.2) | 251 (47.8) | 377 (71.4) | 151 (28.6) | |||
| Primary outcomes, % (95% CI) | 2.1 (0.9-4.4) | 8.9 (5.4-13.8) | .0008 | 4.7 (2.5-7.9) | 4.8 (2.5-8.2) | .886 | 6.1 (3.9-9) | 1.3 (0.2-4.7) | .036 |
| Patients with positive D-dimer who did not resume anticoagulation n (%) | 77 (70.6) | 32 (29.4) | 70 (64.2) | 39 (35.8) | 83 (76.1) | 26 (23.9) | |||
| Primary outcomes, % (95% CI) | 14.3 (7.4-24.1) | 12.5 (3.5-29.0) | .956 | 10.0 (4.1-19.5) | 20.5 (9.3-36.5) | .220 | 15.7 (8.6-25.3) | 7.7 (1.0-25.1) | .483 |
Among the patients with positive D-dimer who did not resume anticoagulation, the rate of recurrence was higher in those whose D-dimer became positive within one month from VKA withdrawal than in those whose D-dimer became positive later; however, the difference did not reach statistical difference, probably owing to the low number of cases (13/77 [16.9%] vs 2/32 [6.2%], P = .247; the 2 subjects with late-positive D-dimer who recurred were both young).
In patients who resumed anticoagulation after a positive D-dimer result, 4 thrombotic events (1.1%; 95% CI, 0.3-2.7; 0.7 per 100 pt-y, 95% CI, 0.2-1.7) and 14 major hemorrhages (fatal in 1) (3.7%, 95% CI, 2.1-6.2; 2.3 per 100 pt-y, 95% CI, 1.3-3.9) occurred. The rate of bleeding was higher in elderly (4.7%) than in younger (2.7%) patients, but the difference was not significant (P = .460).
Discussion
Our study shows that a management procedure based on repeated D-dimer testing can be used in patients with a single VTE event that is either idiopathic or associated with WRFs to identify those with a low risk of recurrence and in whom anticoagulation can be discontinued. Anticoagulation was withdrawn on the basis of D-dimer tests persistently below age- and gender-specific cutoffs in >50% of patients, in whom the subsequent annual recurrence rate was 3%. The recurrence rate in the present study was below the rates recommended as acceptable by the Subcommittee on Control of Anticoagulation of the International Society on Thrombosis and Haemostasis to justify stopping anticoagulant therapy (5% at 1 year and 15% at 5 years, with an upper boundary limit of 8% at 1 year).16
In our study, all the screened patients underwent investigation for the presence of RVT before inclusion, and those with RVT were included only after completing one year of anticoagulation. RVT has long been considered a predictor of recurrence17-19 and a criterion to guide the duration of anticoagulation.7,20 A recent systematic review of available studies21 found that RVT is associated with a significant, albeit modest, increase in the risk of recurrent VTE in patients with (unprovoked or provoked) DVT. The authors concluded that the role of RVT in assessing the risk of recurrent VTE after stopping anticoagulation in patients with unprovoked DVT remains unclear and warrants further investigations. Although the present study was not designed to give an answer to the issue of whether detecting RVT may help guide the duration of anticoagulation, we decided to give patients with RVT a period of anticoagulation long enough (1 year) to achieve a steady-state thrombus condition before starting D-dimer measurements. Of interest, in our cohort patients who did not resume anticoagulation, we failed to show any appreciable difference in recurrence rates between those with and without RVT.
Regarding D-dimer measurement, the current study had important differences from the previous and similar Prolong and Prolong II studies,6,10 in which the same assay (qualitative and calibrated for VTE exclusion) was used in all participating centers. In the present study, centers used their routine commercial quantitative assay, but with age- and sex-specific cutoffs. D-dimer levels increase with age22-24 and are higher in women.25 Compared with the cutoff levels recommended by manufacturers for VTE exclusion, those set for this study were much higher in elderly patients, but were similar or even lower in younger patients, especially in men. As a result, more elderly patients discontinued anticoagulation, whereas the opposite was true for younger patients, especially males. This effect, together with the higher thrombosis risk associated with age, may account for the higher recurrence rate in elderly than in younger patients. Lower cutoff levels might have further lowered the recurrence rate in elderly patients; however, this would have been offset in part by an increase in the proportion of those to be anticoagulated indefinitely, with the associated bleeding risk. Although the cutoff levels adopted in the present study for young subjects proved to be very effective, we believe that a refinement in the cutoff levels for elderly patients is advisable to optimize the relationship between an acceptable rate of recurrence and the proportion of anticoagulated patients. We currently cannot indicate specific cutoff values, different from those used in the study, to be recommended for managing this patient population, and we propose this issue as an important target for future clinical studies.
In the Prolong study, D-dimer was tested only once at one month after VKA interruption,6 whereas in the Prolong II study, patients whose D-dimer levels became abnormal beyond one month after VKA withdrawal had a higher risk of recurrence.10 As is shown in Figure 2, the highest rate of positive D-dimer tests was detected after 15 days (20.8%), with 13.1% positive results at 30 days after VKA withdrawal and another 10% positive results afterward. Among the patients who refused to resume anticoagulation, the recurrence rate in those whose D-dimer became positive after one month (2 cases, both young patients) was lower but not statistically different than in those with earlier positive results. Although we may suggest omitting the D-dimer measurement during anticoagulation (T0) in clinical practice (4 very early recurrences could not be avoided after a negative D-dimer at T0), we believe that the present results confirm the validity of extending D-dimer assessment beyond one month to increase the protection from recurrence, especially in young patients.
The risk of recurrent VTE has consistently been found to be higher in men than in women.26-30 In our study, the difference in the recurrence rate between men and women disappeared when the comparison was made separately among patients with or without positive D-dimer (Table 5). This suggests that D-dimer is an important marker of recurrent thromboembolism and has the potential to compensate for the difference in the gender-related recurrence risk once a proper adjustment of cutoff levels is performed.
Patients were invited to prolong or resume anticoagulation as soon as the D-dimer test result was positive. However, approximately one-fifth of patients refused to resume VKA, and their recurrence rate was about threefold higher than in patients with persistently negative D-dimer (Figure 3). Patients with positive D-dimer who refused to resume anticoagulation were significantly younger than those who agreed to resume anticoagulation, thus showing that young patients with a first VTE are more reluctant to accept an indefinite anticoagulation; no other significant differences could be detected between these 2 groups (Table 3). These results provide further compelling evidence that D-dimer testing can be used to distinguish patients with a high recurrence risk.
Kaplan-Meier cumulative event rates for the primary efficacy outcome in patients with persistently negative D-dimer results in whom anticoagulation was definitively stopped (dotted line) and in those with positive D-dimer results who refused to resume anticoagulation (continuous line).
Kaplan-Meier cumulative event rates for the primary efficacy outcome in patients with persistently negative D-dimer results in whom anticoagulation was definitively stopped (dotted line) and in those with positive D-dimer results who refused to resume anticoagulation (continuous line).
The risk of recurrence is higher after idiopathic events1,2 ; however, it is not negligible when the events are associated with WRFs. In fact, Iorio et al showed a recurrence rate of 4.2% patient-years in subjects whose index event was secondary to nonsurgical risk factors.14 The proportion of patients with VTE events associated with WRFs is generally relevant (one-fourth of all included patients in our study) and it is important to give them justified clinical advice. This is why our study included patients with either idiopathic events or events associated with WRFs, because we intended to propose and analyze the efficacy and safety of a practical model to manage the duration of anticoagulation in patients after a first VTE event. Our study showed that the majority of the patients with an index event associated with a WRF (64.4%) had negative D-dimer and stopped anticoagulation. As expected, among the patients with positive D-dimer who did not resume anticoagulation, the rate of recurrence was almost twice as high in patients with an idiopathic event as in those with WRFs; however, among the latter patients, the rate of recurrence was higher in those with positive than in those with negative D-dimer (Table 5; the difference did not reach statistical significance, probably for the limited number of patients). Furthermore, among young women who had a VTE during hormonal contraception, a population usually considered at low risk, one case of recurrence occurred among the 11 of those with positive D-dimer who did not resume anticoagulation, and only one recurrence occurred among the 90 of them with negative D-dimer (9.1% vs 1.1%). These results, while confirming the higher risk of recurrence when the index VTE event is idiopathic, also indicate that D-dimer can be useful to evaluate the risk of recurrence in individual patients with nonidiopathic VTE.
Among the 373 patients who resumed anticoagulation, 4 experienced VTE events (1.1%) (mainly in association with temporary interruption of anticoagulation), and 14 (3.7%) had major bleeding events (1 fatal) during follow-up. Thus, the cumulative rate of harmful events associated with anticoagulation in these subjects was not different from that observed in patients with negative D-dimer who discontinued anticoagulation. This further supports the benefit of identifying patients at lower risk of recurrence in whom anticoagulation can be discontinued.
The most innovative aspects of the management procedure adopted in this study also have potential limitations. First, serial D-dimer testing may be inconvenient for both patients and physicians; to simplify this approach, we suggest the omission of testing during anticoagulation (T0), but we still advise to repeat D-dimer measurement beyond one month after anticoagulation is stopped. Second, some patients, especially younger ones, can disagree with prolonging or resuming anticoagulation based only on a single blood test result. Third, the age and sex-specific D-dimer cutoff levels adopted in this study for patients aged >70 years were substantially high (twice as high as the upper normal limit indicated for diagnostic purposes). This may generate some confusion in professionals used to the cutoffs established for VTE exclusion and may raise perplexity in labeling as negative such high results. Finally, repeating the D-dimer assay in the first 3 months after anticoagulation is stopped, using cutoff values different than those for VTE exclusion, may generate confusion in professionals, especially in the case of VTE recurrence suspicion during this period.
In conclusion, our study showed that, based on persistently normal D-dimer tests, anticoagulation could be stopped in >50% of patients included after a single idiopathic VTE or associated with WRFs; the recurrence rate during follow-up was as low as 3.0 per 100 pt-y (95% CI, 2.0-4.4), which is below the rates recommended as acceptable to justify anticoagulation discontinuation.16
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The Italian Federation of Anticoagulation Clinics (FCSA) supported this study by inviting the affiliated centers to take part in the study and by organizing and supporting the meetings necessary to start and finalize the study. The Department of Angiology and Blood Coagulation of University Hospital of Bologna supported the collection and analysis of the data
Authorship
Contribution: All authors contributed to the design of the study; B.C., V.D.M., A.G., D.P., S.T., and A.T. contributed to data collection; B.C., E.A., and C.L. contributed to data analysis; all authors contributed to the interpretation of the data collected; and G.P. wrote the first draft of the manuscript, and all the authors contributed to its final changes.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
A full list of study investigators can be found in the Appendix.
Correspondence: Gualtiero Palareti, Department of Angiology & Blood Coagulation, University Hospital Policlinico S. Orsola-Malpighi, Via Albertoni 15, 40138 Bologna, Italy; e-mail: gualtiero.palareti@unibo.it.
Appendix
The following were members of the DULCIS study group (the numbers of patients who participated in the study appear in parentheses): Gualtiero Palareti, Benilde Cosmi, Cristina Legnani, Divisione di Angiologia e Malattie della Coagulazione, Azienda Ospedaliero–Universitaria di Bologna, Policlinico S. Orsola–Malpighi, Bologna, Coordinator Center (270); Nicoletta Erba, Valeria De Micheli, U.O. Patologia Clinica, Azienda Ospedaliera provincia di Lecco (139); Angelo Ghirarduzzi, Maria Rosaria Veropalumbo, Ugolotti Maria Chiara, Angiologia, ASMN-IRCCS–Reggio Emilia, Reggio Emilia (126); Daniela Poli, Domenico Prisco, Emilia Antonucci, Malattie Aterotrombotiche, AOU–Careggi, Firenze (114); Sophie Testa, Oriana Paoletti, Centro Emostasi e Trombosi, AO Istituti Ospitalieri, Cremona (87); Alberto Tosetto, Divisione Ematologia, Ospedale S. Bortolo ULSS 6–Vicenza (54); Anna Falanga, Teresa Lerede SIMT Centro Emostasi e Trombosi Ospedali Riuniti di Bergamo (48); Steidl Luigi, Marco Donadini, Elena Rancan, Medicina Interna 1°–Ambulatorio Emostasi e Trombosi, Ospedale Di Circolo-Università dell'Insubria, Varese (42); Roberto Quintavalla, Piera Maria Ferrini, Medicina Interna a d indirizzo Angiologico e Coagulativo, Ospedale Maggiore Azienda Ospedaliero–Universitaria di Parma (36); Rita C. Santoro, Centro Emofilia Emostasi e Trombosi, Az. Osp. “Pugliese-Ciaccio”, Catanzaro (34); Francesco Orlandini, Raffaella Benedetti, Medicina Interna, Osp. Civile S.Andrea–ASL 5 presidio Levante Ligure, La Spezia (32); Marco Cattaneo, Federico Lussana, Elena Bertinato, Medicina III, A.O. San Paolo–Università di Milano, Milano (28); Roberto Cappelli, Medicina Interna 2, Azienda Ospedaliero–Universitaria Senese, Siena (21); Attilia Maria Pizzini, Medicina 1° Centro Emostasi e Trombosi, Ospedale Santa Maria Nuova, Reggio Emilia (20); Lucia Angeloni, Geriatria, Ospedale Maggiore Bologna (10); Armando D’Angelo, Luciano Crippa, Ambulatorio Emostasi e Trombosi, Ospedale S. Raffaele, Milano (10); Roberta Bortolotti, Medicina, Ospedale di San Giovanni Persiceto, Bologna (8); Maria Rita Vandelli, Med. Cardiovascolare–Mod. Organizzativo Angiologia, Centro Trombosi, Nuovo Ospedale Civile S. Agostino Estense, Baggiovara Modena (4). Executive Committee: Gualtiero Palareti (Bologna), Vittorio Pengo (Padova), Paolo Prandoni (Padova); Steering Committee: Walter Ageno (Varese), Angelo Ghirarduzzi (Reggio Emilia), Domenico Prisco (Firenze), Sophie Testa (Cremona), Alberto Tosetto (Vicenza), Armando Tripodi (Milano); Adjudication Committee: Davide Imberti (Piacenza), Marco Moia (Milano), Raffaele Pesavento (Padova); External Safety Committee: Nicola Magrini (Bologna), Francesco Marongiu (Cagliari), Pietro Zonzin (Rovigo); Scientific Secretariat: Benilde Cosmi (Bologna); referent for laboratory issues: Cristina Legnani (Bologna); data manager (collection and processing): Noemi Piaggesi (Bologna); data analysis: Benilde Cosmi (Bologna), Daniela Poli (Firenze), Mauro Silingardi (Reggio Emilia).


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal