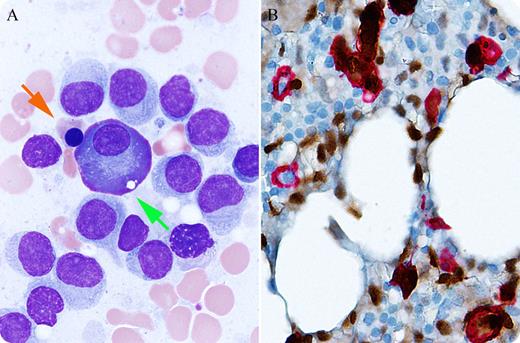
A 65-year-old man, with no previous significant complete blood count findings and no preexisting concern for hematopoietic malignancy, presented for baseline bone marrow evaluation as a potential donor for hematopoietic stem cell (HSC) transplant for his brother, a patient with mantle cell lymphoma (cyclin D1+). Marrow aspirate smear (panel A) revealed 7% myeloid precursors, 36% erythroid precursors (orange arrow), 52% lymphoid cells (un-annotated cells), and 5% plasma cells (green arrow). The vast majority of lymphocytes exhibited a moderate amount of pale cytoplasm with fluffy projections, round-to-oval bland nuclei, and inconspicuous nucleoli, indicative of hairy cells. Plasma cells were predominantly larger than normal, some exhibiting prominent nucleoli. The normocellular marrow biopsy showed extensive interstitial lymphoid infiltrate morphologically and immunophenotypically diagnostic of hairy cell leukemia (positive for pan–B-cell markers, CD25, Annexin A1, and TRAP). There was also an increase in atypical plasma cells (10%-20%) with focal clustering/sheeting, most consistent with asymptomatic plasma cell myeloma because close monitoring detected no serum paraprotein or signs of end-organ damage. Dual immunohistochemical staining with cyclin D1 (brown) and CD138 (red) (panel B) demonstrated that both hairy cell leukemia (cyclin D1+/CD138–) and atypical plasma cells (cyclin D1+/CD138+) were positive for cyclin D1, with few normal plasma cells (cyclin D1–/CD138+).
In this potential donor for hematopoietic stem cell transplant, routine bone marrow biopsy evaluation revealed findings indicative of a presence of synchronous hairy cell leukemia and plasma cell myeloma, a rare observation.
A 65-year-old man, with no previous significant complete blood count findings and no preexisting concern for hematopoietic malignancy, presented for baseline bone marrow evaluation as a potential donor for hematopoietic stem cell (HSC) transplant for his brother, a patient with mantle cell lymphoma (cyclin D1+). Marrow aspirate smear (panel A) revealed 7% myeloid precursors, 36% erythroid precursors (orange arrow), 52% lymphoid cells (un-annotated cells), and 5% plasma cells (green arrow). The vast majority of lymphocytes exhibited a moderate amount of pale cytoplasm with fluffy projections, round-to-oval bland nuclei, and inconspicuous nucleoli, indicative of hairy cells. Plasma cells were predominantly larger than normal, some exhibiting prominent nucleoli. The normocellular marrow biopsy showed extensive interstitial lymphoid infiltrate morphologically and immunophenotypically diagnostic of hairy cell leukemia (positive for pan–B-cell markers, CD25, Annexin A1, and TRAP). There was also an increase in atypical plasma cells (10%-20%) with focal clustering/sheeting, most consistent with asymptomatic plasma cell myeloma because close monitoring detected no serum paraprotein or signs of end-organ damage. Dual immunohistochemical staining with cyclin D1 (brown) and CD138 (red) (panel B) demonstrated that both hairy cell leukemia (cyclin D1+/CD138–) and atypical plasma cells (cyclin D1+/CD138+) were positive for cyclin D1, with few normal plasma cells (cyclin D1–/CD138+).
In this potential donor for hematopoietic stem cell transplant, routine bone marrow biopsy evaluation revealed findings indicative of a presence of synchronous hairy cell leukemia and plasma cell myeloma, a rare observation.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal