To the editor:
The Janus kinase 2 (JAK2) V617F mutation is known to provide a growth and survival advantage to the affected clones of hematopoetic cells. It may result in clinical phenotypes of polycythemia vera, essential thrombocythemia, and primary myelofibrosis. Although constitutive JAK2 activation is largely responsible for developing myeloproliferative neoplasms (MPNs), an exaggeration of hematopoiesis might be beneficial to a preexisting cytopenic disorder. We report a case of normalization of thrombocytopenia in a patient with Gaucher disease upon the emergence of a JAK2 mutation.
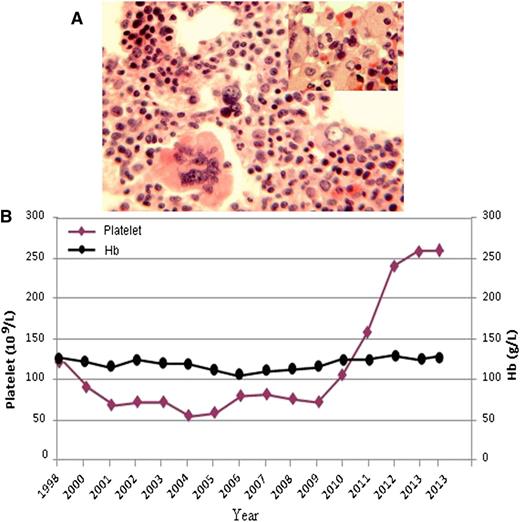
The patient initially presented at the age of 69 years with mild thrombocytopenia and splenomegaly. Gaucher disease type 1 (GD1) was diagnosed based on the findings of Gaucher cells in the bone marrow, a β-glucosidase level of 1.9 nm/mg per hour (normal 8-16), and a genotype of homozygous N370S mutation in the lysosomal glucocerebrosidase gene (GBA1). Clinically, he has remained well over a period of 17 years. The platelet count declined gradually during the first 7 years after the diagnosis. There was no indication of hematologic or autoimmune disease. Interestingly, without any treatment, the platelet count rose gradually over the past 3 years and reached a normal level (Figure 1B). There was no significant change in hemoglobin level and leukocytes, and no significant change in spleen volume as determined by imaging studies during the disease course. The possibility of JAK2 mutation was considered as the cause of rising platelets. Polymerase chain reaction–based assay with allele-specific primers confirmed the presence of the V617F mutation; the allele burden of the JAK2 mutation was estimated at 19% by semiquantitative method. The bone marrow showed normal cellularity (hematopoietic cells in 50% of the marrow cavity) with residual Gaucher cells, a moderate increase in megakaryopoiesis, but no increase in reticulin or fibrotic changes (Figure 1A). Staining for iron showed increased iron stores (4/6) and no ringed sideroblasts. With no thrombocytosis and no evidence of marrow fibrosis, the patient did not meet the diagnostic criteria for essential thrombocythemia or myelofibrosis.
(A) Bone marrow biopsy showed normal cellularity, trilineage hematopoiesis, and all stages of maturation. Megakaryocytes are moderately increased in number, and some appeared with nuclear hyperlobulation; the inset shows a small cluster of characteristic Gaucher cells. (B) Changes in platelet count and hemoglobin level during the course of Gaucher disease.
(A) Bone marrow biopsy showed normal cellularity, trilineage hematopoiesis, and all stages of maturation. Megakaryocytes are moderately increased in number, and some appeared with nuclear hyperlobulation; the inset shows a small cluster of characteristic Gaucher cells. (B) Changes in platelet count and hemoglobin level during the course of Gaucher disease.
Patients with GD1 have been found to have a 3.45- to 12.7-fold risk of developing hematologic malignancies, with a particularly high incidence of multiple myeloma and lymphoma.1,2 Webb et al first reported the JAK2 V617F mutation in a GD1 patient who developed a myeloproliferative/myelodysplastic neoplasm that progressed rapidly to advanced myelofibrosis.3 There was also a report of a false-positive JAK2 V617F leading to diagnosis of Gaucher disease.4 Therefore, testing for JAK2 V617F and other mutations associated with MPN may be useful for investigation of unexpected changes in patients with GD1 to confirm the cause when there are suggestive clinical features.
Thrombocytopenia is one of the most common features of GD1. The mechanism is a combination of hypersplenism and reduced normal hematopoiesis attributable to marrow infiltration.5 Thrombocytopenia may improve with specific treatment of Gaucher disease, such as enzyme therapy. In our patient, the platelet count was normalized with the emergence of JAK2 V617F and an increase in megakaryopoiesis. The patient would appear to have essential thrombocythemia superimposed on Gaucher disease.
Authorship
Contribution: D.A. took care of the patient, conceived the concept, and wrote the manuscript; and C.W. reviewed bone marrow, collected and analyzed the data, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Chen Wang, Department of Pathology and Laboratory Medicine, Mount Sinai Hospital, 600 University Ave, Toronto, ON M5G 1X5, Canada; e-mail: cwang@mtsinai.on.ca.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal