Key Points
Efficacy of imatinib in steroid-refractory chronic GVHD was prospectively compared across 3 different response systems, with high agreement.
Validity of quantitative-based assessment of response with NIH criteria was confirmed by its prognostic impact on long-term survival.
Abstract
Forty adults aged 28 to 73 years were entered into a prospective trial of imatinib for the treatment of steroid-refractory chronic graft-versus-host disease (SR-cGVHD). After 6 months, intention-to-treat (ITT) analysis of 39 patients who received the drug, regardless of the duration of treatment, revealed 14 partial responses (PR), 4 minor responses (MR) with relevant steroid sparing (46%) according to Couriel criteria, and 20 ≥ PR (51.3%), as per the National Institutes of Health (NIH) criteria and NIH severity score changes. The best responses were seen in the lungs, gut, and skin (35%, 50%, and 32%, respectively). After a median follow-up of 40 months, 28 patients were alive, with a 3-year overall survival (OS) and event-free survival of 72% and 46%, respectively. The 3-year OS was 94% for patients responding at 6 months and 58% for nonresponders according to NIH response, suggesting that these criteria represent a reliable tool for predicting OS after second-line treatment. Monitoring of anti–platelet-derived growth factor receptor (PDGF-R) antibodies showed a significant decrease in PDGF-R stimulatory activity in 7 responders, whereas it remained high in 4 nonresponders. This study confirms the efficacy of imatinib against SR-cGVHD and suggests that the response at 6 months significantly predicts long-term survival. This study is registered at https://eudract.ema.europa.eu/ (EUDRACT number: 2009-012927-27).
Introduction
Treatment for steroid-refractory chronic graft-versus-host disease (SR-cGVHD) represents an unmet challenge. The National Institutes of Health (NIH) consensus on chronic graft-versus-host disease (cGVHD) has defined SR-cGVHD as: progression despite treatment with prednisone 1 mg/kg per day for ≥2 weeks or no improvement after 4 to 8 weeks of prednisone 0.5 mg/kg per day, or the inability to taper prednisone below 0.5 mg/kg per day.1
The NIH consensus has also defined the global cGVHD severity scores as mild, moderate, and severe, the last having the worst outcome.2,3 Skin sclerosis is associated with poor functional status,4,5 poor quality of life, and the need for prolonged immunosuppressive therapy.6
Extracorporeal photopheresis (ECP) has been shown to have a significant effect on skin SR-cGVHD, with a consistent steroid-sparing effect; however, there is no evidence of improved outcome.7 In this setting, pentostatin has achieved promising results, albeit at the price of increased fungal infections.8 Imatinib showed promising responses in 2 small cohorts of patients with SR-cGVHD, without major toxicities9,10 ; other studies have shown less favorable results.11-13 Imatinib is a potent dual inhibitor of both transforming growth factor-β and platelet-derived growth factor receptor (PDGF-R) pathways14 ; these 2 cytokines are both involved in the fibrogenic and inflammatory processes of several fibrotic diseases,15 as suggested by a murine model of cGVHD16 and by recent data on cGVHD with fibrotic features (ScGVHD) and systemic scleroderma (SS).17,18 Moreover, imatinib inhibits T-cell proliferation,19 as suggested by clinical improvement in patients with chronic myelogenous leukemia and concomitant autoimmune diseases who are receiving imatinib treatment.20
Patients with ScGVHD have stimulating anti–PDGF-R antibodies as in SS, suggesting a similar pathogenetic mechanism.17,18 However, the role of these antibodies is still debatable, and in a recent study of 15 cGVHD patients receiving imatinib, the presence of anti–PDGF-R antibodies did not correlate with outcome.12
A major limitation of results from different trials on SR-cGvHD is the lack of standardized response criteria. Despite a considerable effort made by the NIH consensus21 to create a uniform response evaluation, this is often based on physician assessment, with considerable variability in measures and a lack of reproducibility.7,8,22,23
Patients and methods
Study design
This prospective, multicenter phase 2 study aimed to evaluate the safety and efficacy of imatinib in patients with SR-cGVHD. The protocol was approved by the coordinating center of Potenza Hospital’s ethical committee (EUDRACT number: 2009-012927-27) and at all participating sites. This study was conducted in accordance with the Declaration of Helsinki and was supported by AIFA (Italian Drugs Agency, CODE: FARM7ZWZ7Y).
The primary end points were as follows: (1) overall response rate (ORR) after 6 months of treatment with imatinib, evaluated according to the Couriel and NIH criteria21-23 ; and (2) acute and long-term toxicity of grade >2, evaluated according to the World Health Organization (WHO) scale.
The secondary end points were as follows:
(a) Overall survival (OS) and event-free survival (EFS). OS was measured from the initiation of imatinib until death, whereas EFS was measured from the initiation of imatinib until death, secondary neoplasia, or treatment failure. Treatment failure was defined as cGVHD progression or death because of cGVHD; relapse of the underlying disease; addition (or increase) of immunosuppressive drug/procedure, excluding a brief, transient steroid dose increase in the event of a GVHD flare21 ; or severe toxicity (grade 3-4 according to the common toxicity criteria [CTC]), requiring permanent discontinuation of imatinib.
(b) Response duration (RD), which was defined as time to loss of response (ie, no response according to Couriel criteria) in patients achieving ≥ minor response/stable disease (MR/SD) at 6 months, according to the Couriel criteria. Among patients with SD, only those with stable pulmonary function and a >50% decrease in steroid dose were included.22
(c) Changes in the NIH cGVHD global and organ-specific severity score during imatinib treatment.2,3,24
(d) Evaluation of stimulating anti–PDGF-R antibodies at baseline and during treatment to assess the correlation with the response to imatinib.
Statistical analysis
Using the Simon 2-stage, mini-max design, on the basis of the results of previous experimental treatment of SR-cGVHD,1 we set a minimal ORR (according to Couriel22,23 ) of 30% (p0) and an expected ORR of 50% (p1). Nineteen patients were recruited in the first stage, with an early stopping rule for futility if fewer than 7 responses occurred and a toxicity stopping rule if >1 death occurred potentially correlated to the treatment. In the second step, 20 more patients were to be recruited. This design yields a type I error probability of 0.05 (α) and a power of 0.80 (1-β); the true response rate is likely to be higher than 30% (p0) if at least 17 of 39 patients exhibit a response.25
Data were analyzed using the Stata 12.0 package (StataCorp, College Station, TX) and Microsoft Excel (Microsoft Corporation, Redmond WA). Actuarial curves were plotted using the Kaplan-Meier method.26 Univariate analyses for the outcome of OS were conducted for all the baseline characteristics reported in Table 1. All reported P values in the text are 2-tailed (α = .05).
Baseline characteristics of the 40 enrolled patients
| Patient characteristics (n = 40) | |
| Gender (female/male), n (%) | 12/28 (32%/68%) |
| Age (y), Median (range) | 48 (28–73) |
| Disease, n (%) | |
| Myeloproliferative disorders: CML/MF/MDS | 3/1/1 (12%) |
| MM | 8 (20%) |
| Lymphoproliferative disorders: NHL/HD/CLL | 5/2/0 (18%) |
| Others: solid tumor | 1 (2%) |
| Transplant, n (%) | |
| MUD | 8 (20%) |
| HLA identical sibling | 32 (80%) |
| PBSC | 30 (75%) |
| BM | 10 (25%) |
| Conditioning regimen, including TBI | 17 (44%) |
| cGVHD | |
| Duration (mo), median (range) | 26 (3–148) |
| Risk score27 (high/intermediate/low), n | 24/15/1 |
| First-line therapy, n | |
| Prednisone (alone or with other drugs) | 36 |
| Miscellaneous (including MMF, tacrolimus, ECP, CSA) | 4 |
| Second and successive lines of therapy, n | |
| Rituximab + miscellaneous (no ECP) | 5 |
| Rituximab + ECP ± miscellaneous | 8 |
| Miscellaneous, including ECP (no rituximab) | 8 |
| Miscellaneous, excluding ECP and rituximab | 19 |
| Karnofsky performance status at enrollment, n (%) | |
| <70 | 28 (70%) |
| 80 | 9 (22%) |
| 90–100 | 3 (8%) |
| Platelet count before imatinib initiation, 109/L, n (%) | |
| <100 | 2 (5%) |
| >100 | 38 (95%) |
| Main cGVHD targets (different organ involvements are not mutually exclusive) | |
| Skin, n (%) | 32 (80%) |
| Mean affected BSA% for erythematous/moveable/nonmoveable sclerosis | 19/27/27 |
| Lung, n (%) | 33 (82.5%) |
| Median values of FEV1/DLCO | 61/55 |
| Mouth, n (%) | 23 (57.5%) |
| Median Schubert Scale value | 3 |
| Liver, n (%) | 6 (15%) |
| Median values of ALT (U/L)/total bilirubin (mg/dL) | 74/3.0 |
| Gut, n (%) | 9 (22.5%) |
| Mean value of the GI scale (0-3) | 1.5 |
| Patient characteristics (n = 40) | |
| Gender (female/male), n (%) | 12/28 (32%/68%) |
| Age (y), Median (range) | 48 (28–73) |
| Disease, n (%) | |
| Myeloproliferative disorders: CML/MF/MDS | 3/1/1 (12%) |
| MM | 8 (20%) |
| Lymphoproliferative disorders: NHL/HD/CLL | 5/2/0 (18%) |
| Others: solid tumor | 1 (2%) |
| Transplant, n (%) | |
| MUD | 8 (20%) |
| HLA identical sibling | 32 (80%) |
| PBSC | 30 (75%) |
| BM | 10 (25%) |
| Conditioning regimen, including TBI | 17 (44%) |
| cGVHD | |
| Duration (mo), median (range) | 26 (3–148) |
| Risk score27 (high/intermediate/low), n | 24/15/1 |
| First-line therapy, n | |
| Prednisone (alone or with other drugs) | 36 |
| Miscellaneous (including MMF, tacrolimus, ECP, CSA) | 4 |
| Second and successive lines of therapy, n | |
| Rituximab + miscellaneous (no ECP) | 5 |
| Rituximab + ECP ± miscellaneous | 8 |
| Miscellaneous, including ECP (no rituximab) | 8 |
| Miscellaneous, excluding ECP and rituximab | 19 |
| Karnofsky performance status at enrollment, n (%) | |
| <70 | 28 (70%) |
| 80 | 9 (22%) |
| 90–100 | 3 (8%) |
| Platelet count before imatinib initiation, 109/L, n (%) | |
| <100 | 2 (5%) |
| >100 | 38 (95%) |
| Main cGVHD targets (different organ involvements are not mutually exclusive) | |
| Skin, n (%) | 32 (80%) |
| Mean affected BSA% for erythematous/moveable/nonmoveable sclerosis | 19/27/27 |
| Lung, n (%) | 33 (82.5%) |
| Median values of FEV1/DLCO | 61/55 |
| Mouth, n (%) | 23 (57.5%) |
| Median Schubert Scale value | 3 |
| Liver, n (%) | 6 (15%) |
| Median values of ALT (U/L)/total bilirubin (mg/dL) | 74/3.0 |
| Gut, n (%) | 9 (22.5%) |
| Mean value of the GI scale (0-3) | 1.5 |
ALT, alanine transaminase; BM, bone marrow; CLL, chronic lymphocytic leukemia; CML, chronic myeloid leukemia; CSA, cyclosporine; HD, Hodgkin disease; MDS, myelodysplastic syndrome; MF, myelofibrosis; MM, multiple myeloma; MMF, mycophenolate mofetil; MUD, matched unrelated donor; NHL, non-Hodgkin lymphoma; and PBSC, peripheral blood stem cells.
Intention-to-treat (ITT) analysis for response and outcome evaluation included the 39 patients receiving imatinib (regardless of the duration of treatment).
Patient characteristics
Forty consecutive adults with a median age of 48 years (range, 28-73), most with multi-organ cGVHD, were enrolled between February 7, 2008 and May 3, 2011. Patient characteristics are detailed in Table 1.
Eligibility criteria included active, moderate to severe cGVHD as per the NIH criteria24 (requiring >0.4 mg/day of prednisone), with or without sclerotic features and refractory to at least 2 immunosuppressive lines of therapy. The NIH scoring system24 was used at baseline for scoring cGVHD involvement in 5 organs (skin, mouth, gut, liver, lungs); the global NIH severity (mild, moderate, severe) score was then calculated for all evaluable patients3 and re-assessed after 6 and 12 months of treatment. Four patients had moderate cGVHD and 36 had severe cGVHD (Figure 1). Severe scoring was attributable to multiple severe organ involvement in 13 patients and single severe organ involvement in 23 (13 with severe skin involvement and 10 with moderate/severe lung involvement). Thirty-one patients had skin involvement (25 with sclerotic features) and 33 had clinical lung involvement, with compromised forced expiratory volume and/or diffusion capacity of the lung for carbon monoxide. Twenty-four patients exhibited oral mucosal involvement, 9 exhibited gut involvement, and 6 exhibited liver involvement. A patient could have involvement of one or more of the aforementioned organs.
Treatment schedule and concomitant therapy
Imatinib treatment was planned for at least 6 months, starting at 100 mg/day during the first 15 days. In the absence of severe (grade 3-4 WHO) toxicity, the dosage was gradually increased to 400 mg/day.9 Patients who achieved measurable response at 3 months continued imatinib for up to 6 months. After 6 months, imatinib was continued at the discretion of the physician.
Patients taking steroids, cyclosporine, or other concomitant immunosuppressive treatment (including ECP) were allowed to continue treatment, whereas those taking myelotoxic drugs such as cyclophosphamide, pentostatin, or methotrexate were not. Patients treated with rituximab (RTX) in the previous 6 months were excluded to avoid a possible interference with the evaluation of anti–PDGF-R antibodies. Supportive care and other medications were allowed according to institutional guidelines and local practice.
Organ-specific and global response evaluation
A center-assigned global response (Center Response), ie, a clinical judgment reported by the local investigator on the basis of the Couriel criteria,22,23 expressed on a 4-point scale (complete response [CR], partial response [PR], MR/SD, or no response/progressive disease [NR/PD]), was evaluated every 3 months after imatinib therapy. The decision to continue imatinib at 3 and 6 months was based on Center Response. Data about steroid dose modifications during imatinib treatment were also collected and integrated into the Center Response.
At baseline and at 6 months, NIH forms regarding clinician-assessed measures were completed, from which we derived 5 organ-specific core clinical measures of GVHD activity. Genital assessments, for which there were no robust objective measures; fascial/articular evaluations, which could partially overlap with sclerotic involvement; and eyes, whose damage is often irreversible, were not included.8,21 The data were collected centrally, and organ-specific and global responses were calculated together according to the NIH response criteria proposed by Pavletic and coworkers (in their Appendix D) as CR, PR, SD, and PD.21 For the skin, an overall district response was evaluated from the 3 scales resulting from the 3 different skin manifestations (erythematous rash, moveable, and hidebound sclerosis). In the case of discordance between the response in 2 manifestations (ie, PD in the erythematous and PR in moveable), the response was calculated on the overall body surface area; however, PD in the hidebound skin always indicated PD. For patients with lung involvement, improvement of at least 1 point on the lung functional score (LFS), without any evident clinical deterioration, was defined as PR. With regard to the other organs, the original NIH criteria were used according to the algorithm reported in supplemental File (available on the Blood Web site).
Patients were also classified according to modifications of the organ-specific NIH severity score (NIH SS).3-24 Briefly, the NIH SS was calculated in each district at baseline and after 6 months. Changes were recorded as CR (complete resolution), PR (improvement of at least 1 point), SD (stable), and PD (worsening of at least 1 point).
After calculating organ-specific responses with NIH criteria and NIH SS, global response was determined as follows: CR was defined as CR in all affected organs; PR as CR/PR in at least 1 organ, without evidence of PD in any organ; SD as SD in each affected organ; and PD as PD in at least 1 organ.
Antibody (Ab) purification and bioassay for anti-PDGFR Ab
Immunoglobulins (Igs) from patients with cGVHD were purified from serum as previously described.17,18 Briefly, the stimulating ability of these antibodies to induce PDGF-R phosphorylation was evaluated using an in vitro fibroblast bioassay. Murine fibroblasts transduced with human PDGF-R were incubated with the patients’ purified Igs, and the reactive oxygen species (ROS) output was measured at baseline and after treatment with imatinib.17 These tests were conducted for patients who received imatinib for at least 6 months, according to patient and center availability. Only the samples from patients free of imatinib treatment of at least 1 week were evaluated to avoid possible interference with the PDGF-R pathway.
Results
Forty patients were entered into the trial. One patient never began imatinib treatment because the informed consent was reviewed with the local investigator and retracted. This patient received an alternative treatment and eventually died. The 39 patients who received imatinib were evaluated for toxicity, response, and outcome, regardless of the duration of treatment; 34 received treatment of ≥3 months. Imatinib was continued at 200 mg/day in 18 patients, increased to 300 mg/day in 8, and increased to 400 mg/day in 8.
Imatinib was administered at a mean dose of 270 mg/day for a median duration of 16 months (range, 1–45). After 6 months, most patients (22) were receiving imatinib at 200 mg/day.
Thirteen patients discontinued imatinib within 1 year, and 14 were still receiving imatinib at the last follow-up.
Toxicity
No toxic deaths were observed. Details about the patients who had grade 1-2, 3, and 4 toxicities are reported in Table 2. During imatinib treatment, 153 grade 1-2 and 23 grade 3-4 events according to the CTC were recorded (supplemental Table 1 and supplemental Figure 2). Most events occurred during the first 3 months of treatment (90% of grade 3-4 events and 69% grade 1-2 events). Common adverse events (AEs) included fatigue, muscle pain, and weakness. Fluid retention was uncommon, and no severe heart or liver toxicity was observed. Hematologic toxicity was represented mainly by anemia and thrombocytopenia (3 grade 3-4 events).
Main extrahematologic and hematologic toxicities in the 39 patients treated with imatinib
| Toxicities . | Patients experiencing toxicities by grade . | ||
|---|---|---|---|
| 1–2 . | 3 . | 4 . | |
| Extrahematologic | |||
| Nausea | 7 (17%) | 0 | 0 |
| Diarrhea | 5 (12%) | 0 | 0 |
| Cramps | 14 (35%) | 1 (2%) | 1 (2%) |
| Muscle pain | 11 (28%) | 3 (7%) | 2 (5%) |
| Peripheral edema | 6 (15%) | 1 (2%) | 0 |
| Periorbital edema | 5 (12%) | 2 (5%) | 0 |
| Asthenia | 13 (33%) | 2 (5%) | 2 (5%) |
| Emesis | 2 (5%) | 0 | 0 |
| Abdominal pain | 5 (12%) | 0 | 0 |
| Rash | 2 (5%) | 0 | 0 |
| Kidney | 5 (12%) | 0 | 0 |
| Muscle weakness | 9 (23%) | 2 (5%) | 1 (2%) |
| Liver | 1 (2%) | 0 | 0 |
| Neuropathy | 1 (2%) | 0 | 0 |
| Weight gain | 2 (5%) | 0 | 0 |
| Heart failure | 2 (5%) | 0 | 0 |
| Bullous dermatitis | 0 | 0 | 1 (2%) |
| Hematologic | |||
| Anemia | 25 (64%) | 1 (2%) | 0 |
| Neutropenia | 6 (15%) | 0 | 0 |
| Thrombocytopenia | 4 (10%) | 1 (2%) | 0 |
| Toxicities . | Patients experiencing toxicities by grade . | ||
|---|---|---|---|
| 1–2 . | 3 . | 4 . | |
| Extrahematologic | |||
| Nausea | 7 (17%) | 0 | 0 |
| Diarrhea | 5 (12%) | 0 | 0 |
| Cramps | 14 (35%) | 1 (2%) | 1 (2%) |
| Muscle pain | 11 (28%) | 3 (7%) | 2 (5%) |
| Peripheral edema | 6 (15%) | 1 (2%) | 0 |
| Periorbital edema | 5 (12%) | 2 (5%) | 0 |
| Asthenia | 13 (33%) | 2 (5%) | 2 (5%) |
| Emesis | 2 (5%) | 0 | 0 |
| Abdominal pain | 5 (12%) | 0 | 0 |
| Rash | 2 (5%) | 0 | 0 |
| Kidney | 5 (12%) | 0 | 0 |
| Muscle weakness | 9 (23%) | 2 (5%) | 1 (2%) |
| Liver | 1 (2%) | 0 | 0 |
| Neuropathy | 1 (2%) | 0 | 0 |
| Weight gain | 2 (5%) | 0 | 0 |
| Heart failure | 2 (5%) | 0 | 0 |
| Bullous dermatitis | 0 | 0 | 1 (2%) |
| Hematologic | |||
| Anemia | 25 (64%) | 1 (2%) | 0 |
| Neutropenia | 6 (15%) | 0 | 0 |
| Thrombocytopenia | 4 (10%) | 1 (2%) | 0 |
Infectious episodes developed in 12 patients: 7 episodes of pneumonia (2 from Aspergillus and 1 from Candida albicans), 2 from cytomegalovirus reactivation, 1 from sepsis (Pseudomonas aeruginosa), 1 from varicella zoster reactivation, 1 from enteritis (Salmonella), and 1 from influenza pneumonia (H1N1 virus) associated with the Aspergillus pneumonia. The 2 patients in whom Aspergillus pneumonia developed eventually died.
Response
Of the 39 patients receiving imatinib, 7 were not evaluable for response at 6 months because of treatment failure. Three patients died (1 each at 8 days, 6 weeks, and 3 months after initiating imatinib), 2 because of rapid cGVHD progression and 1 as a result of a pulmonary infection. Two patients had severe AEs after 2 and 10 weeks of imatinib treatment and received an alternative treatment (both were alive at the last follow-up). Two patients discontinued imatinib within 3 months because of cGVHD progression and received an alternative treatment (both were alive at the last follow-up).
The response at 6 months was evaluated using Center Response, NIH response criteria and NIH SS change (Table 3; see details in supplemental Table 2 and supplemental Figure 2). One patient with a GVHD flare after 5 months was treated with transient steroid increase and saw notable improvement; because of the rapid changing situation, the local investigator judged him to be not evaluable for Center Response.
Global and organ-specific response according to center evaluation (response based on Couriel criteria), NIH response criteria, and changes in NIH severity score (NIH SS)
| Center (Couriel) . | NIH criteria . | Changes in NIH SS . | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Response . | Overall . | Response . | Skin . | Lungs . | Mouth . | Liver . | Gut . | Overall . | Response . | Skin . | Lungs . | Mouth . | Liver . | Gut . | Overall . |
| ORR corr* | 46% | ORR corr* | 51.3% | ORR corr* | 56.4% | ||||||||||
| ORR | 36% | ORR | 32% | 35% | 16% | 25% | 50% | 51.3% | ORR | 22% | 25% | 38% | 25% | 50% | 51.3% |
| CR | 0 | CR | 3 | 2 | 4 | 2 | 5 | 0 | CR | 3 | 2 | 4 | 2 | 5 | 0 |
| PR | 14 | PR | 7 | 9 | 0 | 0 | 1 | 20 | PR | 4 | 6 | 5 | 0 | 0 | 20 |
| MR/SD | 12 | SD | 15 | 13 | 18 | 4 | 4 | 7 | SD | 20 | 17 | 13 | 5 | 3 | 9 |
| NR/PD | 5 | PD | 2 | 1 | 0 | 0 | 2 | 5 | PD | 0 | 1 | 0 | 0 | 2 | 3 |
| NE | 8 | NE | 4 | 7 | 3 | 2 | 0 | 7 | NE | 4 | 6 | 2 | 1 | 0 | 7 |
| TOT. | 39 | TOT | 31 | 32 | 25 | 8 | 12 | 39 | TOT | 31 | 32 | 24 | 8 | 10 | 39 |
| EVAL | 31 | EVAL | 27 | 25 | 22 | 6 | 12 | 32 | EVAL | 27 | 26 | 22 | 7 | 10 | 32 |
| Center (Couriel) . | NIH criteria . | Changes in NIH SS . | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Response . | Overall . | Response . | Skin . | Lungs . | Mouth . | Liver . | Gut . | Overall . | Response . | Skin . | Lungs . | Mouth . | Liver . | Gut . | Overall . |
| ORR corr* | 46% | ORR corr* | 51.3% | ORR corr* | 56.4% | ||||||||||
| ORR | 36% | ORR | 32% | 35% | 16% | 25% | 50% | 51.3% | ORR | 22% | 25% | 38% | 25% | 50% | 51.3% |
| CR | 0 | CR | 3 | 2 | 4 | 2 | 5 | 0 | CR | 3 | 2 | 4 | 2 | 5 | 0 |
| PR | 14 | PR | 7 | 9 | 0 | 0 | 1 | 20 | PR | 4 | 6 | 5 | 0 | 0 | 20 |
| MR/SD | 12 | SD | 15 | 13 | 18 | 4 | 4 | 7 | SD | 20 | 17 | 13 | 5 | 3 | 9 |
| NR/PD | 5 | PD | 2 | 1 | 0 | 0 | 2 | 5 | PD | 0 | 1 | 0 | 0 | 2 | 3 |
| NE | 8 | NE | 4 | 7 | 3 | 2 | 0 | 7 | NE | 4 | 6 | 2 | 1 | 0 | 7 |
| TOT. | 39 | TOT | 31 | 32 | 25 | 8 | 12 | 39 | TOT | 31 | 32 | 24 | 8 | 10 | 39 |
| EVAL | 31 | EVAL | 27 | 25 | 22 | 6 | 12 | 32 | EVAL | 27 | 26 | 22 | 7 | 10 | 32 |
ORR, overall response rate, calculated as (CR + PR)/TOT (total number of patients receiving imatinib); ORR corr*, corrected ORR, taking into account patients with MR/SD with concomitant steroid sparing (>50% of the initial dose); CR, complete response; PR, partial response; MR, minor response; SD, stable disease; NR, no response; PD, progressive disease; NE, not evaluable (NE category includes patients who did not undergo a CR evaluation at 6 months because of treatment failure within 6 months [7] or other reasons [1 for Center Response]); TOT, total patients receiving imatinib included in the ITT analysis; EVAL, includes patients undergoing a complete response evaluation at 6 months according to NIH, Center, and changes in NIH SS response.
According to Center (Couriel) criteria, patients with SD and without significant steroid-sparing were considered NR; in the category MR/SD, we included patients with SD and >50% steroid reduction, and all patients with MR.22
According to Center Response, we observed 14 PR and 12 MR/SD; of these, four achieved significant and sustained steroid sparing (>50% of the daily dose). Therefore, the ORR (including the criterion of steroid sparing used in our first trial9 ) was 46.1% (18/39 patients). According to the NIH criteria, 20 of 39 patients were classified as PR (51.3%) and 7 of 39 as SD. The best response rates were observed in the gut and lungs, with 50% and 35% of affected patients achieving PR, respectively. A retrospective evaluation of response based on changes in NIH SS revealed 20 PR (51.3%) and 9 SD.
The response evaluation was grossly different in 2 patients (ie, changing the status from ≥SD/MR to NR/PD or vice versa) according to the 3 response criteria. One patient exhibited a strong improvement in LFS (from 8 to 3) as well as an evident worsening in the skin according to the NIH criteria; exhibiting PD in the skin resulted in overall PD. Regarding the NIH SS, this patient already had the highest category of skin score (3) at baseline; therefore, he was judged to have SD. In the Center Response, the local investigator classified him as an MR. The second patient exhibited severe lung involvement with the highest LFS (12), and pulmonary function further worsened at 6 months. This patient was judged to have SD by NIH response and NIH SS change and NR by Center Response. A few other minor discordances were observed. For example, a patient was classified as PR according to the NIH criteria because of an improvement in LFS (9 to 8), but as SD according to NIH SS changes: in fact the lung improvement was not enough to improve the NIH severity category in the lung; other affected organs were stable. This patient was judged to be MR by the local investigator according to the Couriel criteria.
At initiation of imatinib, 14 patients were receiving concomitant steroid therapy. In 13 patients evaluable at 6 months (1 patient died), the median dose of prednisone (PDN) was 0.16 mg/kg at baseline and 0.03 mg/kg after 6 months. Two patients were given PDN after imatinib discontinuation because of treatment failure, and four discontinued the PDN. According to Center Response, PDN dose was decreased in all 5 patients classified as PR at 6 months. Of the 7 patients with MR/SD, the dose was decreased in five and was unchanged in two. Of the 3 patients with NR, the PDN dose was increased in two and discontinued in one because of inefficacy. Twelve months after the initiation of imatinib, 18 of 26 patients with ≥MR/SD maintained their improvement: 9 remained unchanged or decreased their previous immunosuppressive treatments and 9 were able to permanently discontinue them.
No significant differences (P = .29) were found in the mean imatinib dose between responders (202 mg/day) and nonresponders (221 mg/day).
Outcome
The median follow-up period was 40 months (minimum 12). Twenty-eight of the 39 patients were alive at the last follow-up. We observed 2 early deaths (before completing the first month of imatinib therapy) because of lung cGVHD progression. Five patients died because of cGVHD progression after 3, 7, 9, 15, and 16 months, respectively; 3 died of infection (1 each from necrotizing enteritis, lung candidiasis, and septic shock) after 6, 26, and 51 months, respectively; and 1 died from relapsed acute myelogenous leukemia 24 months after imatinib discontinuation.
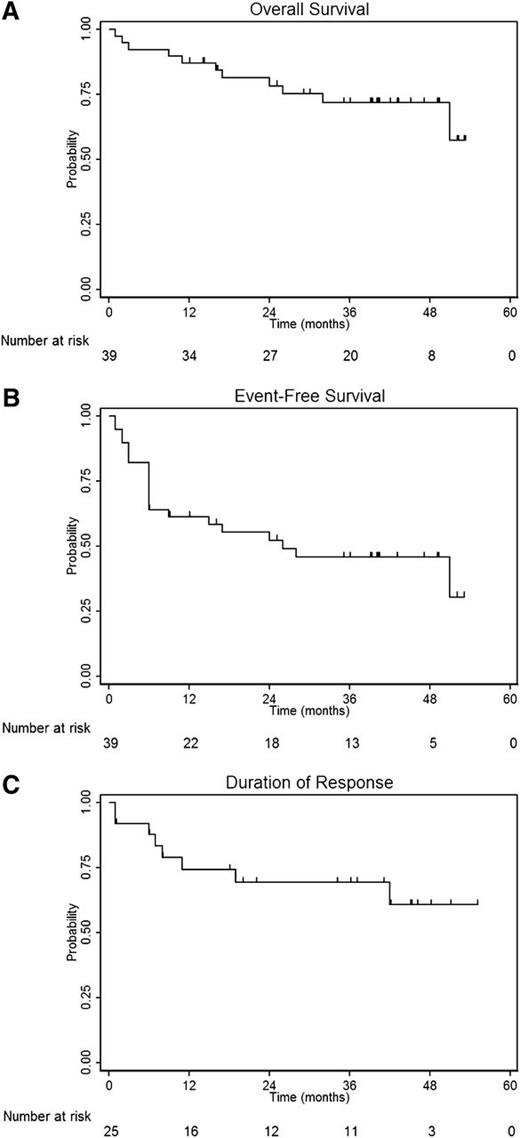
The 3-year OS and EFS were 72% (95% confidence interval [CI], 54-84) and 46% (95% CI, 29-61), respectively. In the 26 patients who achieved ≥MR/SD after 6 months, RD was 69% at 36 months (95% CI, 46-84; Figure 2). In the 14 patients with ≥ PR according to Center Response, RD was 83.1% at 36 months (data not shown). A landmark analysis for OS at 6 months according to response status revealed that achieving ≥PR at this time point (regardless of the response criteria used) strongly predicted the outcome (Figure 3A-C), suggesting that adopting a centralized NIH response criteria is a reliable tool for predicting outcome. According to univariate analyses, the baseline characteristics reported in Table 1 were not significantly associated with a difference in OS.
Survival outcomes. Overall survival (A) and event-free survival (B) in the 39 patients receiving imatinib, and response duration (C) in the 26 patients who achieved ≥ MR/SD (minor response or stable disease with steroid sparing) at 6 months according to Center Response. OS was measured from the initiation of imatinib until death, and EFS was measured from the initiation of imatinib until death, secondary neoplasia, or treatment failure. Response duration (RD) was defined as time from response evaluation at 6 months to loss of response (NR/PD) in patients achieving ≥ MR/SD at this time point, according to Center Response. Among patients with SD, only those with stable pulmonary function and a >50% decrease in steroid dose were included.22
Survival outcomes. Overall survival (A) and event-free survival (B) in the 39 patients receiving imatinib, and response duration (C) in the 26 patients who achieved ≥ MR/SD (minor response or stable disease with steroid sparing) at 6 months according to Center Response. OS was measured from the initiation of imatinib until death, and EFS was measured from the initiation of imatinib until death, secondary neoplasia, or treatment failure. Response duration (RD) was defined as time from response evaluation at 6 months to loss of response (NR/PD) in patients achieving ≥ MR/SD at this time point, according to Center Response. Among patients with SD, only those with stable pulmonary function and a >50% decrease in steroid dose were included.22
Thirty-six of the 39 patients receiving imatinib were alive at 6 months and were included in a landmark analysis for overall survival (OS) according to response status at 6 months. In this analysis responders were those patients included in the ORR reported in Table 3, not corrected for steroid sparing. The 36-month OS was significantly higher for responders (dotted line) than for nonresponders (solid line): 94% vs 55%, 100% vs 60%, and 94% vs 58% according to changes in NIH SS (A), Center Response (B), and NIH criteria (C), respectively.
Thirty-six of the 39 patients receiving imatinib were alive at 6 months and were included in a landmark analysis for overall survival (OS) according to response status at 6 months. In this analysis responders were those patients included in the ORR reported in Table 3, not corrected for steroid sparing. The 36-month OS was significantly higher for responders (dotted line) than for nonresponders (solid line): 94% vs 55%, 100% vs 60%, and 94% vs 58% according to changes in NIH SS (A), Center Response (B), and NIH criteria (C), respectively.
Anti–PDGF-R antibodies and response
All 11 patients who were evaluated with the functional bioassay17,18 had relevant anti–PDGF-R antibody activity before treatment; of these, seven responded to imatinib, whereas four did not. The relative decrease in PDGFR agonistic activity in terms of ROS stimulation (ROS index) was evaluated at different time points, and a significant difference was observed between the 2 groups (P = .006). The ROS index was decreased in all responders, whereas in the nonresponders, the anti–PDGF-R activity did not substantially change compared with that at baseline, suggesting a relationship between clinical response and the resolution of agonistic antibody–mediated PDGF-R stimulation (Figure 4). There was no significant difference in the mean imatinib dose between responders and nonresponders (P = .38), and no correlation was observed between the imatinib dose and a change in ROS index (r = −0.12).
Mean change in the ROS stimulatory index (ROI) of cGVHD Igs before and after imatinib treatment according to response status (Center Response).
Mean change in the ROS stimulatory index (ROI) of cGVHD Igs before and after imatinib treatment according to response status (Center Response).
Discussion
The management of SR-cGVHD is problematic, and the evidence is limited to phase 2 trials or retrospective studies.7-9,28,29
Survival at 5 years among patients with high-risk cGVHD is reported to be approximately 50%.1,5,31 with a median survival of only 30 months.2 In a recent study, the NIH SS was an independent factor for predicting cGVHD-specific survival.31 A recent retrospective study in 312 patients receiving second-line treatment of cGVHD showed a 56% failure-free survival (FFS) at 6 months, and NIH SS emerged again as an independent factor influencing outcome. Moreover, this study suggested that the 6-month FFS may represent an early surrogate end point for predicting the long-term efficacy of a second-line treatment of SR-cGVHD in clinical trials.27
Our study demonstrates that response at 6 months strongly correlates with OS, regardless of the criteria adopted, suggesting that this early end point is highly predictive of the long-term outcome. There was a low discordance rate using the 3 different response criteria; however, the feasibility of the NIH response criteria has been extensively evaluated in both retrospective32 and prospective33 studies. Our study is the first to assess the feasibility of NIH response criteria in the context of a therapeutic trial and validate their prognostic impact on survival. Although further confirmation in larger randomized trials and in different populations of cGVHD patients is required, NIH criteria should be considered the new standard for measuring therapeutic response in future prospective trials of cGVHD. The use of an automatic algorithm defining the kind of response according to NIH recommendations (supplemental File) may facilitate its application in clinical practice.
As per the Couriel criteria, the response rate in this trial was lower than that in our first trial,9 but it should be noted that the median age of the population treated in this trial was significantly higher than that in the first cohort (48 vs 27 years), which also included pediatric patients. The incidence of severe toxicity was acceptable; 2 patients died of lung aspergillosis, a common complication of SR-cGVHD regardless of the immunosuppressive treatment used.
In our first trial, only patients with skin fibrotic features were treated, whereas this study also included patients with visceral involvement, suggesting that imatinib is effective against all types of cGVHD. In a retrospective French study, 39 patients with SR-cGVHD who were taking imatinib were evaluated by the physician according to his perception of the change in skin involvement: as “improvement,” “stability,” or “worsening.” According to this empirical approach, the authors found an overall improvement rate of 30%. Systemic corticosteroids were tapered or discontinued in 41% of patients.13 Other experiences with imatinib for SR-cGVHD have yielded fewer encouraging results. Chen et al12 evaluated 15 patients according to Hopkins criteria and reported an ORR of 40% at the last follow-up. Stadler11 reported only 2 PR among 9 patients with severe SR-cGVHD of the lungs. Several factors such as differences in baseline characteristics of patients, duration of imatinib treatment, higher variability because of a smaller sample size, and evaluation of only some organs with different response criteria can partly explain the lower ORR found in these studies.
Despite the low number of patients, our data suggest a relationship between response to imatinib and anti–PDGF-R antibody activity. In contrast to the findings of Chen et al,12 we observed that although patients had a relevant anti–PDGF-R activity at baseline, the stimulating activity of these antibodies significantly decreased in the responding patients. Chen et al used a different assay for detecting the anti–PDGF-R antibodies; therefore, we cannot exclude that these authors assessed antibodies directed against different PDGF-R epitopes. Moreover, the behavior of the anti–PDGF-R antibodies during treatment suggests that imatinib may also act through an immune-modulating effect, leading to a decrease in the level of these antibodies in the responders.
In conclusion, imatinib represents a valuable option for patients with SR-cGVHD who cannot access other treatments such as ECP; this treatment is simple because it requires neither hospitalization nor long-term central venous access. In our study, imatinib use was feasible in 85% of the patients, achieving a clinically meaningful response in approximately half of the patients. Our data support further investigation of this agent in SR-cGVHD; the true efficacy of imatinib has to be confirmed and tested in larger randomized controlled trials.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This study was supported by AIFA (Agenzia Italiana del Farmaco–Italian Drug Agency).
Authorship
Contribution: A.O., A.B., and M.C. conceived and designed the study; A.O., M.C., P.C., N.M., R.F., C.S., F.O., F.P., E.P., P.L., A.B., and P.B. provided study materials or patients; S.S., A.P., and A.G. performed, analyzed, and interpreted the biological data; M.C., J.O., S.P., R.N., and A.O. collected, analyzed, and interpreted the clinical data; and A.O. and A.B. wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Prof. Attilio Olivieri, Clinica di Ematologia, Azienda Ospedaliero-Universitaria “Ospedali Riuniti,” via Conca 71, 60126 Ancona, Italy; e-mail: a.olivieri@univpm.it.




This feature is available to Subscribers Only
Sign In or Create an Account Close Modal