Abstract
Acute myeloid leukemia (AML) is a clinically and biologically complex and heterogeneous hematopoietic neoplasm. Recent advances in acute myeloid leukemia (AML) biology have lead to prognosticate and predict treatment outcome in AML based on molecular markers. Mutations in NPM1, CEBPA are considered good prognosis and High BAALC, ERG & MN1 expression associate with worse outcome in AML patients treated with standard chemotherapy. Although many efforts have been made to identify genetic mutations and modulated gene expression levels that can be used to predict outcomes in patients with AML, the association between these prognostic markers has not been evaluated. We have reported previously that the NPM1 mutated patients have significantly high dCK and hENT1 gene expression (involved in cytarabine metabolism) and low ABCG2 and ABCB1transporter expression (Abraham et al, ASH abstracts; Nov 2011; 118: 3481 and Nov 2012; 120: 143), suggesting that the good prognostic nature of this mutation is possibly due to the better metabolism and transport of the chemotherapeutic drugs used in induction therapy. We extended this study to look for association between NPM1/FLT3 mutation status and the RNA expression of other good or poor prognostic markers in patients with AML.
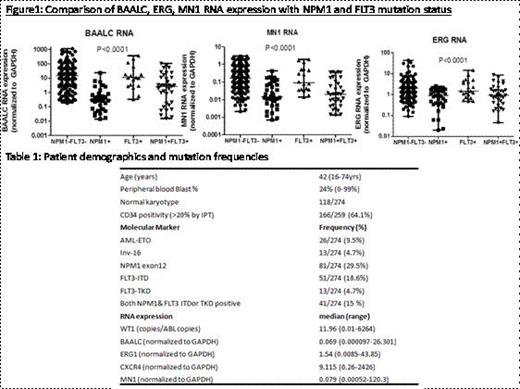
We prospectively included 274 adult patients with AML in this study. The median age was 42 years (range 16-74y). AML was diagnosed according to the FAB and WHO classifications. There were 238 patients with de novo AML; Secondary AML -6; Therapy related AML- 2 and Relapsed AML-28. Bone marrow cytogenetics and immunophenotyping analysis was available for all patients at diagnosis and/or relapse. Diagnostic bone marrow MNCs were isolated by ficoll- density gradient centrifugation and stored in trizol reagent for RNA expression and mutation detection. RT-PCR was used to screen AML-ETO and Inv 16, and the expression of BAALC, ERG1, MN1, CXCR4 and WT1were analyzed using RQ-PCR. NPM1-c, FLT3 ITD and TKD were screened using DNA PCR followed by gene-scan, sequencing or RFLP methods. The basic demographics and the frequency of the markers are listed in Table 1. When analyzed separately in normal karyotype AML (NK-AML), the frequencies of the mutations were: NPM1: 52.2%; FLT3-ITD: 24%; TKD: 4.3%.
When the RNA expression of BAALC, WT1, ERG1, CXCR4 and MN1 was compared in patients with NPM1 or FLT3 mutations, we noticed that patients with NPM1 had significantly low expression of BAALC, MN1 and ERG1 while those with FLT3 mutations (ITD or TKD) had higher expression of these genes (Figure1). There was no significant association with CXCR4 or WT1 expression and these mutations. When analyzed separately in the normal karyotype AML, these associations were still significant. In addition, the relapsed patients had significantly higher expression of BAALC, MN1, and ERG1 RNA compared to de-novoAML cases (data not shown).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal