Abstract
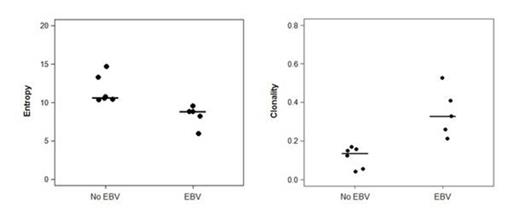
Umbilical cord blood (UCB) is an alternative source of hematopoietic stem cells (HSC) for allogeneic HSC transplantation but reconstitution of T cell immunity remains problematic even with double UCB transplantation (dUCBT). This is related to the small T cell numbers of the UCB graft, the naïve nature of these T cells and often the use of ATG as part of the conditioning regimen. Consequently, UCBT recipients are susceptible to viral infections that require intact T cell immunity for their containment. Epstein Barr virus (EBV) is a gammaherpes virus that is transmitted orally. EBV initially replicates in a lytic cycle in the epithelium of the oropharynx and then establishes a latent state in memory B cells. Reactivation of EBV from latent to lytic cycle is mediated by physiologic stress of the memory B cell pool and by defects in antiviral T cell immunity, and can cause aggressive lymphomas known as post transplant lymphoproliferative disorder (PTLD) in immunocompromised hosts. The specific immunological correlates of EBV reactivation in adult UCBT recipients have not been examined. In the present study we attempted to distinguish immune reconstitution profiles in UCBT recipients who developed EBV viremia from those who did not, in order to better understand the immune profile of UCBT recipients who control gammaherpes virus reactivation. Thirty-one patients with hematologic malignancies received dUCBT with melphalan, fludarabine, ATG conditioning and tacrolimus plus sirolimus for GvHD prophylaxis. EBV viral load was determined on a weekly basis after dUCBT. Immunophenotype of peripheral blood lymphocytes, serum cytokine levels and T cell receptor excision circle analysis (TREC) values, were examined prior to and at 1, 2, 3, 6 and 12 months after UCBT and were compared between EBV viremic and non-viremic patients using the Wilcoxon-rank sum test. During the first 12 months after dUCBT, 14 of 31 (45%) patients developed EBV viremia and four (13%) developed PTLD. At one month after dUCBT, patients who developed EBV viremia displayed higher numbers of CD19+ B cell numbers (p=0.04) and CD4+CD25+ T regulatory cells (p=0.03) compared with patients who never became viremic. Surprisingly, development of EBV viremia correlated with increased numbers of CD3+ (p=0.04), CD4+ (p=0.015) and CD8+ (p=0.021) T cells. This finding was counterintuitive, as one might expect better quantitative peripheral T cell reconstitution in patients with recovering immunity and no EBV reactivation. One mechanism of impaired immune reconstitution after UCBT is skewing towards a late effector memory T cell phenotype, a stage in which T cells are incapable of mounting protective immune responses. We examined whether development of EBV viremia was associated with altered naïve versus memory T cell distribution. We determined that patients who developed EBV reactivation had higher numbers of memory cell subsets (CD4+CD45RO+, p=0.0023; CD8+CD45RO+, p=0.019) at two months after dUCBT. Neither development nor control of EBV viremia correlated with TREC recovery, which occurred after the time period of EBV viremia. We were unable to identify EBV-specific T cells in any patient group due to the very low T cell numbers during the time of viremia. However, analysis of repertoire diversity by deep-sequencing on PCR-amplified CDR3 regions of the TCRb gene using the ImmunoSEQ assay showed a more diverse TCR repertoire, as determined by higher entropy (p=0.03) and lower clonality (p=0.03), among patients who did not develop EBV reactivation, compared with those who developed EBV viremia and PTLD. Assessment of serum levels of SCF (a c-kit ligand), IL-7, thrombomodulin, VEGF and angiopoetin-1 showed that patients without EBV viremia had significantly higher levels of SCF (p=0.0001) and IL-7 (p=0.05), at 1 and 2 months after dUCBT, compared with patients who developed EBV reactivation and PTLD. SCF-mediated signaling via c-kit is integral to the homing and longevity of uncommitted hematopoietic stem cells whereas IL-7 is a critical factor for survival and homeostasis of naïve T cells. Together our findings suggest that control of EBV reactivation after dUCBT might be linked to the support of naïve T cell homeostasis, which enables maintenance of a diverse TCR repertoire.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal