Abstract
Recent studies have suggested that increased circulating free light chains, inflammatory cytokines, hepcidin, ferritin, and ASXL1 mutated status have independent prognostic value for survival in primary myelofibrosis (PMF). In the current retrospective study, we studied all the aforementioned variables in the context of DIPSS-plus to examine their relative prognostic contributions for overall and leukemia-free survival.
The diagnosis of PMF was according to WHO criteria. The study population included all consecutive referrals to the Mayo Clinic, Rochester, MN where complete information on clinical and laboratory parameters and bone marrow karyotype was available. Inclusion to the study required availability of a research blood sample collected at referral. Levels of circulating free light chains (FLC) (J Clin Oncol. 2012 Apr 1;30(10):1087), inflammatory cytokines (J Clin Oncol. 2011 Apr 1;29(10):1356), hepcidin and ferritin (Am J Hematol. 2013 Apr;88(4):312) were determined as previously described. Disease-relevant mutations (ASXL1, SRSF2, EZH2, IDH-1/2, SF3B1, JAK2V617F and MPLW515) were identified as previously described (Leukemia. 2013 Apr 26. doi: 10.1038/leu.2013.119).
A total of 224 PMF patients were studied (66% male; median age 63 years, range 18-83 years). The DIPSS-plus distribution was: Low 23 (10%), Int-1 26 (12%), Int-2 98 (44%), and High 77 (34%). Clinical characteristics were: unfavorable karyotype 13%, hemoglobin <10 g/dL 58%, leukocyte count >25 x 109/L 13%, platelet count <100 x 109/L 20%, peripheral blasts ≥1% 62%, red blood cell transfusion-dependent 38%, and constitutional symptoms 36%. Mutation frequencies were: JAK2V617F 61% (n=220), MPLW515 6% (n=204), ASXL1 34% (n=154), SRSF2 16% (n=189), IDH-1/2 3% (n=209), EZH2 1.5% (n=134), SF3B1 5% (n=91) and SETBP1 4% (n=114). Distribution of circulating biomarkers was: FLC >receiver operating characteristic (ROC) cutoff of 3.78 mg/dL 37% (n=222), interleukin (IL)-2R and/or IL-8 >3 standard deviations above normal mean (SD) 75% (n=197), ferritin ≥1000 mcg/L 18% (n=146), ferritin ≥500 30% (n=146), and hepcidin >3SD 72% (n=203).
Median follow up from the time of referral was 45 months (range 1-317 months); during this period, 139 deaths (62%) and 27 (12%) leukemic transformations have been documented.
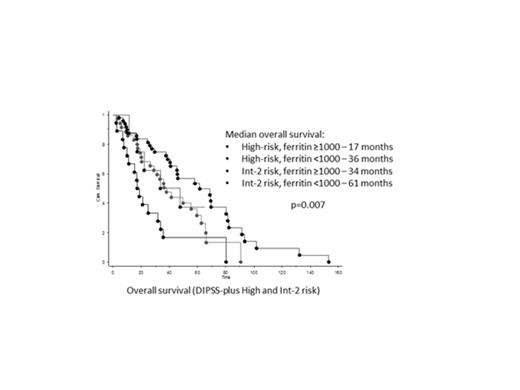
The median overall survival of the entire cohort was 61 months. The following variables had DIPSS-plus independent predictive value for inferior survival: ferritin ≥1000 mcg/L (HR 1.9), ASXL1 mutated status (HR 1.7) and FLC >ROC cutoff (HR 2.0) and IL-2R and/or IL-8 >3SD (HR 1.6) (all p<0.05). When the aforementioned variables were added to the multivariate model (sequentially or altogether), only serum ferritin >1000 mcg/L retained its significance for overall survival independent of DIPSS-plus (HR 2.1; p=0.03). The predictive significance for increased ferritin level was maintained in RBC transfusion-dependent (ferritin ≥1000 mcg/L; n=26/54; median survival 21 versus 59 months; p=0.03) and -independent (ferritin >500 mcg/L; n=5/92; median survival 20 versus 80 months; p=0.0002) patients.
Multivariable analysis identified the following predictors for inferior leukemia-free survival: SRSF2 mutated status (HR 4.8), unfavorable karyotype (HR 4.0), and circulating blasts ≥1% (HR 3.0) (p<0.05).
When considering composite risk-assessment in PMF where input variables were disease-relevant mutations and circulating biomarkers in addition to traditional clinical parameters, only increased serum ferritin levels at time-of-referral retained adverse predictive value for overall survival independent of DIPSS-plus. The prognostic value of serum ferritin was independent of anemia and RBC transfusion need. It appears to more fully capture the severity of the underlying erythropoietic defect in PMF by also likely reflecting (as an acute-phase reactant) the marrow-suppressive effect of disease-related inflammation. The shortened survival in patients with increased ferritin levels was unrelated to iron overload since none of the deaths, where information was available, were caused by cardiac siderosis. Serum ferritin levels were not associated with leukemic transformation risk. In the latter analysis, only SRSF2 mutations, unfavorable karyotype and presence of circulating blasts were independently associated with inferior leukemia-free survival.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal