Abstract

The discovery of the NPM mutation in acute myeloid leukemia (AML) allowed to identify a distinct entity with intermediate-good prognosis particularly when the FLT3/ITD mutation is absent. The most appropriate consolidation treatment of these patients upon the achievement of the first complete remission has not been established yet and the role of allogeneic stem cell transplantation (SCT) is still debated.
to assess long-term outcome of adult patients with NPM positive acute myeloid leukemia according to type and intensity of consolidation therapy.
Between May 2000 and February 2012, 1155 patients were enrolled into two consecutive, prospective Northern Italy Leukemia Group (NILG) trials (00/01 and 02/06). Six-hundred sixty nine were studied for NPM mutation and 218 (33%) proved positive (by immunohistochemistry or by molecular analysis) (Falini et al, Haematologica. 2007 Apr;92(4):519-32). Median age of NPM+ patients was 50 years (range 16-72) and 134 (61%) were female. Median WBC was 33.3 x 10^9/L (range 0.9-313.9), 71 (33%) had myelomonocytic leukemia (FAB M4), and 211 (96%) had de novo AML. According to the European Leukemia Net (ELN) classification, cytogenetic risk groups were: normal 178 (82%), intermediate 26 (12%), unfavorable 2 (1%) and unknown 12 (5%). Eighty-two (38%) patients had a concurrent FLT3/ITD mutation and 31 (14%) a FLT3/TKD mutation. According to cytogenetics and additional risk factors (late response, WBC count >50x10^9/L, FAB class M0/6/7, hepato/splenomegaly, MDS-related/secondary AML, FLT3/ITD mutation), patients were stratified in standard (SR) and high (HR) risk groups.
In both studies the remission induction was based on combination of cytarabine with idarubicin. Post-remission therapy was allogeneic SCT in HR while high-dose cytarabine or busulfan/cyclophosphamide with autologous SCT was given to SR patients. The molecular evaluation of minimal residual disease (MRD) was planned after induction, before the post-remission consolidation and the follow-up.
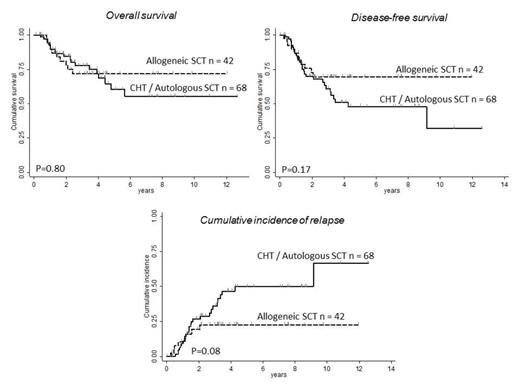
Complete remission (CR) was achieved in 196/218 (90%) NPM+ patients. One hundred sixty-eight out of 196 remitters (86%) received post-remission consolidation therapy: allogeneic SCT 72 (37%), high dose Ara-C 74 (38%), autologous SCT 14 (7%), other therapy 8 (4%); 28 patients did not receive consolidation due to early relapse (n=24), CR death (n=3), and loss to follow-up (n=1). With a median follow-up of 1.8 years (range 0.008-12.66), 99 CR patients (50.5%) were alive in 1st CR, 13 (6.5%) died of complications, and 84 (43%) had recurrent AML. In a cumulative analysis, 5-year overall and disease-free survival were 46% (OS) and 43% (DFS), respectively. In univariate analysis FLT3/ITD mutation (n=82) affected negatively 5-year OS (29% vs. 49%, P < .0001) and DFS (27% vs. 46%, P < .0001), whereas FLT3/TDK mutation did not. In patients with FLT3/ITD mutation able to receive consolidation therapy (n=49), the application of allogeneic SCT improved DFS significantly (55% vs. 18%, P = .03) and reduced the cumulative incidence of relapse (CIR) (39% vs. 81%, P = .026). In patients with NPM+ and FLT3/ITD- AML, the risk of relapse after high dose cytarabine or autologous SCT (n=68) was more than doubled compared to that observed after allogeneic SCT (n=42) (50% vs. 23%, P= .08) (Figure). However, DFS (48% vs. 69.5%, p= .17), and OS (60% vs. 72%, p= .80) were not significantly different since allogeneic SCT was associated with higher treatment related mortality, albeit effective in the salvage of some relapsed patients. In multivariate analysis, FLT3/ITD mutation was the most powerful factor that unfavorably affected OS, DFS and CIR, while age > 55 years negatively affected OS and DFS. No other clinical factor was predictive for relapse in FLT3- patients. The relationship between MRD and clinical outcome is currently being studied and will be presented.
Our data indicate that allogeneic SCT is the most active post-remission treatment for NPM+ AML, but its benefit over chemotherapy may be limited in patients without FLT3/ITD. For this reason the evaluation of MRD could help identify the patients for whom an allogeneic SCT should be preferable.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal