Abstract
Presence of primary central nervous system (pCNS) involvement at the time of diagnosis of acute lymphoblastic leukemia (ALL) in adults is a poor prognostic feature. Few reports have systematically analyzed the outcomes of adult patients (pts) diagnosed with CNS involvement at diagnosis of ALL. This report provides analysis of single institution experience outcomes in adult pts diagnosed and treated for ALL with pCNS involvement with the hyperfractionated cyclophosphamide, vincristine, doxorubicin and dexamethasone (HCVAD) or augmented Berlin-Frankfurt-Munster (AUG-BFM) based induction regimens, with or without the frontline use of Rituximab and tyrosine kinase inhibitors (TKIs).
The records of 623 consecutive pts with newly diagnosed ALL treated at the M. D. Anderson Cancer Center between January 2001 and June 2013 were reviewed. Those who had CNS involvement at diagnosis were treated with intrathecal (IT) chemotherapy twice weekly until at least 2 consecutive cerebrospinal fluid (CSF) cell counts normalized and cytologic examination was negative for evidence of malignant cells. IT therapy was subsequently administered weekly for at least 6-8 weeks, then according to the prophylactic schedule (2 intrathecals per course) for the remaining courses of intensive chemotherapy.
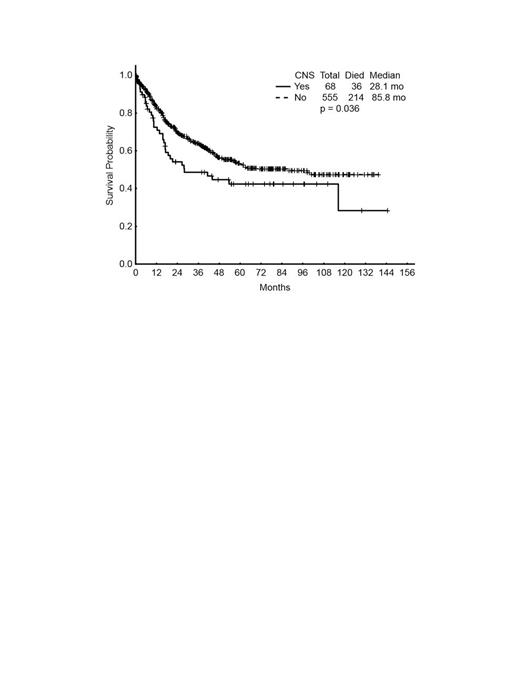
A total of 68 (11%) pts had pCNS involvement by analysis of CSF; 5 (7%) had additional brain, leptomeningeal, base of skull or spine evidence of involvement. They were treated with either HCVAD (n=52) or AUG-BFM (n=16). HCVAD with Rituximab was used in 22 (32%), and HCVAD with Dasatinib or Ponatinib in 17 (25%). Median age at diagnosis was 38 (range 13-80); 45 (66%) were male; median white blood cell count 9.9 (vs. 6.7 for those with no pCNS involvement; p=0.007); peripheral blood blast 46% (vs. 18; p=0.0008); lactate dehydrogenase 1266 (vs. 1013; p=0.03); albumin 3.3 (vs. 3.55; p=0.03); platelets 54; hemoglobin 9.3; bone marrow blast 83%. Philadelphia chromosome (Ph+) was seen in 18 (26%) vs. 140 (25%) of pts with no pCNS involvement. Among pts with pCNS, 46% expressed CD20 vs. 47% of pts with no pCNS involvement. Complete response (CR) was achieved in 61 (90%) pts compared to 513 (92%) among those with no pCNS involvement (p=0.465). Of those with CNS disease who achieved CR, 21 (34%) had a relapse, compared to 138 (27%) among those with no CNS involvement. Median complete remission duration has not been reached; Kaplan-Meier estimates for remission duration at 18 months are 66% vs. 81% for pts with with or without pCNS, respectively (p=0.147). Overall, 6 (10%) of pts with pCNS disease who had a recurrence had an isolated CNS relapse; 3 (50%) of them had a baseline Ph+. They were treated with combination therapy including HCVAD and IT cytarabine and/or methotrexate with or without craniospinal radiation and allogeneic stem cell transplantation. Five (24%) reached the second CR. The median overall survival (OS) was 28 mo for pts with pCNS involvement vs. 86 mo for those without CNS involvement at presentation (p=0.036). Of those who were evaluable in the CNS cohort, 48 (74%) pts were alive at 1 year, and 24 (41%) were alive at 4 years.
The incidence of pCNS involvement in adults with ALL has remained virtually the same over the last 20 years; 10% for HCVAD treated cohort (Cortes et al. Blood. 1995). Despite effective and wider therapeutic arsenal for ALL including Rituximab and advanced generation TKIs since year 2000, adults with ALL who present with pCNS involvement have an inferior outcome, with shorter median OS compared to pts who do not present with pCNS disease. However, pCNS is still compatible with cure if properly treated.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal