Abstract

New, refined prognostic scoring systems have been established for MDS. Most scores assess prognosis at time of diagnosis assuming stable prediction over time. Earlier studies have shown moderate loss of prognostic power over time in scores using clinical parameters whereas cytogenetic scores maintained prognostic power, scores including comorbidity had shown gain of prognostic power (Pfeilstöcker et al, 2012).
The aim of this multicenter retrospective study was to assess the relative stability of the newly developed scoring systems over time, to compare and explain observed time-related losses of prognostic power, and to discuss their clinical implications.
This study is based on 7212 untreated (no disease modifying treatment) MDS patients from multiple institutional databases of the IWG-PM, which generated the IPSS-R (Greenberg et al, 2012). Patient characteristics were well comparable with other populations: median age 71 years, male gender 60 %, median overall survival 3.8 years (range 3.7-4.0), median time to AML transformation not reached with 25% of patients transforming to AML after 6.8 years. Patients were diagnosed and classified by FAB and WHO; cytogenetics were classified by original IPSS subtypes and by the recently refined proposal integrated into the IPSS-R (Schanz et al, 2012). The following scores were analysed for their stability over time: IPSS, IPSS-R, WPSS variants, cytogenetic scores, age, performance status and other differentiating features of the IPSS-R. Time variations were described by the Cox-zph-test, and by applying Dxy, a measure of concordance, for censored data at separate observation periods.
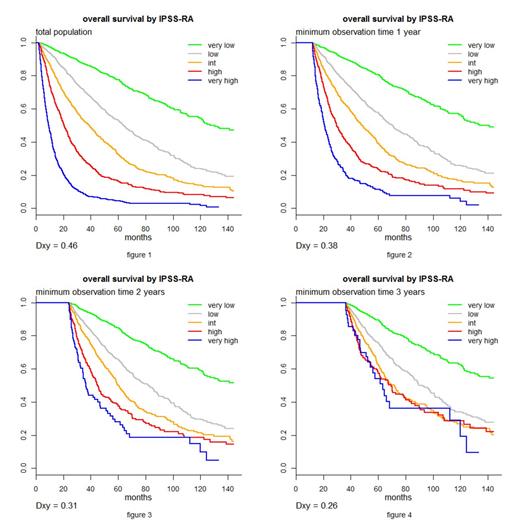
In line with previous observations, loss of prognostic power occurred over time after diagnosis in all scoring systems. While for the entire population the risk between adjacent IPSS-R risk categories differs by ∼80%, for patients observed at least 1 year the increase is ∼66%, and for those observed 4 years it is only ∼25%. The IPSS-R and particularly its age-including version (the IPSS-RA) retained the highest prognostic values compared to all other scoring systems at all time points. Dxy for IPSS-R: at diagnosis 0.43, 1 year 0.35, 2 years 0.27, 4 years 0.14. Including age, as in the IPSS-RA, was associated with less loss of prognostic power over time: Dxy at diagnosis 0.46, 1 year 0.38, 2 years 0.31, 4 years 0.22. For the IPSS and WPSS (available for the latter in only 33% cases), these values were: 0.37, 0.30, 0.22, 0.11 and 0.44, 0.36, 0.29, 0.18 respectively.
Considering risk categories, the risk remained fairly constant over time for the lower risk categories in every analyzed scoring system, while the risks in the higher risk categories were especially high in the second half of the first year after diagnosis, diminishing thereafter, thus reducing the prognostic value of these categories over time. To determine whether statistical weights optimized for each time period would alter these results, time-specific weights were applied, which did not demonstrate substantially different prognostic values from the basic model analysis. Particularly good retention of prognostic power was found in the lower risk categories over time. The lesser retention of prognostic power in the higher risk categories appeared related to loss of a larger portion of these patients over time due to their deaths or being censored by their beginning treatment. For the IPSS-R intermediate risk category patients, the prognosis for survival approached the “high” category ∼3 years after diagnosis, while it remained intermediate regarding their risk of AML transformation.
These data demonstrate that a degree of attrition of prognostic value occurred over time from diagnosis for all of the assessed MDS prognostic scoring systems. The IPSS-R, particularly the age-inclusive IPSS-RA, best retained such prognostic capability over time for the untreated patients analyzed.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal