Abstract
There is limited information on the best management of hyperleucocytosis at presentation in patients with acute promyelocytic leukemia (APL) and few studies have evaluated the clinical features and treatment options in this subset of patients (pts).
We reviewed the medical records of 233 pts with a diagnosis of APL at University of Texas - MD Anderson Cancer Center between January 1990 and December 2011. Twenty-nine (12%) had a white cell count (WBC) ≥ 50 x 109/L at presentation. Kaplan-Meier methods and log-rank tests were used to assess survival.
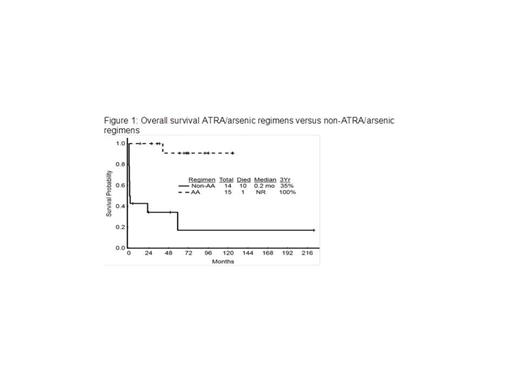
Among the 29 pts, 13 (45%) were male and median age at presentation was 48 years (29 - 77). Thirteen pts (45%) had the microgranular variant of APL. Karyotype analysis was available in 23 pts (79.3%). All 23 pts harbored the t(15:17)(q22; q21). Additional cytogenetic abnormalities involved chromosome 9 in 3 (10%), chromosome 21 in 2 (7%) and others in 6 (18%) each. Median PML-RARA transcript value was 24.0 (0.13 - 42.7). FLT3 analysis was performed in 11 pts presenting after 2003 with 100% having FLT3-internal tandem duplication and one having both FLT3-ITD and FLT3-tyrosine kinase domain mutations. No RAS or c-KIT mutations identified. Median WBC count, peripheral promyelocyte percentage, hemoglobin and platelet count at presentation were 85.5 x 109/L (53.8 - 194.8), 86.5% (0 - 97), 9.60 g/dL (7.7 - 12.8), and 25 x 109/L (10 - 124), respectively. Median bone marrow (BM) cellularity, BM promyelocyte, and BM blasts at presentation were 95% (75 - 100), 82% (0 - 90), and 5% (0 - 97), respectively. 23 (79%) pts had clinical evidence of leucostasis at presentation including hypoxia in 10 (34%), hemoptysis or diffuse alveolar hemorrhage in 6 (21%), stroke or intracranial bleeding in 4 (14%), intraocular bleeding in 4 (14%), and gastrointestinal bleeding in 4 (14%). Chemical DIC seen in 27 pts (93%) with median fibrinogen of 243 mg/dL (125 - 662), median PT of 16.6 seconds (12.6 - 24.2), median PTT of 25 seconds (21.0 - 33.8) and median INR of 2.21 (1.56 - 2.95). Treatment regimens included all-trans retinoic acid (ATRA)/arsenic trioxide (ATO) combinations in 15 (52%) patients including ATRA+ ATO in 4 (14%) and ATRA+ATO+GO (gemtuzumab ozogamicin) in 11 (38%). Non-ATRA/ATO regimens were used in 14 (48%) patients including ATRA+idarubicin (IDA) in 8 (27%), ATRA+GO in 4 (14%), and ATRA+IDA+GO in 2 (7%), respectively. Leukapheresis was performed in 11 pts (38%) with a median of 3 leukapheresis procedures (1 - 6). Median WBC at initiation and completion of leukapheresis were 106.0 (80.2 - 194.8) and 26.1 (1.7 - 35.9), respectively. 6 pts died within 4-weeks of initiating therapy. All remaining 23 pts achieved morphological complete remission (CR) after induction with median time to CR of 21.5 days (15 - 35). 6 pts relapsed and 5 achieved a second CR with salvage regimens including allogeneic transplant in 2 pts. Median OS for the entire group is 67 months. CR rate and 3-year overall survival (OS) for the pts who underwent leukapheresis were 82% and 73% versus 78% and 67% for those who did not receive leukapheresis (P=0.79 and P=0.64; respectively). CR rate and 3-year OS for the pts treated with ATRA/ATO combinations were 100% and 100% versus 57% and 35% for those treated with non-ATRA/ATO combinations (P=0.004 and P=0.002, respectively).
ATRA/ATO based combinations are superior to other therapeutic regimens in patients with APL who have hyperleukocytosis and WBC ≥ 50 x 109/L at presentation with an improved CR rate and improved 3-year OS.
3-year OS by patient characteristics
| Characteristics . | N . | 3-year survival % . | P-value . |
|---|---|---|---|
| Age | |||
| </=65 | 24 | 79 | 0.12 |
| >65 | 5 | 20 | |
| Gender | |||
| Male | 13 | 69 | 0.94 |
| Female | 16 | 68 | |
| Cytogenetics | |||
| t(15;17) alone | 17 | 88 | 0.12 |
| t(15;17) + Other | 6 | 50 | |
| Clinical Stasis | |||
| Yes | 23 | 70 | 0.58 |
| No | 6 | 67 | |
| WBC | |||
| </=100 | 17 | 77 | 0.64 |
| >100 | 12 | 57 | |
| Platelets | |||
| </=20 | 11 | 62 | 0.9 |
| >20 | 18 | 72 | |
| Fibrinogen | |||
| </=200 | 11 | 64 | 0.43 |
| >200 | 16 | 75 | |
| Leukapheresis | |||
| Yes | 11 | 73 | 0.64 |
| No | 18 | 67 | |
| Regimen | |||
| ATRA/ATO | 15 | 100 | 0.002 |
| Non-ATRA/ATO | 14 | 35 | |
| Characteristics . | N . | 3-year survival % . | P-value . |
|---|---|---|---|
| Age | |||
| </=65 | 24 | 79 | 0.12 |
| >65 | 5 | 20 | |
| Gender | |||
| Male | 13 | 69 | 0.94 |
| Female | 16 | 68 | |
| Cytogenetics | |||
| t(15;17) alone | 17 | 88 | 0.12 |
| t(15;17) + Other | 6 | 50 | |
| Clinical Stasis | |||
| Yes | 23 | 70 | 0.58 |
| No | 6 | 67 | |
| WBC | |||
| </=100 | 17 | 77 | 0.64 |
| >100 | 12 | 57 | |
| Platelets | |||
| </=20 | 11 | 62 | 0.9 |
| >20 | 18 | 72 | |
| Fibrinogen | |||
| </=200 | 11 | 64 | 0.43 |
| >200 | 16 | 75 | |
| Leukapheresis | |||
| Yes | 11 | 73 | 0.64 |
| No | 18 | 67 | |
| Regimen | |||
| ATRA/ATO | 15 | 100 | 0.002 |
| Non-ATRA/ATO | 14 | 35 | |
Kantarjian:Sanofi-Aventis: Research Funding. Faderl:Sanofi-Aventis: Membership on an entity’s Board of Directors or advisory committees, Research Funding. Garcia-Manero:Novartis Pharmaceutical: Research Funding. Verstovsek:Incyte Corporation: Research Funding. Ravandi:Sunesis: Consultancy, Honoraria, Research Funding; Celgene: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Bristol Myers Squibb: Honoraria, Research Funding; Teva: Consultancy, Honoraria; Pfizer: Honoraria; Merck: Research Funding; Bayer/Onyx: Consultancy, Honoraria; EMD Serono: Research Funding; Medimmune: Research Funding; Amgen: Consultancy, Honoraria; Seattle Genetics: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal