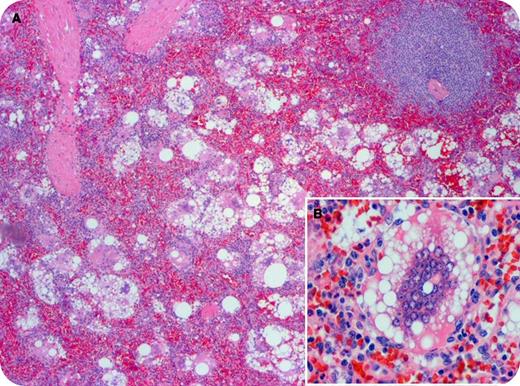
A 59-year-old woman was evaluated for a platelet count of 105 × 109/L, splenomegaly, and associated symptoms of fatigue, early satiety, and nausea. She had history of breast cancer treated with lumpectomy followed by prophylactic bilateral mastectomy and placement of silicone breast implants 25 years earlier. Hemoglobin, white blood cell, liver and renal function, vitamin B12, and folate levels were all within normal ranges. The blood smear showed reduced numbers of morphologically normal platelets; platelet antibody studies were negative. Positron emission tomography/computed tomography imaging showed doubling of the spleen size, with normal consistency and intensity. Bone marrow evaluation was noted for mild hypercellularity and megakaryocyte hyperplasia without clonal populations. Splenectomy revealed an enlarged spleen (710g; normal up to 180) with diffuse lipogranulomatosis, characterized by numerous foreign body giant cells (panel A) and histiocytes with abundant cytoplasmic vacuoles (panel B) occupying the red pulp, consistent with silicone toxicity. A magnetic resonance imaging scan of the breasts revealed bilateral capsular implant ruptures. The patient’s platelet count normalized after splenectomy and her symptoms resolved. The silicone breast implants were subsequently removed and replaced with saline filled implants.
Silicone-mediated toxicity with distant tissue lipogranumolatosis is a feature of both silent and symptomatic implant ruptures. Doctors and patients should be aware of the potential of disseminated silicone driving systemic clinical syndromes. Our patient represents a rare description of silicone-mediated lipogranulomatosis generating symptomatic hypersplenism.
A 59-year-old woman was evaluated for a platelet count of 105 × 109/L, splenomegaly, and associated symptoms of fatigue, early satiety, and nausea. She had history of breast cancer treated with lumpectomy followed by prophylactic bilateral mastectomy and placement of silicone breast implants 25 years earlier. Hemoglobin, white blood cell, liver and renal function, vitamin B12, and folate levels were all within normal ranges. The blood smear showed reduced numbers of morphologically normal platelets; platelet antibody studies were negative. Positron emission tomography/computed tomography imaging showed doubling of the spleen size, with normal consistency and intensity. Bone marrow evaluation was noted for mild hypercellularity and megakaryocyte hyperplasia without clonal populations. Splenectomy revealed an enlarged spleen (710g; normal up to 180) with diffuse lipogranulomatosis, characterized by numerous foreign body giant cells (panel A) and histiocytes with abundant cytoplasmic vacuoles (panel B) occupying the red pulp, consistent with silicone toxicity. A magnetic resonance imaging scan of the breasts revealed bilateral capsular implant ruptures. The patient’s platelet count normalized after splenectomy and her symptoms resolved. The silicone breast implants were subsequently removed and replaced with saline filled implants.
Silicone-mediated toxicity with distant tissue lipogranumolatosis is a feature of both silent and symptomatic implant ruptures. Doctors and patients should be aware of the potential of disseminated silicone driving systemic clinical syndromes. Our patient represents a rare description of silicone-mediated lipogranulomatosis generating symptomatic hypersplenism.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal