Abstract
Abstract 2998
GvHD remains the most deadly complication of HSCT despite current prevention strategies. To address the unmet need for better GvHD control, we have created a non-human primate (NHP) model with which to rigorously test mechanism and efficacy of novel therapeutics. In this study, we determined whether a novel combination of mTOR inhibition (with sirolimus) and CD28:CD80/86 costimulation blockade (with belatacept) could control GvHD. Here we show for the first time that these two agents combine synergistically to prevent both the clinical and immunologic manifestations of primate aGvHD.
Rhesus macaque recipients were irradiated (9.6 Gy in 2 fractions at 7cGy/min), and then transplanted with G-CSF-mobilized PBSC from a haplo-identical donor (1–5×108 TNC/kg). Recipients were treated with either sirolimus alone (n = 4, troughs targeted at 5–10 ng/mL), belatacept alone (receiving weekly doses of 20 mg/kg), or combination therapy. Clinical GvHD was monitored using our previously described NHP grading scale (Miller et al., Blood 2010), and multiparameter flow cytometric analysis was performed.
Untreated controls (n = 5) developed rapid, severe histopathologically-proven aGvHD and succumbed rapidly (MST = 7 days). Recipients treated with either sirolimus or belatacept alone were partially protected from the clinical manifestations of GvHD. Sirolimus-treated recipients (n = 6) developed predominantly GI disease (with diarrhea but no elevation of bilirubin) and had an MST of 14 days (Figure 1). Recipients treated with belatacept alone (n = 3) developed primarily liver aGvHD (bilirubin rapidly rising to 6–30 × normal with histologically-confirmed lymphocytic infiltration) and an MST of 11 days. In striking contrast, recipients treated with combined sirolimus + belatacept (n = 5) demonstrated neither uncontrolled diarrhea nor hyperbilirubinemia at the timed terminal analysis (1 month post-transplant).
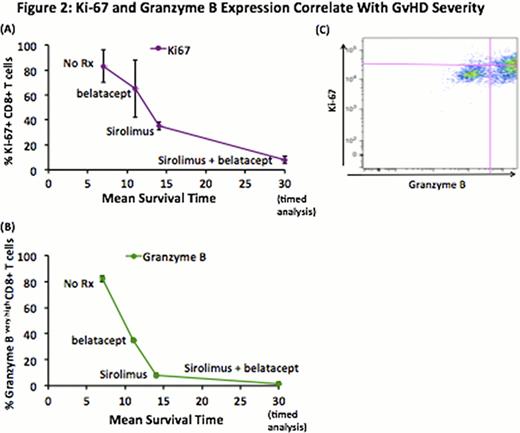
We employed multiparameter flow cytometry to determine the immunologic consequences of sirolimus and belatacept on T cell proliferation (using Ki-67 expression) and cytotoxity (using granzyme B expression). We found that the clinical synergy observed with combined therapy was recapitulated immunologically. Thus, while untreated aGvHD was associated with rampant CD8+ proliferation (with 83 +/− 14% Ki-67+ CD8+ vs 4.7 +/− 0.6% pre-transplant), sirolimus or belatacept as monotherapy both partially controlled proliferation (35 +/− 3% and 65 +/− 23% Ki-67+ CD8+ with sirolimus or belatacept, respectively). Combined sirolimus + belatacept dramatically reduced proliferation (to 8 +/− 3%, favorably comparing with 13% Ki-67+ CD8+ T cells using standard Calcineurin Inhibitor/Methotrexate (CNI/MTX) prophylaxis).
Sirolimus and belatacept both also partially controlled GvHD-related T cell cytotoxicity. Thus, while untreated aGvHD was associated with excessive granzyme B expression in CD8+ T cells (82 +/− 2% granzyme Bvery high CD8+ cells vs 0.3 +/− 0.2% pre-transplant) sirolimus or belatacept monotherapy also partially controlled cytotoxicity (8 +/− 1% and 35 +/− 1% granzyme Bvery high with sirolimus or belatacept, respectively). Combination therapy dramatically reduced the proportion of these cells, to 1.5 +/− 0.8 % granzyme Bvery high, favorably comparing with 4% granzyme Bvery high using CNI/MTX.
The ability of sirolimus, belatacept, or the combination to control Ki-67 and Granzyme B expression closely correlated with survival (Figure 2A, B) supporting a pathogenic role for these highly proliferative and cytotoxic cells in aGvHD pathology. Moreover, significant co-expression of granzyme B in the Ki-67+ cells was observed (Figure 2C) suggesting that dual-positive Ki-67/Granzyme B cells may mark a pathogenic population, amenable to tracking in the peripheral blood.
These results reveal a previously undiscovered synergy between sirolimus and belatacept in the control of primate aGvHD, and provide support for future clinical investigation of this novel prevention strategy. They also identify CD8+/Ki-67+/Granzyme Bvery high dual-positive T cells as a potentially sensitive biomarker of GvHD pathogenesis, amenable to monitoring in either the blood or in GvHD target organs.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal