Abstract
Ras proteins are critical nodes in cellular signaling that integrate inputs from activated cell surface receptors and other stimuli to modulate cell fate through a complex network of effector pathways. Oncogenic RAS mutations are found in ∼ 25% of human cancers and are highly prevalent in hematopoietic malignancies. Because of their structural and biochemical properties, oncogenic Ras proteins are exceedingly difficult targets for rational drug discovery, and no mechanism-based therapies exist for cancers with RAS mutations. This article reviews the properties of normal and oncogenic Ras proteins, the prevalence and likely pathogenic role of NRAS, KRAS, and NF1 mutations in hematopoietic malignancies, relevant animal models of these cancers, and implications for drug discovery. Because hematologic malignancies are experimentally tractable, they are especially valuable platforms for addressing the fundamental question of how to reverse the adverse biochemical output of oncogenic Ras in cancer.
Introduction
Aberrant signal transduction resulting in reduced dependence on growth factors and other extracellular stimuli for the survival and proliferation of malignant cells is an established “hallmark of cancer.”1 RAS genes encode a family of 21-kDa proteins that are central nodes in signaling networks that regulate cell fate in many tissue lineages. RAS genes are also the most common targets of dominant somatic mutations in human cancer.2,3 The high prevalence of mutations in NRAS, KRAS, and molecules, such as CKIT, PTPN11, CBL, and BCR-ABL1, that interact with Ras biochemically strongly implicate aberrant Ras signaling as an important therapeutic target in these cancers.4-7 In this review, we focus on the pathobiology of mutations in hematologic cancers involving the “core” Ras-GTPase activating protein (GAP) complex, which includes Ras itself, guanine nucleotide exchange factors, and GAPs. At this writing, mutations in NRAS, KRAS, and the NF1 tumor suppressor, which encodes a GAP called neurofibromin,8 are strongly associated with myeloid malignancies. Increasing evidence also implicates these genes as “drivers” in lymphoid cancers with “high-risk” clinical features. No mechanism-based treatments exist for the ∼ 25% of human cancers with KRAS or NRAS mutations or for the growing number of malignancies showing NF1 inactivation, and we discuss potential therapeutic strategies for addressing the adverse biochemical consequences of aberrant Ras signaling.
Structural and functional properties of the Ras GTPase switch
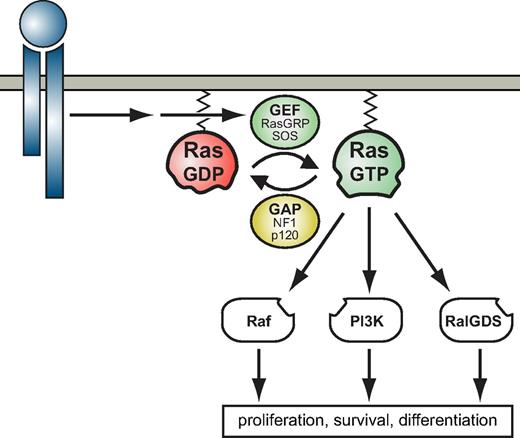
Ras proteins are signal switch molecules that regulate cell fates by cycling between active guanosine triphosphate (GTP)–bound and inactive guanosine diphosphate (GDP)–bound conformations.9 On ligand binding, molecules, such as Shc, Grb2, Gab2, and SHP-2, are recruited to growth factor receptors and these complexes activate Ras guanine nucleotide exchange factors (GEFs; Figure 1).10 GEFs catalyze dissociation of guanine nucleotides from Ras, which is followed by passive rebinding. Because the concentration of free GTP in cells vastly exceeds that of GDP, GEF-induced nucleotide exchange increases Ras-GTP levels.10 Ras can be activated by a number of different GEFs in mammalian cells, including SOS1 and SOS2, RasGRFS1 and RasGRFS2, and RasGRP1 to RasGRP4 (Figure 1).2
The Ras switch. Ras proteins are switches that relay signals initiated when transmembrane receptors bind ligand. Activated receptors recruit GEFs by assembly of multiprotein complexes (eg, including SOS) or more indirectly, by evoking lipid modifications that recruit GEFs, such as RasGRPs, to cytosolic membrane surfaces. GEFs promote exchange of GDP for GTP on Ras. When bound to GTP, Ras adopts a conformation in which the “switch” regions are stabilized and can interact productively with various downstream effectors. Thus, Ras connects extracellular stimuli to intracellular networks that compute and execute cell fate decisions. The Ras signal is terminated by GTP hydrolysis, which is largley dependent on GAPs, such as neurofibromin (NF1) or p120 RasGAP.
The Ras switch. Ras proteins are switches that relay signals initiated when transmembrane receptors bind ligand. Activated receptors recruit GEFs by assembly of multiprotein complexes (eg, including SOS) or more indirectly, by evoking lipid modifications that recruit GEFs, such as RasGRPs, to cytosolic membrane surfaces. GEFs promote exchange of GDP for GTP on Ras. When bound to GTP, Ras adopts a conformation in which the “switch” regions are stabilized and can interact productively with various downstream effectors. Thus, Ras connects extracellular stimuli to intracellular networks that compute and execute cell fate decisions. The Ras signal is terminated by GTP hydrolysis, which is largley dependent on GAPs, such as neurofibromin (NF1) or p120 RasGAP.
GTP binding stabilizes the switch I and switch II domains of Ras, which then interacts productively with effectors.9 These effector molecules are activated biochemically through complex mechanisms that involve recruitment to discrete subcellular compartments, increasing intrinsic catalytic activity and/or inducing conformational changes that allow effectors to act as scaffolds for the assembly of signaling complexes.11,12 Three canonical Ras effectors have been the focus of intense study: PI3-kinase (PI3K), Raf, and Ral-GDS proteins (Figure 1). Of these, aberrant activation of the Raf/MEK/ERK pathway and the PI3K/Akt/mTOR cascade is most strongly implicated in malignant transformation and tumor maintenance. We refer interested readers to detailed reviews of individual effector pathways.2,13
Signaling is terminated when Ras-GTP is hydrolyzed to Ras-GDP. This “off” reaction is catalyzed by intrinsic Ras GTPase activity, which is inefficient in the absence of GAPs. GAPs bind to the switch domains of Ras-GTP and insert an “arginine finger” into the phosphate binding loop of Ras that stabilizes a transition state between Ras-GTP and Ras-GDP.2,8 Because GAPs accelerate GTP hydrolysis thousands of fold, some view the Ras-GTPase as enzyme complex composed of Ras and a GAP. Neurofibromin, the protein encoded by NF1, and p120 GAP are the predominant Ras GAPs in mammalian cells, and both are expressed broadly.8,14 Given the central role of Ras signaling in cellular homeostasis, it is perhaps not surprising that germline mutations in NF1 and other genes that regulate Ras-GTP levels also cause developmental disorders.2,10
Ras isoforms, posttranslational modifications, and intracellular trafficking
RAS genes encode 4 highly homologous proteins (H-Ras, N-Ras, K-Ras4a, and K-Ras4b) that are identical in the first 85 amino acids. This “G” domain includes the P-loop, which interacts with the γ-phosphate of GTP, and the switch regions (Figure 2).2,10 Ras proteins share 85% identity over the next 80 amino acids and only diverge substantially at the C-terminal “hypervariable region” (Figure 2).2 The hypervariable region of all Ras isoforms terminates with a CAAX motif, where the cysteine is prenylated by farnesyltransferase (FTase). After prenylation, the —AAX of the CAAX motif is removed by Ras-converting enzyme 1, and the carboxyl group of the newly exposed isoprenylcysteine is methylated by isoprenylcysteine-carboxyl-methyltransferase (ICMT). These lipid modifications provide weak membrane binding affinity that is stabilized by a second signal motif. For K-Ras4b, this is provided by a polybasic lysine domain, which interacts strongly with the phospholipid membrane. By contrast, H-, N-, and K-Ras4a are palmitoylated at cysteine(s) adjacent to the CAAX motif (Figure 2). These modifications are essential for correct trafficking and subcellular localization of each isoform.15 In particular, whereas H-, N-, and K-Ras4a are directed from the endoplasmic reticulum (ER) to the Golgi en route to the plasma membrane (PM), K-Ras4b localizes directly to the PM through an unknown mechanism. A significant portion of H-Ras, N-Ras, and K-Ras4a reside and signal in the Golgi and ER, and these proteins traffic between the Golgi, ER, and PM in a dynamic cycle that is regulated by depalmitoylation and repalmitoylation.15 Depalmitoylation is mediated by acyl protein thioesterase 1 and acyl protein thioesterase 2.15 By contrast, there are at least 20 palmitoyl transferases, and it is uncertain which of these act on individual Ras proteins.16 Perturbation of palmitate turnover leads to nonspecific distribution of H-Ras, N-Ras, and K-Ras4a to endomembranes and decreases signaling from the PM.17
Ras processing and trafficking to subcellular compartments. H-Ras, N-Ras, K-Ras4a, and K-Ras4b proteins are identical in the first 85 amino acids, a region that includes the P loop (phosphate binding loop, amino acids 10-16), which binds the γ-phosphate of GTP, and the switch I (amino acids 30-38) and switch II (amino acids 60-76) regions, which regulate binding to Ras regulators and effectors. The next 78 amino acids show ∼ 85%-90% sequence homology. Amino acids that are shared by all isoforms are depicted in light gray, those that differ are depicted in dark gray. The final 24 (23 for K-Ras4b) amino acids, called the hypervariable region (HVR), specify posttranslational modifications and trafficking for each Ras isoform. All 4 isoforms have a C-terminal —CAAX motif, which is farnesylated (F) by FTase. The —AAX is removed by Ras-converting enzyme 1 (RCE1) and the cysteine methylated (M) by ICMT. K-Ras4b is then shuttled directly to the PM where it is stabilized by its polylysine domain (KKKKKK). The other 3 isoforms are shuttled to the Golgi apparatus, where they are palmitoylated (P) at one or more cysteines near the C-terminus before reaching the plasma membrane. On the membrane, H-Ras, N-Ras, and K-Ras4a can be depalmitoylated by acyl protein thioesterases 1 and 2 (APT1/APT2), directing them back to the Golgi. This palmitoylation-depalmitoylation, Golgi-plasma membrane cycle continues in a delicate balance until the proteins are degraded.
Ras processing and trafficking to subcellular compartments. H-Ras, N-Ras, K-Ras4a, and K-Ras4b proteins are identical in the first 85 amino acids, a region that includes the P loop (phosphate binding loop, amino acids 10-16), which binds the γ-phosphate of GTP, and the switch I (amino acids 30-38) and switch II (amino acids 60-76) regions, which regulate binding to Ras regulators and effectors. The next 78 amino acids show ∼ 85%-90% sequence homology. Amino acids that are shared by all isoforms are depicted in light gray, those that differ are depicted in dark gray. The final 24 (23 for K-Ras4b) amino acids, called the hypervariable region (HVR), specify posttranslational modifications and trafficking for each Ras isoform. All 4 isoforms have a C-terminal —CAAX motif, which is farnesylated (F) by FTase. The —AAX is removed by Ras-converting enzyme 1 (RCE1) and the cysteine methylated (M) by ICMT. K-Ras4b is then shuttled directly to the PM where it is stabilized by its polylysine domain (KKKKKK). The other 3 isoforms are shuttled to the Golgi apparatus, where they are palmitoylated (P) at one or more cysteines near the C-terminus before reaching the plasma membrane. On the membrane, H-Ras, N-Ras, and K-Ras4a can be depalmitoylated by acyl protein thioesterases 1 and 2 (APT1/APT2), directing them back to the Golgi. This palmitoylation-depalmitoylation, Golgi-plasma membrane cycle continues in a delicate balance until the proteins are degraded.
Structural properties of oncogenic Ras proteins and therapeutic implications
Somatic point mutations of RAS genes at codons 12, 13, and 61 are the most common dominant oncogenic lesions in human cancer.2 Substitutions in these residues favor the GTP-bound conformation because of reduced intrinsic GTP hydrolysis and resistance to GAPs.2 The oncogenic Ras/GAP switch is an exceedingly difficult target for rational drug discovery. The most tractable molecular targets in cancer, such as BCR-ABL, the mutant epidermal growth factor receptor (EGFR), and B-RafV600E, are aberrantly activated kinases that are inhibited by selective small-molecule inhibitors. By contrast, oncogenic Ras proteins have reduced GTPase activity.2 Restoring enzymatic function, the fundamental biochemical problem posed by oncogenic Ras, is extremely challenging. Developing mechanism-based inhibitors of oncogenic Ras is further complicated by the picomolar affinity of Ras for GTP and by high intracellular GTP concentrations.18 Finally, the P loop of Ras is structurally constrained, with any amino acid substitution at glycines 12 or 13 introducing space-occupying side chains that distort the interaction with GAPs.9 It is therefore difficult to envision how small molecules might bind to Ras and restore GAP-mediated GTP catalysis. For these reasons, recent drug discovery efforts have largely focused on inhibiting kinase components of downstream effector pathways, such as PI3K, Akt, mammalian target of rapamycin (mTOR), and MEK.
NRAS, KRAS, and NF1 mutations in hematologic cancers
Different RAS genes are preferentially mutated in distinct tumor types, with KRAS mutations highly prevalent in common epithelial malignancies.2 As summarized in the next 5 sections and in Table 1, hematologic cancers are unusual in that NRAS and KRAS are both mutated at significant frequencies, with NRAS mutations predominating. NF1 is the only Ras GAP implicated in tumorigenesis to date. Although mutations in Ras GEFs have been linked to the development of drug resistance in mouse models of hematologic malignancies,19 other mutations in this family of molecules are rare in human cancers (COSMIC database).
Incidence of NRAS, KRAS, and NF1 mutations in hematologic malignancies
| . | NRAS . | KRAS . | NF1 . |
|---|---|---|---|
| JMML | 17% (9-30) | 8% (3-18) | 7% (4-15) |
| CMML | 19% (2-43) | 11% (6-15) | ND |
| AML | 11% (10-44) | 5% (1-13) | ∼ 5% (0-7) |
| MDS | 5% (4-9) | ∼ 1% | ∼ 3% (0-9) |
| ALL | 10% (0-18) | 4% (0-5) | 6% (3-8)* |
| MM | 18% (17-30) | 8% (6-9) | ND |
| . | NRAS . | KRAS . | NF1 . |
|---|---|---|---|
| JMML | 17% (9-30) | 8% (3-18) | 7% (4-15) |
| CMML | 19% (2-43) | 11% (6-15) | ND |
| AML | 11% (10-44) | 5% (1-13) | ∼ 5% (0-7) |
| MDS | 5% (4-9) | ∼ 1% | ∼ 3% (0-9) |
| ALL | 10% (0-18) | 4% (0-5) | 6% (3-8)* |
| MM | 18% (17-30) | 8% (6-9) | ND |
These data are tabulated from published series that used the current definition for each disease, distinguished clearly between NRAS and KRAS mutations and, with 1 exception (*T-ALL only), did not restrict inclusion based on an underlying genetic alteration or specific subtype of disease. The supplemental Materials (available on the Blood Web site; see the Supplemental Materials link at the top of the online article) include tables and references listing the primary sources for the data shown here by disease category, along with the number of cases sequenced in each report.
ND indicates not determined.
JMML and CMML
These aggressive myeloid malignancies are classified as myelodysplastic syndrome/myeloproliferative neoplasia (MDS/MPN) “overlap” syndromes by the World Health Organization. A distinctive pattern of hypersensitive CFU-GM progenitor growth in methylcellulose cultures containing GM-CSF is a cellular hallmark of juvenile myelomonocytic leukemia (JMML) that is also observed in some cases of chronic myelomonocytic leukemia (CMML).20
The association between neurofibromatosis type 1 (NF1) and JMML pointed the way toward our current understanding of the underlying molecular pathogenesis.20 Genetic analysis of JMML bone marrow specimens from children with NF1 revealed somatic loss of the normal NF1 allele, elevated levels of Ras-GTP, and activation of the Raf/MEK/ERK effector pathway.20 Sequencing revealed NF1 mutations in ∼ 15% of patients with JMML, suggesting that other genes involved in Ras signaling might also be mutated. Indeed, molecular analysis demonstrating somatic NRAS and KRAS in 25%-30% of JMML patients, and subsequent research identifying PTPN11 and CBL mutations firmly established JMML as a disease of hyperactive Ras.20 Furthermore, the observation that children with NF1 and certain other developmental disorders are predisposed to JMML provided strong evidence that hyperactive Ras/Raf/MEK/ERK signaling initiates this disease.2
NRAS and CBL mutations are highly prevalent in CMML.4,21 Whereas RAS mutations are found in > 20% of patients with the myeloproliferative variant of CMML, they are rare in the more benign myelodysplastic variant.22,23 It is uncertain whether hyperactive Ras signaling can initiate leukemogenesis in CMML or whether mutations in genes that are involved in epigenetic programming are also required.24 However, there is some evidence to support the role of cooperation between hyperactive Ras signaling and transcription factor mutations in acute transformation of CMML.25
AML
The 2 largest published series identified NRAS codon 12, 13, or 61 mutations in 10%-11% of adult acute myeloid leukemia (AML), and KRAS mutations in an additional 5%.26,27 A similar incidence of NRAS/KRAS mutations is observed in pediatric patients.28,29 NRAS/KRAS mutations do not have independent prognostic significance in patients treated with current antileukemia regimens, although patients with AML harboring a RAS mutation may respond better to high-dose cytarabine as post-remission therapy.30 Recently, high-throughput sequencing revealed novel NRAS and KRAS mutations in AML and CMML that introduce substitutions at amino acids 14, 60, 74, and 146 in 2%-5% of cases.31 This discovery suggests that 20%-25% of AML carries somatic NRAS/KRAS mutations. Loss of NF1 expression was reported in 7 of 95 patients with AML, and 7 additional cases had heterozygous NF1 loss.32
Observations in JMML and CMML and studies of genetically engineered mice summarized in “Insights from mouse models” provide compelling evidence that NF1, NRAS, and KRAS mutations are early or initiating events in some myeloid malignancies, particularly MDS/MPN overlap disorders. The picture is more complex in AML, with existing data suggesting that these mutations may function as either early/initiating or as cooperating mutations that are acquired during disease progression. RAS and NF1 mutations are over-represented in the French-American-British (FAB) M4 and M5 monocytic subtypes, with an overall incidence of > 30%.26,27,32 Interestingly, JMML and CMML also evolve to M4/M5 AML,31,33 and leukemia cells from patients with JMML, CMML, and FAB M4/M5 AML exhibit a similar signature of phospho-protein activation characterized by aberrant STAT5 activation at low GM-CSF concentrations.34 Together with the absence of consistent transcription factor mutations in FAB M4/M5 AML, these data raise the possibility that M4/M5 AML, JMML, and CMML are related malignancies in which NRAS/KRAS/NF1 play an early and essential role in leukemic growth.34,35
A popular model suggests that initiation of AML requires both a “class 1” mutation that aberrantly activates signal transduction and a “class 2” mutation in a transcription factor.36 Recent studies demonstrating a high frequency of heterozygous and homozygous mutations in genes that broadly regulate the eipgenome, such as TET2, EZH2, IDH1, IDH2, and DNMT3A, and other lines of evidence indicate that this simple paradigm only partially explains the complex pathogenesis of AML.37 However, it is useful for considering the potential role of NRAS/KRAS/NF1 mutations as cooperating events in leukemogenesis. The observation that activating mutations in FLT3 and CKIT, which encode receptor tyrosine kinases upstream of Ras, are common in AML and largely confined to cases without RAS mutations supports the broad relevance of “class 1” mutations in AML. Furthermore, several groups have shown that RAS and FLT3 mutations can be lost or gained during disease evolution in AML and MDS.38,39 Indeed, cases with an NRAS mutation at diagnosis may demonstrate a FLT3 mutation at relapse (and vice versa), and NRAS mutations are associated with acquired resistance to Flt3 kinase inhibitors in vitro.40 These studies are consistent with the idea that mutations that alter signaling molecules are secondary events that contribute to clonal evolution in many patients with AML.
MDS/MPNs
Initial studies demonstrating somatic NRAS mutations in 20%-40% of MDS included patients with CMML, which undoubtedly inflated these numbers. Recent data indicate that NRAS is mutated in ∼ 5% of MDS where it is associated with adverse clinical features and a high risk of transformation to AML.41,42 KRAS mutations are rare in MDS.42 Although there are limited data on somatic NF1 inactivation in MDS, recurrent cryptic changes or deletions involving the NF1 locus were identified in 3 of 35 patients.43 Mutations in BRAF, PTPN11, CBL, FLT3, CKIT, and other genes encoding signaling molecules that interact with Ras are also uncommon in MDS.44 Taken together, although the existing data do not support an integral role of NRAS/KRAS/NF1 mutations in the development of MDS, they probably contribute to transformation to AML. By contrast, mutations that deregulate signaling networks are integral to the pathogenesis of MPN and NRAS/KRAS/NF1 mutations are therefore not implicated in progression to acute leukemia.45
ALL
There are limited data regarding RAS mutations in lymphoid malignancies, particularly in adults. One small study suggested that ∼ 11% of adult T lineage acute lymphoblastic leukemia (T-ALL) patients harbor RAS mutations.46 Neri et al identified RAS mutations in 6 of 33 ALL cases (18%), all of which were in codon 12 or 13 of NRAS, although patient age was not reported.47 In the pediatric literature, estimates of RAS mutation frequency in both B- and T-lineage ALL approximate 15%, with NRAS mutations predominating.48,49
Early T-cell precursor ALL is a recently identified subtype of pediatric ALL with a distinct gene expression profile and an immunophenotype notable for expression of stem cell and myeloid markers.50 Children with this form of leukemia have high rates of induction failure, as well as extremely high risk of relapse.50 Whole-genome sequencing recently uncovered mutations in genes involved in Ras signaling in 67% of early T-cell precursor ALL cases (19% NRAS, 3% KRAS, 14% FLT3, and the remainder in JAK1, JAK3, BRAF, and IGFR1).48 These data suggest that early T-cell precursor ALL may be initiated by NRAS/KRAS and other “driver” mutations that are commonly identified in myeloid malignancies in a multipotent hematopoietic stem/progenitor cell. Somatic NF1 mutations were also reported recently in some human T-ALLs.51
MM
RAS is the single most commonly mutated gene family in multiple myeloma (MM).52 Whereas early publications estimated the frequency of NRAS/KRAS mutations in MM as high as 30%-40%,53-55 a comprehensive recent study identified codon 12, 13, or 61 RAS mutations in 23% of 529 patients.52 Of these, two-thirds were in the NRAS gene (mostly in codon 61), with the remainder in KRAS (largely in codons 12 and 13). RAS mutations predict shorter overall survival and progression-free survival in MM, but are rare in monoclonal gammopathy of unknown significance, a precursor to MM in some patients.52,53 Furthermore, as in AML, RAS gene mutations are occasionally not detected at diagnosis but found at relapse. Although not definitive, these data suggest that NRAS/KRAS mutations are more likely to be involved in MM progression rather than initiation.52,53,55
Insights from mouse models
Ras oncogenes have been studied extensively in the mouse, both to elucidate the mechanisms underlying deregulated growth and to develop robust in vivo platforms for performing preclinical trials. Table 2 presents a partial list of informative models of hematologic malignancies. One strong theme that has emerged is that either inactivating Nf1 or expressing oncogenic Kras from its endogenous genetic locus in the hematopoietic compartment is sufficient to produce a myeloproliferative disorder that models human MDS/MPN. This highly penetrant phenotype progresses rapidly in Mx1-Cre; KrasG12D mice.35,56 Interestingly, similar models based on endogenous NrasG12D expression demonstrated a mild and variable myeloid phenotype,57-59 although mice that are homozygous for a conditional NrasG12D knock-in allele consistently develop aggressive MPN.59,60 Together, these data support the idea that differences in the structure and/or expression levels of different Ras isoforms influence the severity of myeloid growth dysregulation, which may have implications for therapeutic development.
Mouse models of hematologic malignancies characterized by KRAS, NRAS, or NF1 mutations
| Allele . | Model type . | Genotype . | Phenotype(s) . | References . |
|---|---|---|---|---|
| KrasG12D | Heterozygous conditional “knock in” | Mx1-Cre; KrasG12D/+ | Aggressive MPN | 35, 56 |
| KrasG12D | Adoptive transfer of conditional “knock in” marrow into irradiated recipients | Mx1-Cre; KrasG12D/+ | T-ALL | 65, 108 |
| KrasG12D | Conditional “knock in” + retroviral insertional mutagenesis | Mx1-Cre; KrasG12D/+ | T-ALL (∼ 80%); AML (∼ 20%) | 66 |
| NrasG12D | Retroviral transduction/transplantation | WT cells expressing exogenous NrasG12D | CMML, AML | 69, 70, 71 |
| NrasG12D | Heterozygous conditional “knock in” | Mx1-Cre; NrasG12D/+ | Indolent MPN, MDS, LPD, HS | 57, 58, 75 |
| NrasG12D | Homozygous conditional “knock in” | Mx1-Cre; NrasG12D/G12D | Aggressive MPN | 59, 60 |
| NrasG12D | Heterozygous conditional “knock in” + retroviral insertional mutagenesis | Mx1-Cre; NrasG12D/+ | AML | 58 |
| Nf1− | Heterozygous germline “knock out” | Nf1+/− | Late-onset MPN in ∼ 10% of mice | 109 |
| Nf1− | Adoptive transfer of homozygous “knock out” fetal liver cells | Nf1−/− | Subactute MPN | 110 |
| Nf1− | Heterozygous “knock out” + irradiation | Nf1+/− | MDS, MPN | 72, 73 |
| Nf1flox | Homozygous conditional “knock out” | Mx1-Cre; Nf1flox/flox | MPN | 74 |
| Nf1flox | Homozygous conditional “knock out” + retroviral insertional mutagenesis | Mx1-Cre; Nf1flox/flox | AML (∼ 70%); T-ALL (∼ 30%) | 19 |
| Allele . | Model type . | Genotype . | Phenotype(s) . | References . |
|---|---|---|---|---|
| KrasG12D | Heterozygous conditional “knock in” | Mx1-Cre; KrasG12D/+ | Aggressive MPN | 35, 56 |
| KrasG12D | Adoptive transfer of conditional “knock in” marrow into irradiated recipients | Mx1-Cre; KrasG12D/+ | T-ALL | 65, 108 |
| KrasG12D | Conditional “knock in” + retroviral insertional mutagenesis | Mx1-Cre; KrasG12D/+ | T-ALL (∼ 80%); AML (∼ 20%) | 66 |
| NrasG12D | Retroviral transduction/transplantation | WT cells expressing exogenous NrasG12D | CMML, AML | 69, 70, 71 |
| NrasG12D | Heterozygous conditional “knock in” | Mx1-Cre; NrasG12D/+ | Indolent MPN, MDS, LPD, HS | 57, 58, 75 |
| NrasG12D | Homozygous conditional “knock in” | Mx1-Cre; NrasG12D/G12D | Aggressive MPN | 59, 60 |
| NrasG12D | Heterozygous conditional “knock in” + retroviral insertional mutagenesis | Mx1-Cre; NrasG12D/+ | AML | 58 |
| Nf1− | Heterozygous germline “knock out” | Nf1+/− | Late-onset MPN in ∼ 10% of mice | 109 |
| Nf1− | Adoptive transfer of homozygous “knock out” fetal liver cells | Nf1−/− | Subactute MPN | 110 |
| Nf1− | Heterozygous “knock out” + irradiation | Nf1+/− | MDS, MPN | 72, 73 |
| Nf1flox | Homozygous conditional “knock out” | Mx1-Cre; Nf1flox/flox | MPN | 74 |
| Nf1flox | Homozygous conditional “knock out” + retroviral insertional mutagenesis | Mx1-Cre; Nf1flox/flox | AML (∼ 70%); T-ALL (∼ 30%) | 19 |
Although the role of Ras pathway activation has been more thoroughly described in the development of myeloid disease, growing evidence implicates hyperactive Ras in the development of lymphoid cancers as well. Lymphoid transformation was observed in early studies of primary hematopoietic cells expressing mutant Ras,61 and spontaneous T-ALL is a common finding in transgenic mouse models bearing Ras oncogenes.62-64 In retrospect, such studies predicted the presence of Ras pathway mutations in human lymphoid leukemia (see “ALL”). T-ALL can be induced in KrasG12D mice by transplanting limiting numbers of hematopoietic stem cells into irradiated recipients or by retroviral insertional mutagenesis.65-67 Mutations leading to Notch1 activation are common in this setting, and strong synergy exists between these 2 human leukemia oncogenes.68
It is probable that additional mutations contribute to leukemic outgrowth initiated by oncogenic Ras or Nf1 inactivation in other contexts. Bone marrow transduced with retroviral vectors encoding oncogenic Kras or Nras can cause AML in recipient mice after transplantation, and these cancers exhibit clonal retroviral integrations.69-71 Retroviral insertional mutagenesis in Nf1, Kras, and Nras mutant mice was deployed as a forward genetic strategy to identify mutations that might cooperate with hyperactive Ras in leukemogenesis.19,58,66 These studies implicated Evi1, Myb, Sox4, and Gfi1 in AML initiated by Nras or Nf1 inactivation, and Ikzf1 in Kras mutant mice with T-ALL. Consistent with reports of therapy-induced hematologic cancers in patients with NF1, heterozygous Nf1 inactivation cooperates with radiation to induce MDS and MPN in mice.72,73
Hematopoietic cells that either express endogenous levels of oncogenic NrasG12D or KrasG12D or have inactivated Nf1 demonstrate a hypersensitive pattern of CFU-GM progenitor colony growth in response to GM-CSF that recapitulates what is observed in JMML and in some patients with CMML.20,35,58,74 Consistent with in vivo observations, this cellular phenotype is most pronounced in cells from Mx1-Cre; KrasG12D/+ and homozygous Mx1-Cre; NrasG12D/G12D mice, but relatively subtle in Mx1-Cre; NrasG12D/+ and Mx1-Cre; Nf1flox/flox cells. Whereas biochemical analysis of bone marrow cells from these mutant mice revealed elevated basal levels of phosphorylated ERK (pERK), the degree of activation was unexpectedly subtle and bone marrow cells markedly increased pERK levels in response to growth factor stimulation.35,59,60,74,75 Detailed biochemical profiling of Nf1 and Nras mutant AMLs has not been reported. Interestingly, however, although T-ALL cells from Kras mutant mice have constitutively high Ras-GTP levels, pERK, pAkt, and pS6 levels were highly variable.66 Together, biochemical studies of mouse leukemias support the idea that primary hematopoietic cells dynamically modulate signaling networks in response to increased Ras-GTP levels, which has implications for the use of targeted therapeutics.
Therapeutic strategies for inhibiting Ras processing and activation
Inhibiting posttranslational processing of Ras engendered intense interest in the 1990s. Drug discovery efforts focused on the essential lipid modification at CAAX sequence that is catalyzed by FTase.76 Clinical trials of selective and potent FTase inhibitors were largely disappointing,76,77 probably because K-Ras and N-Ras undergo lipid modification via geranylgeranyl transferase when FTase is inhibited and therefore retain biologic activity.76 Indeed, a preclinical trial of the FTase inhibitor L744,832 in mice that developed MPN after adoptive transfer of Nf1-deficient hematopoietic cells revealed no inhibition of K- or N-Ras processing at the maximally tolerated dose and no improvement in leukocyte counts or splenomegaly.78 Off-target effects may explain the clinical responses to FTase inhibitors reported in some leukemias.77,79 Unfortunately, combining FTase and geranylgeranyl transferase inhibition proved too toxic to represent a viable therapeutic regimen.76
Genetic studies in mice investigated the effects of interfering with C-terminal processing of prenylated Ras proteins by Ras-converting enzyme 1 and ICMT. Inactivating Rce1 in hematopoietic cells unexpectedly accelerated MPN in the Mx1-Cre, KrasG12D model of JMML/CMML.80 By contrast, conditional inactivation of Icmt attenuated myeloproliferation in this strain and also dramatically reduced growth-factor independent colony growth in vitro.81 Although the opposite effects of Rce1 and Icmt inactivation on KrasG12D-induced myeloid disease are perplexing, it should be recalled that these enzymes catalyze the posttranslational modification of many other cellular proteins that could modulate the phenotype. Small molecules have been identified that block ICMT activity; however, these compounds have not yet been tested in vivo.82
The palmitoylation/depalmitoylation cycle is a potential therapeutic target for selectively inhibiting the growth of hematologic cancers with NRAS mutations (Figure 2). A recent study reported that mutating the palmitoylation site at cysteine 181 to serine (C181S) in N-RasG12D inhibited plasma membrane localization in fibroblasts and prevented the development of myeloid disease in a retroviral transduction/transplantation model of MPN.83 Xu et al found that the C181S mutation exhibited dominant negative activity on myeloid progenitor growth and ERK activation, probably by sequestering effectors.60 Palmostatin B is a novel APT inhibitor that causes entropy-driven diffusion of H-Ras and N-Ras throughout the cell.84 Exposing transduced hematopoietic cells from Nras and Kras mutant mice to palmostatin B mislocalized N-RasG12D away from the plasma membrane and reduced CFU-GM and AML blast colony growth. Importantly, this inhibition was selective for Nras mutant cells and mapped to the hypervariable region. Together, these studies identify APT inhibitors as a novel class of potential therapeutics in hematologic malignancies with NRAS mutations. Newer and more potent inhibitors in this chemical series were reported recently, although systemic toxicities have not been fully described.85
Blocking growth-promoting signals that converge to activate GEFs is another potential therapeutic strategy for treating cancers characterized by NRAS/KRAS/NF1 mutations. In the case of oncogenic Ras, this raises the question of whether these proteins are truly “constitutively active” or remain dependent on guanine nucleotide exchange for transforming activity. The answer is not known and may depend, at least in part, on cell context and on the nature of the underlying RAS mutation. However, there is some evidence that the mutant Ras/GAP switch is at least partially dependent on growth factor signaling in hematopoietic cells. This dependence is clearest in Nf1-deficient cells where genetic ablation of either Gmcsf or the β-common chain of the GM-CSF receptor markedly attenuates the JMML-like MPN.86,87 Interestingly, primary hematopoietic cells from Mx1-Cre, KrasG12D mice show little basal activation of Raf/MEK/ERK or PI3K/Akt/S6 signaling, and these pathways respond robustly to growth factor stimulation.35,88 It is unclear exactly how upstream inputs promote growth of cells expressing mutant Ras proteins, but the rapid development of AML in Mx1-Cre, KrasG12D mice after Nf1 deletion implies that Ras-GTP levels may be limiting.89 Together, these observations suggest that interfering with growth factor-mediated Ras activation may be beneficial, at least in principle, in some cancers with RAS or NF1 mutations. Along these lines, Maurer et al18 recently identified chemical inhibitors to a novel binding pocket on the surface of Ras. DCA1, a compound from this screen, inhibits Ras activation by interfering with SOS-mediated guanine nucleotide exchange, and probably also has activity against other exchange factors.18 Although the long-term therapeutic potential of this approach is uncertain, treatment with drugs that block “upstream” proteins might be considered in hematologic cancers with NRAS/KRAS/NF1 mutations that respond to growth factor stimulation.
Targeting Ras effector pathways
Intensive effort has focused on developing small-molecule inhibitors of the Raf/MEK/ERK and PI3K/Akt/mTOR cascades. Effectors of oncogenic Ras are “indirect” targets that are activated by the mutant protein, introducing additional complexity. It is now appreciated that oncoprotein expression elicits compensatory responses with unpredictable consequences for downstream pathways. For example, whereas T-ALLs generated by insertional mutagenesis in Mx1-Cre, KrasG12D mice invariably show elevated levels of Ras-GTP, the activation of effectors, such as ERK, Akt, and S6, is highly variable in independent leukemias.66
Although evidence is limited regarding which Ras effector pathways are essential for tumor initiation and which are required for maintenance in vivo, the spectrum of non-RAS mutations offers some insights. Whereas mutations that alter Ras-activated proteins are uncommon in JMML, CMML, and AML, “upstream” genes, such as FLT3, CKIT, CBL, and PTPN11, are frequently mutated in these cancers, suggesting that deregulation of multiple effector pathways is essential for myeloid transformation. By contrast, mutational analysis strongly implicates the PI3K pathway in T-ALL,90 and the recent discovery of activating BRAF mutations in ∼ 4% of MM91 suggests that aberrant Raf/MEK/ERK signaling is an important consequence of RAS mutations in this cancer.
Given the uncertainty regarding which Ras effector(s) are essential for the survival and proliferation of different hematopoietic cancers, evaluating targeted inhibitors in preclinical and clinical trials that include pharmacodynamic monitoring of biochemical endpoints can provide pathogenic as well as clinical insights. Sorafenib, a multikinase inhibitor with activity against Raf proteins, had promising single-agent efficacy in AML with FLT3 mutations in a phase 1 trial.92 However, this may be the result of non-Raf effects, as sorafenib also inhibits Flt3 and other kinases.93 More potent and selective Flt3 inhibitors have shown great promise in AML94 and will certainly supersede sorafenib for directly targeting this mutant protein.
CI-1040 and PD0325901 are allosteric MEK inhibitors that have been evaluated in preclinical models of JMML/CMML, AML, and T-ALL.19,66,95 Whereas CI-1040 was ineffective in Mx1-Cre, Nf1flox/flox mice with MPN,19 PD0325901 induced dramatic hematologic improvement and greatly prolonged survival in the Mx1-Cre, KrasG12D model of JMML/CMML.95 These differential effects may reflect the short duration of in vivo MEK inhibition in the bone marrow cells of mice treated with CI-1040 (∼ 4 hours) versus prolonged effects of PD0325901.19 The beneficial effects of PD0325901 in Mx1-Cre, KrasG12D mice were associated with persistence of Kras mutant cells.95 These observations imply that treatment modulates the biologic behavior of these cells and suggest that it will be important to assess molecular markers of the malignant clone in clinical trials of MEK inhibition in JMML and CMML.
MEK inhibitors were also tested in insertional mutagenesis models of AML initiated by Nf1 inactivation19 and of T-ALL characterized by oncogenic KrasG12D expression.66 Although CI-1040 had no beneficial therapeutic index in Mx1-Cre, Nf1flox/flox mice with MPN, it induced dramatic disease regression and markedly extended survival in recipients transplanted with primary Nf1-deficient AMLs.19 This suggests that cooperating mutations acquired during progression from MPN to AML rendered these aggressive cancers more dependent on Raf/MEK/ERK signaling. All of these mice that initially responded to MEK inhibition ultimately relapsed despite continued treatment. Genetic analysis revealed the emergence of preexisting drug-resistant clones, underscoring the importance of genetic heterogeneity as a cause of resistance to targeted inhibitors.
“First-generation” MEK inhibitors demonstrated efficacy against solid tumors with BRAF mutations but had minimal activity in RAS-mutant tumors.96 Based on these disappointing data and unexpected ocular toxicity, clinical development of CI-1040 and PD0325901 was suspended. Newer MEK inhibitors appear to have less toxicity and greater efficacy against solid tumors harboring RAS mutations. However, it is uncertain whether they are superior to standard therapies, and a recent phase 2 study of the MEK inhibitor AZD6244 in advanced AML showed only modest and transient antitumor activity.97 PI3K signaling is activated in AML blasts, and PI3K inhibitors demonstrated antiproliferative activity in vitro. Although there are a number of PI3K inhibitors in clinical trials for solid tumors, none has yet been tested in humans with hematologic malignancies.
One potential explanation for lack of efficacy of single-agent PI3K/Akt or Raf/MEK/ERK inhibition in RAS-mutant cancers tumors may be the ability of either pathway to overcome inhibition of the other through the release of negative feedback loops or other mechanisms. This provides a rationale for simultaneously inhibiting both major effector pathways in RAS-mutant malignancies. Studies demonstrating synergistic antitumor effects of combining MEK and PI3K/mTOR inhibition in genetically engineered murine solid tumor models supports this general strategy. Finally, other Ras effectors in addition to PI3K/Akt and Raf/MEK/ERK may promote tumor formation and/or maintenance in human malignancies and could also represent potential avenues for acquiring drug resistance.
Identifying synthetic lethal interactions with oncogenic Ras
Performing RNA interference (RNAi) screens to identify “synthetic lethal” interactions between oncogene mutations and other cellular proteins is an emerging strategy for identifying novel therapeutic targets in cancer. The underlying rationale is that 2 mutations compatible with survival on their own may be lethal when combined. The goal of these experiments is to identify genes that, when “knocked down,” selectively kill cells with RAS mutations with the hope that some of these will be tractable targets for drug discovery. Studies performed to date have uncovered novel candidate targets whose suppression results in selective apoptosis of oncogenic KRAS-mutant cell lines, including PLK1, STK33, TBK1, and WT1.98-100 It will be several years before we know whether patients with KRAS-mutant malignancies will benefit from drugs that inhibit any of these targets; however, a number of issues have already emerged. First, there has been little overlap in the candidate genes identified by different groups. Second, genetic dependencies in cancer cell lines may not accurately reflect reality in primary malignances, which, as clinicians know, are exceptionally resilient. Third, reducing the expression of a protein is not equivalent to pharmacologically inhibiting a specific activity of that molecule. For example, many kinases are multidomain proteins that regulate cell growth through enzymatic and nonenzymatic mechanisms. RNAi screens cannot distinguish which of these functions is essential for the growth of transformed cells. Finally, recent experience with RNAi screens emphasizes that it is essential to thoroughly validate “hits” by attempting to rescue the lethal phenotype by re-expressing candidate cDNA molecules that are not inhibited by the knockdown construct used in the initial screen. With these caveats in mind, in vitro and in vivo RNA interference screening is a promising approach for discovering new therapeutic targets in an unbiased manner. A recent study that applied this general strategy to KRAS mutant nonsmall cell lung cancer uncovered a strong synthetic lethal interaction with the GATA2 transcription factor.101 This work was particularly impressive as the authors identified drugable GATA-regulated signaling modules, which they validated by performing in vivo preclinical therapeutic trials in mice. Given the importance of GATA2 in hematopoietic lineage specification, these data have obvious implications for leukemia.
Summary and future directions
Developing therapeutic strategies to reverse the abnormal biochemical output of oncogenic Ras proteins without unacceptable toxicity to normal cellular signaling networks is one of the fundamental problems in cancer. NRAS and KRAS mutations contribute to a spectrum of hematologic malignances, and genetic analysis of human specimens as well as experiments in mouse models support the idea that RAS mutations can initiate leukemic growth or serve as cooperating mutations. The latter observation raises the question of whether targeting oncogenic Ras is worthwhile in cancers, such as AML, where it probably functions as a secondary mutation in most patients. Although the answer to this question is unknown, a reasonable working hypothesis is that any somatic genetic lesion that undergoes positive clonal selection in a substantial percentage of cancers contributes to malignant growth. The recent experience with Flt3 inhibitors in AML supports this idea. Like NRAS, FLT3 mutations have been classified as “class 1” mutations that cooperate with aberrant transcription to induce full leukemic transformation. Early-phase clinical trials of potent and selective Flt3 inhibitors, such as AC220, showed that monotherapy induced remission in some patients with refractory AML.102 Importantly, “gatekeeper” mutations in the Flt3 kinase occur with relapse,103 providing compelling genetic evidence that there is strong selective pressure for AML cells to restore aberrant Flt3 signaling in vivo. Effective biochemical inhibition of oncogenic Ras signaling in human acute leukemias with RAS mutations would probably have similar efficacy.
Treating advanced cancers with kinase inhibitors almost uniformly leads to genotype-specific response followed by regrowth of resistant cells.104,105 Based on this precedent, combining inhibitors of oncogenic Ras signaling with other anticancer agents will probably be essential for sustained efficacy. This general strategy was recently implemented in patients with “high risk” B-lineage ALL and BCR-ABL1 rearrangements with promising results.106 A recent study in lung cancer cells lines with EGFR mutations suggests that synthetic lethal screens might be particularly useful for identifying proteins that contribute to resistance to inhibitors of Ras effectors.107 In contrast to advanced cancers, such as AML and MM, it is possible that “early-stage” hematologic disorders, such as JMML, will respond to therapies that exclusively target oncogenic Ras signaling networks.
Targeting aberrant signaling downstream of oncogenic Ras remains a daunting challenge. Our current understanding of the Ras effector pathways that are essential for cancer initiation and maintenance is incomplete, and it is likely that these dependencies vary in specific cell types. A related question is how “addicted” different cancers are to oncogenic Ras signaling. At one end of the spectrum, mutant RAS might be required during early stages of leukemogenesis but dispensible thereafter. Alternatively, advanced hematologic cancers, such as AML, might become ever more dependent on oncogenic Ras as they evolve. If the latter proves true, it will be important fully elucidate the feedback mechanisms that cancer cells deploy to restrain aberrant signaling and to characterize how these adaptations contribute to oncogene dependence. In addition to their inherent value as potential anticancer drugs, potent and selective inhibitors of Ras-regulated kinases are invaluable tools for addressing these questions through in vitro and in vivo studies.
Hematopoietic malignancies provide exceptional platforms for addressing mechanistic and translational questions because of established systems for culturing primary cells, robust mouse models, and the ability to serially sample diseased tissues from patients enrolled on clinical trials. Thus, rigorously interrogating how targeted anticancer agents modulate oncogenic Ras signaling and how this correlates with therapeutic response in hematologic malignancies has broad implications for reducing the major contribution of oncogenic RAS mutations to the worldwide burden of cancer.
Acknowledgments
The authors thrank the members of the laboratories of B.S.B. and K.M.S. for helpful discussions. Limitations on the number of references prevented us from citing some primary sources.
The work in our laboratories on RAS and NF1 mutations in hematologic cancers was supported by the Children's Tumor Foundation (Neurofibromatosis Preclinical Consortium award), the National Institutes of Health (grant R37 CA72614), the Leukemia & Lymphoma Society of America (Specialized Center of Research award), a St Baldrick's Foundation Scholar award (B.S.B.), and a Hyundai Hope on Wheels Fellowship (A.F.W.). K.M.S. is an American Cancer Society Research Professor.
National Institutes of Health
Authorship
Contribution: A.F.W., B.S.B., and K.M.S. wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Kevin M. Shannon, Helen Diller Family Cancer Research Building, University of California, San Francisco, 1450 3rd St, Room 240, San Francisco, CA 94158-9001; e-mail: shannonk@peds.ucsf.edu.