Abstract
The exact mechanisms underlying the role of oxidative stress in the pathogenesis and the prothrombotic or proinflammatory status of antiphospholipid syndrome (APS) remain unknown. Here, we investigate the role of oxidative stress and mitochondrial dysfunction in the proatherothrombotic status of APS patients induced by IgG-antiphospholipid antibodies and the beneficial effects of supplementing cells with coenzyme Q10 (CoQ10). A significant increase in relevant prothrombotic and inflammatory parameters in 43 APS patients was found compared with 38 healthy donors. Increased peroxide production, nuclear abundance of Nrf2, antioxidant enzymatic activity, decreased intracellular glutathione, and altered mitochondrial membrane potential were found in monocytes and neutrophils from APS patients. Accelerated atherosclerosis in APS patients was found associated with their inflammatory or oxidative status. CoQ10 preincubation of healthy monocytes before IgG-antiphospholipid antibody treatment decreased oxidative stress, the percentage of cells with altered mitochondrial membrane potential, and the induced expression of tissue factor, VEGF, and Flt1. In addition, CoQ10 significantly improved the ultrastructural preservation of mitochondria and prevented IgG-APS–induced fission mediated by Drp-1 and Fis-1 proteins. In conclusion, the oxidative perturbation in APS patient leukocytes, which is directly related to an inflammatory and pro-atherothrombotic status, relies on alterations in mitochondrial dynamics and metabolism that may be prevented, reverted, or both by treatment with CoQ10.
Introduction
Antiphospholipid syndrome (APS) is a clinical disorder characterized by thrombosis and pregnancy morbidity associated with the persistent presence of antiphospholipid (aPL) antibodies, including anti–β2-glycoprotein-I (anti-β2GPI), lupus anticoagulant, or both and complement factors.1 Procoagulant cell activation, accompanied with tissue factor (TF) expression, and TF pathway up-regulation are key events considered explaining the pathophysiology of thrombosis in patients with APS.2,3 In addition, it has been shown that TF signaling activities in APS are mainly mediated by protease-activated receptors (PARs).4,5 Accordingly, PAR1- and PAR2-induced signaling is directly involved in the constitutive mitogen-activated protein kinase (MAPK) activation6 and the increased expression found in patients with aPL antibodies of the proinflammatory cytokine vascular endothelial growth factor (VEGF) and its receptor Flt1.7 Similar results have been reported in endothelial cells (ECs),8 platelets, and monocytic cell lines and in in vivo models of aPL-induced thrombogenicity.9–11
Notably, aPL antibodies also trigger an inflammatory cascade, and they have been associated with atherosclerosis as well as cerebrovascular and peripheral arterial diseases.12,13 Moreover, aPL antibodies may cross-react with oxidized low-density lipoproteins (ox-LDLs), and both aPL and anti–ox-LDL antibodies have been implicated in the pathogenesis of atherosclerosis associated with systemic lupus erythematosus (SLE) and APS. It has been shown that aPL antibodies, in particular anti-β2GPI antibodies, can accelerate the influx of ox-LDLs into macrophages.14 Other autoantibodies, such as anti–high-density lipoproteins (HDLs) and antiapolipoprotein A-I, also have been detected in APS. In addition, macrophages and ECs bind to β2GPI during the atherosclerotic process. In this regard, anticardiolipin (aCL) antibodies can induce monocyte adherence to ECs, which is mediated by adhesion molecules such as ICAM-1, VCAM-1, and E-selectin. Thus, aCL antibodies might promote atherosclerosis by attracting monocytes into the vessel wall. Moreover, a correlation between serum levels of aCL and anti-β2GPI antibodies and the incidence and severity of acute coronary syndrome, myocardial infarction, and stroke have been demonstrated previously.15,16 Early endothelial dysfunction17 and increased carotid intima-media thickness also have been observed in APS.18
Various studies have evidenced that oxidative stress is directly involved in the pathophysiology of both APS and SLE. Mitochondrial dysfunction, accompanied with ATP depletion, oxidative stress, abnormal activation, and death signal processing in lupus T cells have been demonstrated previously.19 In the setting of APS, aCL antibodies seem to play an important role in the oxidative status by inducing nitric oxide (NO) and superoxide production, resulting in enhanced levels of plasma peroxynitrite, a powerful pro-oxidant substance.20 Titers of aCL antibodies have been found positively correlated to plasma levels of F2-isoprostanes, sensitive markers of in vivo lipid peroxidation, indicating enhanced oxidative stress in APS.21,22 Functional and structural arterial abnormalities were associated with lower activity of paraoxonase, an antioxidant enzyme linked to HDLs that prevents LDL oxidation. Moreover, in patients with aPL antibodies, HDL reduced NO bioavailability and showed impaired anti-inflammatory and antioxidant properties.23
Thus, aCL antibody production has been associated with vascular disease, plasma oxidation, and endothelial activation. However, few studies have critically analyzed the precise pathogenic role of the aCL-induced oxidative stress; in most cases, analysis has been just at plasmatic level.23–25. In addition, oxidative stress markers in circulating leucocytes from APS patients have not been investigated, and the source of reactive oxygen species (ROS) in those cells and the cellular and molecular mechanisms regulating those processes remain elusive. Mitochondrial machinery is particularly susceptible to oxidative damage, and the mitochondrial integrity of circulating peripheral lymphocytes in APS, which perpetuate chronic inflammation and prothrombotic status, has not been fully investigated to date.
Coenzyme Q10 (CoQ10; ubiquinone) is a vital component of the mitochondrial respiratory chain, with a crucial role in ATP production as the coenzyme for the mitochondrial complexes I, II, and III.26 CoQ10 provides membrane-stabilizing properties and also acts as an antioxidant with cell-protective effects, including inhibition of LDL oxidation and thus the progression of atherosclerosis. Furthermore, CoQ10 decreases the production of proinflammatory cytokines, as well as blood viscosity, demonstrated to be helpful in patients with heart failure and coronary artery disease. Different studies have highlighted the beneficial effects of CoQ10 supplementation in a variety of clinical conditions, with emphasis on cardiovascular disease.27,28 Yet, CoQ10 beneficial effects on APS patients with high risk of atherothrombosis have not been evaluated.
We undertook this study to investigate the role of oxidative stress and mitochondrial dysfunction in the aPL-induced proatherothrombotic status of APS patients and to test the effects of CoQ10 supplementation of cells.
Methods
Patients
Forty-three patients fulfilling the classification criteria for APS, 25 with previous thrombotic events and 19 with pregnancy morbidity, and 38 healthy donors were included in the study (during a period of 24 months) after ethics committee approval was obtained at the Reina Sofia Hospital in Cordoba, Spain. All patients provided written informed consent in accordance with the Declaration of Helsinki. Patients were studied at least 9 months after their latest thrombotic event or pregnancy loss. We excluded all APS patients who had evidence of an underlying systemic rheumatic disease or other medical conditions or who were using drugs for any other conditions. None of the healthy controls had a history of autoimmune disease, bleeding disorders, thrombosis, or pregnancy loss.
All patients were tested for the presence of aCL and lupus anticoagulant antibodies: IgG-and IgM-aCL antibodies were determined by ELISA using a commercial kit (Inova Diagnostics). Results were expressed in standard IgG- or IgM-aCL units (IgG phospholipid units GPL or IgM phospholipid units, respectively). Lupus anticoagulant was detected according to the guidelines recommended by the Subcommittee for Standardisation of the International Society on Thrombosis and Hemostasis.29 The characteristics of the patients and the controls are shown in Table 1.
Clinical and laboratory parameters of the APS patients and the controls
| . | APS patients . | Healthy donors . | P . |
|---|---|---|---|
| Clinical parameters* | |||
| Females/males | 34/9 | 32/6 | |
| Age, y | 48.43 ± 11.68 | 42.88 ± 9.50 | n.s. |
| Arterial thrombosis (%) | 18 (42) | 0 | |
| Venous thrombosis (%) | 7 (16) | 0 | |
| Recurrences (%) | 8 (19) | 0 | |
| Pregnancy morbidity (%) | 19 (44) | 0 | |
| Obesity (%) | 10 (23) | 2 (5) | |
| Increased CIMT (%) | 13 (30) | 2 (5) | |
| Lupus anticoagulant positivity (%) | 29 (67) | 0 | |
| aCL IgG, GPL | 48.64 ± 97.57 | 1.96 ± 2.70 | .007 |
| aCL IgM, MPL | 29.69 ± 53.10 | 10.38 ± 7.58 | .038 |
| Anti-β2GPI, SGU | 41.3 ± 103.0 | 4.07 ± 9.29 | .022 |
| Antiplatelet, ASA/clopidogel (%) | 17 (39) | 0 | |
| Anticoagulant, warfarin/acenocoumarol (%) | 16 (37) | 0 | |
| Hydroxychloroquine (%) | 3(7) | 0 | |
| Laboratory parameters* | |||
| Total cholesterol, mg/dL | 195.88 ± 38.07 | 208.31 ± 31.12 | n.s. |
| Cholesterol HDL, mg/dL | 52.68 ± 13.95 | 63.62 ± 15.45 | n.s. |
| Cholesterol LDL, mg/dL | 118.18 ± 33.93 | 126.45 ± 29.66 | n.s. |
| Triglycerides, mg/dL | 120.61 ± 67.99 | 89.07 ± 57.93 | n.s. |
| C reactive protein, mg/dL | 5.80 ± 10.80 | 1.84 ± 4.81 | n.s. |
| Apolipoprotein A, g/L | 140.19 ± 19.12 | 159.26 ± 28.12 | .019 |
| Apolipoprotein B, g/L | 89.57 ± 19.13 | 89.57 ± 21.64 | n.s. |
| . | APS patients . | Healthy donors . | P . |
|---|---|---|---|
| Clinical parameters* | |||
| Females/males | 34/9 | 32/6 | |
| Age, y | 48.43 ± 11.68 | 42.88 ± 9.50 | n.s. |
| Arterial thrombosis (%) | 18 (42) | 0 | |
| Venous thrombosis (%) | 7 (16) | 0 | |
| Recurrences (%) | 8 (19) | 0 | |
| Pregnancy morbidity (%) | 19 (44) | 0 | |
| Obesity (%) | 10 (23) | 2 (5) | |
| Increased CIMT (%) | 13 (30) | 2 (5) | |
| Lupus anticoagulant positivity (%) | 29 (67) | 0 | |
| aCL IgG, GPL | 48.64 ± 97.57 | 1.96 ± 2.70 | .007 |
| aCL IgM, MPL | 29.69 ± 53.10 | 10.38 ± 7.58 | .038 |
| Anti-β2GPI, SGU | 41.3 ± 103.0 | 4.07 ± 9.29 | .022 |
| Antiplatelet, ASA/clopidogel (%) | 17 (39) | 0 | |
| Anticoagulant, warfarin/acenocoumarol (%) | 16 (37) | 0 | |
| Hydroxychloroquine (%) | 3(7) | 0 | |
| Laboratory parameters* | |||
| Total cholesterol, mg/dL | 195.88 ± 38.07 | 208.31 ± 31.12 | n.s. |
| Cholesterol HDL, mg/dL | 52.68 ± 13.95 | 63.62 ± 15.45 | n.s. |
| Cholesterol LDL, mg/dL | 118.18 ± 33.93 | 126.45 ± 29.66 | n.s. |
| Triglycerides, mg/dL | 120.61 ± 67.99 | 89.07 ± 57.93 | n.s. |
| C reactive protein, mg/dL | 5.80 ± 10.80 | 1.84 ± 4.81 | n.s. |
| Apolipoprotein A, g/L | 140.19 ± 19.12 | 159.26 ± 28.12 | .019 |
| Apolipoprotein B, g/L | 89.57 ± 19.13 | 89.57 ± 21.64 | n.s. |
GPL indicates IgG phospholipid units; MPL, IgM phospholipid units; SGU, standard IgG units; and n.s., not significant.
Except where otherwise indicated, values are the number of subjects and mean ± SD.
Blood samples
The collection of peripheral venous blood samples for obtaining plasma and serum and for the preparation of purified monocytes (nonmonocytes depleting kit; Miltenyi Biotech) and lymphocytes and neutrophils (dextran sedimentation) was performed as described previously3,5,7 (for details see supplemental Methods, available on the Blood Web site; see the Supplemental Materials link at the top of the online article).
Flow cytometry analysis
Flow cytometric analysis was performed in white blood cells (WBCs) as described previously,3 using an FACScan cytometer (BD Biosciences) and monoclonal anti-human TF antibodies (clone TF9-6B4, FITC-conjugated; American Diagnostica), PAR2- and Flt1 FITC-conjugated (Santa Cruz Biotechnology), or to human CD14 PE-conjugated (Caltag).
FlowCytomix
CD40L, IFN-α, IFN-γ, interleukin (IL)–6, IL-8, IL-10, monocyte chemotactic protein (MCP)–1, macrophage inflammatory protein (MIP)–1α, tissue plasminogen activator (tPA), VEGF-A, and soluble platelet-selectin levels were quantified in sera using a cytofluorimetry-based ELISA system (FlowCytomix; Bender Medsystem). Two-color cytometric analysis was performed using a FACSCalibur cytometer (BD Biosciences). Data were obtained and analyzed using the FlowCytomix Pro Version 2.2.1 software.
Confocal fluorescent microscopy and image analyses
The fluorescent probes dichlorofluorescein diacetate (DCF-DA) and Rhodamine-123 were used to monitor the intracellular generation of ROS and the alterations in the mitochondrial membrane potential (Δψm) of monocytes treated in vitro with purified aCL antibodies. After a 30-minute incubation with DCF-DA (20.5μM) and Rhodamine-123 (5μM), intracellular ROS and Δψm were monitored using confocal fluorescence microscopy (LSM 5 Exciter; Carl Zeiss). To analyze the mitochondrial dynamics alterations and to follow the changes in the architecture of mitochondria as a consequence of APS-IgG treatment, cells were simultaneously incubated with MitoTracker (Invitrogen). For morphologic analyses of mitochondria, acquired images were analyzed with ImageJ Version 1.43u software (National Institutes of Health).
Determination of oxidative stress biomarkers in WBCs
Oxidative stress biomarkers were analyzed in WBCs (lymphocytes, monocytes, and neutrophils) using a dual-laser FACSCalibur flow cytometry system (Clontech). Test standardization and data acquisition analysis were performed using CellQuest Version 3.3 software (BD Biosciences). A forward and side scatter gate was used for the selection and analysis of the different cell subpopulations.
For the assessment of ROS generation, including superoxide anion and hydrogen peroxide, cells were incubated with 20.5μM DCF-DA at 37°C for 30 minutes in the dark. For the detection of intracellular glutathione (GSH), WBCs were incubated with 1μM 5-chloromethylfluorescein diacetate for 30 minutes in the dark. The cells were washed, resuspended in PBS, and then analyzed on a dual-laser FACSCalibur flow cytometry system. The MitoScreen assay kit (containing JC-1; BD Biosciences) was used (final concentration 2μM), to assess Δψm according to manufacturer's instructions.
Determination of plasma and cell oxidative stress biomarkers
The NO stable end products nitrite plus nitrate were measured in plasma using a commercial kit (Total Nitric Oxide Assay kit; Thermo Fisher Scientific). Serum total antioxidant capacity (TAC) was measured by quantitative colorimetric determination, using a TAC Assay kit (BioVision). Nitrotyrosine, as a marker of nitrative stress, was measured in monocytes and neutrophil extracts with a competitive enzyme immunoassay (Cell Biolabs). Mitochondrial superoxide dismutase (SOD) activity (manganese-SOD), catalase (CAT) activity, and glutathione peroxidase (GPx) activity were assayed in cell lysates using specific kits (Cayman Chemical) according to manufacturer's instructions.
B-mode ultrasound IMT measurements
All patients and controls underwent B-mode ultrasound imaging for carotid intima media thickness (CIMT) measurements. B-mode ultrasound imaging of the carotid arteries was performed as described previously18,30 using Toshiba equipment (Aplio platform) equipped with 7- to 10-MHz broadband linear array transducers. For further details, see supplemental Methods.
Plaque was defined as a focal structure that encroached into the arterial lumen of at least 50% of the surrounding intima media thickness (IMT) value or demonstrated a thickness more than 1.5 mm as measured from the media-adventicia interface to the intima-lumen interface.30
Western blotting and EMSAs
VEGF, Flt1, inducible NO synthase, IκBα, Nrf2, actin, TFIIB, phospho-p38 MAPK, p38 MAPK, FIS-1, OPA-1, DRP-1, MFN-1, and MFN-2 protein levels were determined by Western blotting,3 using specific antibodies (Santa Cruz Biotechnology). Nuclear extracts (20 μg) were tested in electrophoretic mobility shift assays (EMSAs) for nuclear factor-κB (NF-κB)–binding activity (consensus oligonucleotides, 5′-AGTTGAGGGGACTTTCCCAGGC-3′ and 3′-TCAACTCCCCTGAAAGGGTCCG-5′) using the digoxigenin EMSA kit (Roche Diagnostics) according to the manufacturer's recommendations.
Purification of IgG and in vitro exposure of normal monocytes to aPL antibodies
IgG from the pooled sera of 7 patients with APS (characterized by high titers of aCL antibodies, ie, > 120 IgG phospholipid units) and from the pooled sera of 7 healthy subjects (as controls) was purified by protein G-Sepharose high-affinity chromatography (MAbTrap kit; Amersham Biosciences) following the manufacturer's recommendations.
For in vitro studies, monocytes purified from healthy donors were cultured in serum-free RPMI 1640 containing 2mM l-glutamine, 100 U/mL penicillin, 100 mg/mL streptomycin, and 250 pg/mL Fungizone (BioWhittaker/MA Bioproducts), at 37°C in a humidified 5% carbon dioxide atmosphere. Purified normal monocytes (1.5 × 106 cells/mL) were incubated either with normal human serum (NHS)–IgG (500 μg/mL) or purified APS patient-IgG (500 μg/mL) for 6 hours at 37°C.
To test the effect of ROS inhibition on APS-IgG–induced monocyte activation, monocytes were pretreated for 1 hour at 37°C with antioxidants N-acetyl-l-cysteine (NAC) or vitamin C (Vit C) and then incubated for 6 hours with purified APS patient-IgG (APS-IgG) or NHS (NHS-IgG) in the presence of the drugs. Mitochondrial function was evaluated in vitro by preincubating purified monocytes with CoQ10, rotenone, or antimycin, followed by stimulation with APS-IgG and analysis of Δψm using the dyes JC-1 and TMRM (15nM).
Electron microscopy
Electron microscopy analysis of monocytes treated with APS-IgG in the presence or in the absence of CoQ10 was performed as described previously.31–33 For further details, see supplemental Methods.
Statistical analysis
All data are expressed as mean ± SEM. Statistical analyses were performed using the SSPS 15.0 package (SPSS). After normality and equality of variance tests, comparisons were made by paired Student t test or alternatively using a nonparametric test (Mann-Whitney rank sum test). Correlations were assessed by Pearson product-moment correlation and association studies were performed with χ2 test. The independent association between different variables in univariate analysis was determined by multivariate regression analysis using SPSS Version 15.0 for Windows statistical software. Differences were considered significant at P < .05.
Results
Clinical and analytical characteristics of APS patients
No significant difference between APS patients and controls was found in terms of traditional risk factors for atherosclerosis and inflammation (obesity, total cholesterol, HDL cholesterol, LDL cholesterol, or triglycerides), except for apolipoprotein A-I levels, which were found significantly altered in APS patients (Table 1).
CIMT was significantly greater in patients with APS versus controls (0.95 ± 0.23 vs 0.67 ± 0.20 mm; P < .05).
Prothrombotic and Inflammatory parameters are dysregulated in APS patients
As reported in previous studies,2,5,7 monocytes of APS patients showed increased cell surface expression of TF, PAR2, and Flt1 compared with the control group (Table 2). APS patients also displayed increased plasma levels of VEGF, IL-8, MCP-1, MIP-1α, and tPA.
Parameters of thrombosis, inflammation, and oxidative stress in the APS patients and the controls
| . | APS patients (n = 43) . | Healthy donors (n = 38) . | P . |
|---|---|---|---|
| Prothrombotic and proinflammatory parameters | |||
| TF, % | |||
| Monocytes | 47.13 ± 23.08 | 28.39 ± 22.20 | .03 |
| Neutrophils | 20.99 ± 19.14 | 12.28 ± 11.14 | n.s. |
| PAR2, % | |||
| Monocytes | 10.55 ± 8.9 | 5.90 ± 3.60 | .024 |
| Neutrophils | 2.25 ± 1.27 | 2.13 ± 1.71 | n.s. |
| VEGF-R1, % | |||
| Monocytes | 70.84 ± 24.62 | 50.06 ± 31.81 | .011 |
| Neutrophils | 61.47 ± 51.39 | 34.17 ± 27.61 | n.s. |
| VEGF-A, pg/mL | 605.26 ± 500.73 | 347.29 ± 221.33 | .047 |
| sCD40L, ng/mL | 16.32 ± 22.16 | 22.85 ± 19.30 | n.s. |
| IFN-α, pg/mL | 87.60 ± 145.71 | 168.47 ± 258.58 | n.s. |
| IFN-γ, pg/mL | 1.89 ± 6.29 | 5.46 ± 11.50 | n.s. |
| IL-6, pg/mL | 0.03 ± 0.10 | 0.11 ± 0.15 | n.s. |
| IL-8, pg/mL | 25.20 ± 52.70 | 4.10 ± 13.40 | .030 |
| IL-10, pg/mL | 22.30 ± 61.20 | 35.69 ± 79.49 | n.s. |
| MCP-1, pg/mL | 627.10 ± 251.60 | 486.79 ± 157.14 | .016 |
| MIP1-α, pg/mL | 455.80 ± 509.20 | 192.58 ± 273.86 | .016 |
| soluble P-selectin, ng/mL | 193.19 ± 75.28 | 183.52 ± 69.60 | n.s. |
| tPA, ng/mL | 2.54 ± 1.40 | 1.90 ± 0.82 | .049 |
| Oxidative status in plasma and monocytes | |||
| TAC, plasma; mM Trolox equivalent | 103.57 ± 44.9 | 147.12 ± 54.78 | .005 |
| NO, plasma, μM | 15.76 ± 7.97 | 21.75 ± 12.09 | .035 |
| Nitrotyrosine, μM | 729.10 ± 695.76 | 196.75 ± 201.41 | .010 |
| Manganese-SOD, U/min/mL/μg protein | 0.24 ± 0.19 | 0.11 ± 0.11 | .019 |
| Catalase, nmoL/min/mL/μg protein | 122.11 ± 90.91 | 211.69 ± 111.81 | .025 |
| GPx, nmoL/min/mL/μg protein | 1.19 ± 0.60 | 2.33 ± 0.97 | .009 |
| . | APS patients (n = 43) . | Healthy donors (n = 38) . | P . |
|---|---|---|---|
| Prothrombotic and proinflammatory parameters | |||
| TF, % | |||
| Monocytes | 47.13 ± 23.08 | 28.39 ± 22.20 | .03 |
| Neutrophils | 20.99 ± 19.14 | 12.28 ± 11.14 | n.s. |
| PAR2, % | |||
| Monocytes | 10.55 ± 8.9 | 5.90 ± 3.60 | .024 |
| Neutrophils | 2.25 ± 1.27 | 2.13 ± 1.71 | n.s. |
| VEGF-R1, % | |||
| Monocytes | 70.84 ± 24.62 | 50.06 ± 31.81 | .011 |
| Neutrophils | 61.47 ± 51.39 | 34.17 ± 27.61 | n.s. |
| VEGF-A, pg/mL | 605.26 ± 500.73 | 347.29 ± 221.33 | .047 |
| sCD40L, ng/mL | 16.32 ± 22.16 | 22.85 ± 19.30 | n.s. |
| IFN-α, pg/mL | 87.60 ± 145.71 | 168.47 ± 258.58 | n.s. |
| IFN-γ, pg/mL | 1.89 ± 6.29 | 5.46 ± 11.50 | n.s. |
| IL-6, pg/mL | 0.03 ± 0.10 | 0.11 ± 0.15 | n.s. |
| IL-8, pg/mL | 25.20 ± 52.70 | 4.10 ± 13.40 | .030 |
| IL-10, pg/mL | 22.30 ± 61.20 | 35.69 ± 79.49 | n.s. |
| MCP-1, pg/mL | 627.10 ± 251.60 | 486.79 ± 157.14 | .016 |
| MIP1-α, pg/mL | 455.80 ± 509.20 | 192.58 ± 273.86 | .016 |
| soluble P-selectin, ng/mL | 193.19 ± 75.28 | 183.52 ± 69.60 | n.s. |
| tPA, ng/mL | 2.54 ± 1.40 | 1.90 ± 0.82 | .049 |
| Oxidative status in plasma and monocytes | |||
| TAC, plasma; mM Trolox equivalent | 103.57 ± 44.9 | 147.12 ± 54.78 | .005 |
| NO, plasma, μM | 15.76 ± 7.97 | 21.75 ± 12.09 | .035 |
| Nitrotyrosine, μM | 729.10 ± 695.76 | 196.75 ± 201.41 | .010 |
| Manganese-SOD, U/min/mL/μg protein | 0.24 ± 0.19 | 0.11 ± 0.11 | .019 |
| Catalase, nmoL/min/mL/μg protein | 122.11 ± 90.91 | 211.69 ± 111.81 | .025 |
| GPx, nmoL/min/mL/μg protein | 1.19 ± 0.60 | 2.33 ± 0.97 | .009 |
Values are mean ± SD.
APS patients display an oxidative status
Peroxide production was notably increased in monocytes and neutrophils of APS patients (Figure 1A), whereas intracellular reduced GSH was significantly decreased in both cell types (Figure 1B). The percentage of cells with altered Δψm was found significantly increased in monocytes and neutrophils from APS patients compared with cells isolated from healthy donors (Figure 1C).
Cellular oxidative stress in APS patients. (A) Peroxide production in neutrophils, monocytes, and lymphocytes of APS patients, determined by addition of the fluorescent probe DCF-DA to the isolated cells and flow cytometry analysis. Representative histograms are shown in parallel with bar graphs showing the mean ± SD of median fluorescence intensity (MFI) of all the patients (dotted bars) and healthy donors (empty bars) included in the study. (B) Intracellular glutathione levels of neutrophils, monocytes, and lymphocytes of APS patients and healthy donors, determined by addition of the fluorescent probe CMF-DA and measurement as described for panel A. Representative histograms are shown in parallel with bar graphs showing the mean ± SD of MFI. (C) Proportion of circulating neutrophils, monocytes, and lymphocytes with depolarized mitochondria, determined with the JC-1 MitoScreen assay. Representative dot plots of isolated cells from patients and controls are shown together with the bar graph showing the mean ± SD of all the patients and the controls included in the study (*P < .05 vs healthy donors). (D) Nuclear Nrf2 protein abundance in monocytes of representative APS patients and healthy donors. The nuclear abundance of the transcription factor TFIIB was used as a loading control.
Cellular oxidative stress in APS patients. (A) Peroxide production in neutrophils, monocytes, and lymphocytes of APS patients, determined by addition of the fluorescent probe DCF-DA to the isolated cells and flow cytometry analysis. Representative histograms are shown in parallel with bar graphs showing the mean ± SD of median fluorescence intensity (MFI) of all the patients (dotted bars) and healthy donors (empty bars) included in the study. (B) Intracellular glutathione levels of neutrophils, monocytes, and lymphocytes of APS patients and healthy donors, determined by addition of the fluorescent probe CMF-DA and measurement as described for panel A. Representative histograms are shown in parallel with bar graphs showing the mean ± SD of MFI. (C) Proportion of circulating neutrophils, monocytes, and lymphocytes with depolarized mitochondria, determined with the JC-1 MitoScreen assay. Representative dot plots of isolated cells from patients and controls are shown together with the bar graph showing the mean ± SD of all the patients and the controls included in the study (*P < .05 vs healthy donors). (D) Nuclear Nrf2 protein abundance in monocytes of representative APS patients and healthy donors. The nuclear abundance of the transcription factor TFIIB was used as a loading control.
Given the well-characterized antioxidant actions of Nrf2 as a master regulator of antioxidant gene expression, we further evaluated the nuclear Nrf2 protein abundance by Western immunoblotting. We found a significant decrease in nuclear Nrf2 protein abundance in monocytes from APS patients in relation to the control group (Figure 1D).
At the plasma level, a significant reduction of TAC in plasma from APS patients was found compared with healthy donors (P = .001; Table 2) and might indicate a reduced capability to counteract ROS and resist oxidative damage. Plasma NO levels were significantly lower in APS patients versus healthy donors (P = .034), probably as a consequence of its consumption after reacting with reactive substances such as superoxide, and the consequent formation of peroxynitrites. In support for that hypothesis, levels of protein tyrosine nitration were significantly increased in monocytes from APS patients compared with healthy donors (P = .026; Table 2).
A prominent increase in the activity of monocyte mitochondrial SOD (P = .002) was found in APS patients compared with healthy donors. Yet, the activities of CAT and GPx were notably reduced (P = .044 and P = .007, respectively; Table 2).
Correlation and association studies
Levels of aCL antibodies of IgG isotype positively correlated with the percentage of cells showing depolarized mitochondria (r = 0.741; P = .003; Figure 2A). Peroxide levels from monocytes and monocyte cell surface TF expression levels showed a significant positive correlation (r = 0.773; P = .029, Figure 2B). A further positive correlation was demonstrated between peroxide levels in monocytes and neutrophils and plasmatic tPA (r = 0.839; P = .049 and r = 0.371; P = .024, respectively; Figure 2C). We also found a negative correlation between plasma VEGF-A levels and TAC (r = -0.414; P = .015; Figure 2D). Plasma levels of IL-8 and tPA were each other correlated (r = 0.345; P = .042), just as plasma levels of IL-8 and VEGF (r = 0.490; P = .028), plasma levels of VEGF and MCP-1 (r = 0.652; P = .002), and monocyte cell surface TF and PAR2 expression levels (r = 0.502; P = .029).
Correlation and association studies among markers of oxidative stress and different markers related to autoimmunity, inflammation, and thrombosis in APS (statistical test: Pearson correlation analysis). (A) Positive correlation between levels of anticardiolipin antibodies of IgG isotype and the percentage of cells with impaired Δψm (depolarized mitochondria). (B) Positive correlation between peroxide levels in monocytes and cell surface expression of TF. (C) Positive correlation between peroxide levels in monocytes and plasma levels of tPA. (D) Negative correlation between plasma VEGF-A levels and TAC. (E) Relationship between the occurrence of thrombotic events and the levels of aCL antibodies of IgG isotype. Asterisk (*) indicates significant differences versus patients without thrombosis (P < .05). (F) Relationship between the occurrence of thrombotic events and the percentage of cells with depolarized mitochondria. (G) Relationship between the occurrence of thrombotic events and the levels of TAC in plasma.
Correlation and association studies among markers of oxidative stress and different markers related to autoimmunity, inflammation, and thrombosis in APS (statistical test: Pearson correlation analysis). (A) Positive correlation between levels of anticardiolipin antibodies of IgG isotype and the percentage of cells with impaired Δψm (depolarized mitochondria). (B) Positive correlation between peroxide levels in monocytes and cell surface expression of TF. (C) Positive correlation between peroxide levels in monocytes and plasma levels of tPA. (D) Negative correlation between plasma VEGF-A levels and TAC. (E) Relationship between the occurrence of thrombotic events and the levels of aCL antibodies of IgG isotype. Asterisk (*) indicates significant differences versus patients without thrombosis (P < .05). (F) Relationship between the occurrence of thrombotic events and the percentage of cells with depolarized mitochondria. (G) Relationship between the occurrence of thrombotic events and the levels of TAC in plasma.
Association studies showed that the occurrence of thrombotic events in APS was associated with previously reported factors (ie, aCL antibodies, TF; Figure 2E) as well as with oxidative stress markers such as decreased Δψm and TAC (Figure 2F-G). TF, PAR2, and Flt1 cell surface expression in monocytes of APS patients was mostly associated with the occurrence of arterial thrombosis. Yet, the alterations found in different oxidative stress parameters in monocytes and neutrophils, including peroxide production, Δψm, and enzymatic antioxidant activity, were found related to the occurrence of both types of thrombotic events (arterial or venous) and also to the occurrence of pregnancy loss (all P < .05).
In addition, among APS patients, those who had previously experienced a thrombotic event (particularly those with arterial occlusions) had greater CIMT compared with those without prior thrombosis (P = .023). In contrast, a significant association was noted between the increased CIMT and the levels of aCL-IgG (P = .024), the percentage of cells with altered Δψm (P = .046), the cell surface TF expression levels on monocytes (P = .049), and the age of APS patients (P = .041).
Multivariate analysis of all the measured parameters and titers of aCL and anti-β2GPI antibodies demonstrated that IgG aCL titers independently predicted increased CIMT (standardized β coefficient = 0.590; P = .001), thus supporting an atherogenic role for IgG-aCL antibodies in APS patients. Moreover, titers of IgG-aCL antibodies independently predicted the mitochondrial damage (measured as percentage of cells with altered Δψm) observed in patients monocytes (beta = 0.365; P = .011).
aCL antibodies promote an oxidative status in APS monocytes
A 2-hour stimulation of monocytes with IgG-APS induced a marked increase in the levels of peroxides (supplemental Figure 1A) that remained significantly augmented for 12 hours. No such increase was observed with IgG-NHS or with nonspecific human IgG obtained from a commercial source (data not shown). In contrast, we found a significant decrease in the levels of intracellular reduced GSH, which lasted 12 hours after treatment with IgG-APS (supplemental Figure 1B). In parallel, there was a steady decrease in nuclear Nrf2 protein abundance that remained for 24 hours (supplemental Figure 1C).
The percentage of cells with depolarized mitochondria was significantly increased just after 2 hours of IgG-APS treatment (supplemental Figures 1D and 2), suggesting the involvement of the mitochondrial electron transport chain in the IgG-APS–mediated ROS generation.
However, in contrast with our in vivo studies, we observed a significant increase in NO production in the supernatant of monocyte cell cultures, as soon as 2 hours after stimulation with IgG-APS was started, and lasting until 12 hours. Accordingly, the expression of the inducible NO synthase was found significantly increased with the same time-response pattern (supplemental Figure 1E-F).
Preincubation of monocytes for 1 hours with the antioxidants NAC or Vit C significantly reduced the IgG-APS–induced peroxide production, as monitored by flow cytometry and fluorescent micrographs of ROS production (supplemental Figure 3). The use of antioxidants also restored the levels of reduced GSH, NO production, and inducible NO synthase expression (supplemental Figure 4). However, NAC or Vit C pretreatments failed to prevent the mitochondrial depolarization induced by IgG-APS (data not shown), indicating that increased ROS production occurs downstream of mitochondrial damage. Furthermore, no changes in the APS-IgG–induced increase in ROS production was found after cotreatment with 500μM Nω-nitro-l-arginine methyl ester up to 24 hours (data not shown).
A significant reduction in the IgG-APS–induced expression of TF, VEGF, and Flt1 after cotreatment with NAC and Vit C was found. In parallel, the activities of p38 MAPK and NF-κB were down-regulated by the effect of those ROS inhibitors (supplemental Figure 5).
Mitochondrial dysfunction is directly involved in the prothrombotic status of APS
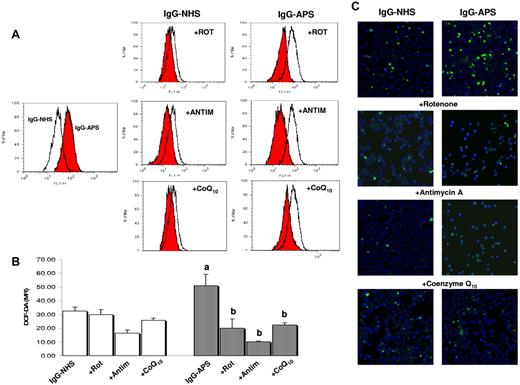
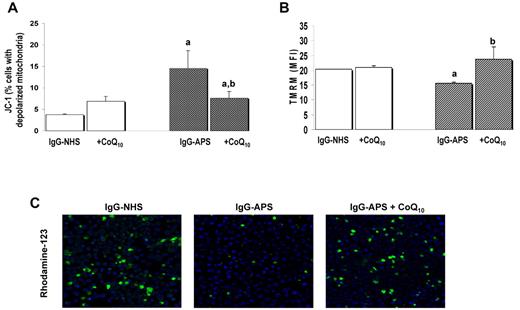
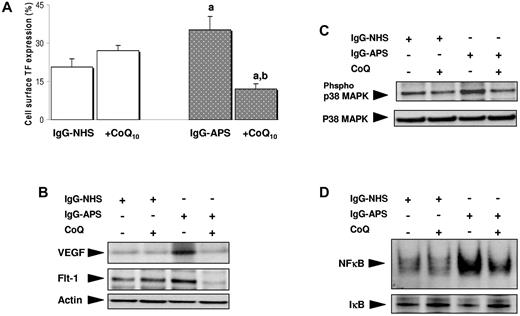
A significant inhibition of ROS generation induced by IgG-APS was observed after pretreatment of monocytes with rotenone and antimycin A, as well as with CoQ10 (Figure 3), strongly supporting the participation of the mitochondrial electron transport chain in the oxidative perturbation induced by these autoantibodies. In addition, CoQ10 significantly diminished the percentage of cells with altered Δψm, and reversed the depolarization of the mitochondria resulting from IgG-APS treatment, as monitored by flow cytometry and fluorescence micrography (Figure 4). Notably, preincubation of monocytes with CoQ10, followed by treatment with IgG-APS, promoted a significant reduction in the increased expression of the thrombotic and proinflammatory markers TF, VEGF, and Flt1, along with the intracellular signaling pathways regulating their expression (Figure 5).
Effects of mitochondrial inhibitors and the mitochondrial cofactor CoQ10 on IgG-APS–induced generation of peroxides. (A) Cells were preincubated with rotenone (Rot) or antimicin A (Antim) for 1 hour, or with CoQ10 for 24 hours, washed, and then stimulated with IgG-APS or IgG-NHS in the presence of the drugs. This figure shows representative flow cytometry histograms of DCF-DA fluorescence for each group of treatment. (B) Bar graph represents the mean of MFI ± SEM of 4 independent experiments. Significant differences (at P < .05) versus monocytes treated with IgG-NHS– (a) and versus IgG-APS–treated cells (b). (C) Representative fluorescent photomicrographs of ROS production by monocytes stimulated as described in panel A. Images were acquired with an LSM 5 Exciter confocal microscope (Carl Zeiss), driven by ZEN 2008 software by exciting at 488 nm to detect the DCF-DA fluorescence, and at 405 nm for 4,6-diamidino-2-phenylindole fluorescence. Samples were viewed with a EC Plan-Neofluar 20×/0.50 numerical aperture objective.
Effects of mitochondrial inhibitors and the mitochondrial cofactor CoQ10 on IgG-APS–induced generation of peroxides. (A) Cells were preincubated with rotenone (Rot) or antimicin A (Antim) for 1 hour, or with CoQ10 for 24 hours, washed, and then stimulated with IgG-APS or IgG-NHS in the presence of the drugs. This figure shows representative flow cytometry histograms of DCF-DA fluorescence for each group of treatment. (B) Bar graph represents the mean of MFI ± SEM of 4 independent experiments. Significant differences (at P < .05) versus monocytes treated with IgG-NHS– (a) and versus IgG-APS–treated cells (b). (C) Representative fluorescent photomicrographs of ROS production by monocytes stimulated as described in panel A. Images were acquired with an LSM 5 Exciter confocal microscope (Carl Zeiss), driven by ZEN 2008 software by exciting at 488 nm to detect the DCF-DA fluorescence, and at 405 nm for 4,6-diamidino-2-phenylindole fluorescence. Samples were viewed with a EC Plan-Neofluar 20×/0.50 numerical aperture objective.
Effect of treatments with CoQ10 on monocytes mitochondrial dysfunction promoted by IgG-APS. (A) Cells were preincubated with CoQ10 for 24 hours, washed, and then stimulated with IgG-APS or IgG-NHS in the presence of the drugs. Then, the proportion of monocytes with depolarized mitochondria was determined with the JC-1 MitoScreen assay. (B) Using the dye TMRM, the change in mitochondrial membrane potential was further monitored by flow cytometry. Values are means and SEM from 4 independent experiments. Significant differences (at P < .05) versus monocytes treated with IgG-NHS (a) and versus IgG-APS–treated cells (b). (C) Representative fluorescent photomicrographs of mitochondrial damage (magnification, ×20) after incubation of monocytes (treated as described in panels A and B) with the probe Rhodamine-123 that only stains cells in which Δψm is intact.
Effect of treatments with CoQ10 on monocytes mitochondrial dysfunction promoted by IgG-APS. (A) Cells were preincubated with CoQ10 for 24 hours, washed, and then stimulated with IgG-APS or IgG-NHS in the presence of the drugs. Then, the proportion of monocytes with depolarized mitochondria was determined with the JC-1 MitoScreen assay. (B) Using the dye TMRM, the change in mitochondrial membrane potential was further monitored by flow cytometry. Values are means and SEM from 4 independent experiments. Significant differences (at P < .05) versus monocytes treated with IgG-NHS (a) and versus IgG-APS–treated cells (b). (C) Representative fluorescent photomicrographs of mitochondrial damage (magnification, ×20) after incubation of monocytes (treated as described in panels A and B) with the probe Rhodamine-123 that only stains cells in which Δψm is intact.
Effects of CoQ10 on IgG-APS–induced expression of prothrombotic markers and intracellular pathways. (A) Cell surface TF expression in monocytes treated with IgG-APS or IgG-NHS in the presence or in the absence of CoQ10. Values are means and SEM from 4 independent experiments. (B-D) Representative electrophoretic mobility shift assay and Western blotting results from 4 separate experiments showing, respectively, VEGF and Flt1 expression, p38 MAPK activity, and NF-κB binding activity after the treatments indicated. Significant differences (at P < .05) versus monocytes treated with IgG-NHS (a) and versus IgG-APS–treated cells (b).
Effects of CoQ10 on IgG-APS–induced expression of prothrombotic markers and intracellular pathways. (A) Cell surface TF expression in monocytes treated with IgG-APS or IgG-NHS in the presence or in the absence of CoQ10. Values are means and SEM from 4 independent experiments. (B-D) Representative electrophoretic mobility shift assay and Western blotting results from 4 separate experiments showing, respectively, VEGF and Flt1 expression, p38 MAPK activity, and NF-κB binding activity after the treatments indicated. Significant differences (at P < .05) versus monocytes treated with IgG-NHS (a) and versus IgG-APS–treated cells (b).
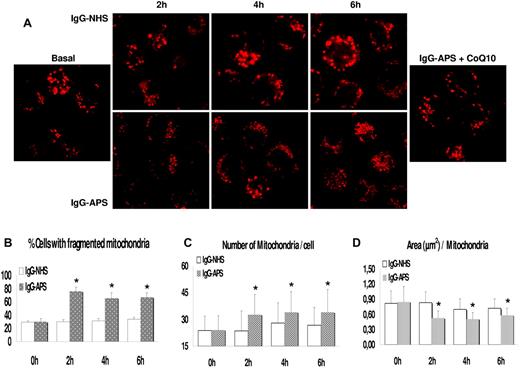
IgG-APS treatment promotes significant changes in mitochondrial ultrastructure and dynamics
Electron microscopy studies revealed that mitochondria of monocytes treated with IgG-APS showed a lower size and poorer ultrastructural preservation. Yet, as shown previously for other physiologic parameters evaluated, the pretreatment with CoQ10 promoted an increase in mitochondrial size and improved ultrastructural preservation (Figure 6A).
Changes in mitochondrial ultrastructure and dynamics in IgG-APS–treated cells and effects of CoQ10 pretreatment. Monocytes were treated with IgG-APS or IgG-NHS in the presence or in the absence of CoQ10 and then fixed with aldehydes, postfixed with osmium tetroxide, dehydrated, and embedded in epoxy resin. Thin sections were cut and stained with uranyl acetate and lead citrate for observation with an electron microscope. Alternatively, after cell treatments extracts were obtained as described under “Western blotting and EMSAs,” the proteins were separated by SDS-PAGE, transferred to nitrocellulose sheets, and stained with antibodies against proteins controlling mitochondrial fission (Drp1 and Fis1) and fusion (Mfn1, Mfn2, and Opa1). (A) Representative pictures of mitochondria from cells treated as indicated. Bar represents 1 μm. (B) Western blot detection of proteins controlling mitochondrial dynamics. Approximately 20 μg protein was loaded in each lane. This figure depicts a representative result from 3 independent determinations.
Changes in mitochondrial ultrastructure and dynamics in IgG-APS–treated cells and effects of CoQ10 pretreatment. Monocytes were treated with IgG-APS or IgG-NHS in the presence or in the absence of CoQ10 and then fixed with aldehydes, postfixed with osmium tetroxide, dehydrated, and embedded in epoxy resin. Thin sections were cut and stained with uranyl acetate and lead citrate for observation with an electron microscope. Alternatively, after cell treatments extracts were obtained as described under “Western blotting and EMSAs,” the proteins were separated by SDS-PAGE, transferred to nitrocellulose sheets, and stained with antibodies against proteins controlling mitochondrial fission (Drp1 and Fis1) and fusion (Mfn1, Mfn2, and Opa1). (A) Representative pictures of mitochondria from cells treated as indicated. Bar represents 1 μm. (B) Western blot detection of proteins controlling mitochondrial dynamics. Approximately 20 μg protein was loaded in each lane. This figure depicts a representative result from 3 independent determinations.
These results were confirmed in planimetric analysis of individual mitochondria, showing a reduction in their size after IgG-APS treatment but an increase in size when monocytes were preincubated with CoQ10 (supplemental Figure 6). Stereologic analysis showed that numerical density of mitochondria was significantly increased but that volume density was decreased in cells treated with IgG-APS and that these effects were abolished by CoQ10 (supplemental Figure 6). These observations are consistent with increased mitochondrial fission in IgG-APS–treated cells.
To support this interpretation, we studied how treatment with IgG-APS affected levels of proteins known to regulate mitochondrial dynamics of fission and fusion.34,35 As depicted in Figure 6B, treatment of monocytes with IgG-APS resulted in a strong increase in cellular levels of proteins stimulating mitochondrial fission, namely, Drp-1 and Fis-1. Interestingly, preincubation of cells with CoQ10 largely abolished this increase. In the proteins related with mitochondrial fusion, we observed that IgG-APS treatment resulted in either no change (Mfn-1) or slight increases (Mfn-2 and Opa-1). In the latter case, the effect of IgG-APS also was abolished by pretreatment of cells with CoQ10. Further studies were performed to analyze the mitochondrial dynamics in the setting of APS. As shown in Figure 7A, the IgG-APS–induced ROS production was accompanied by mitochondrial fragmentation, so that the number of cells containing fragmented mitochondria increased by a 50% in 2 hours of treatment (Figure 7B). We then analyzed mitochondrial morphologies by computer-assisted morphometric analyses that calculated the number of mitochondria per cells and their area. The increased number of mitochondria at each time point (Figure 7C) as well as the reduced average values of area of each mitochondria (Figure 7D) indicated fragmentation as a consequence of IgG-APS treatment. CoQ10 pretreatment prevented mitochondrial fission and restored the mitochondrial size found in IgG-NHS–treated monocytes.
IgG-APS–induced mitochondrial fragmentation. (A) Monocytes were plated in glass-bottomed Petri dishes in phenol red-free RPMI 1640, pretreated for 15 minutes with 50nM MitoTracker Red (excitation 581 nm/emission 644 nm), and then incubated for 6 hours with NHS-IgG or APS-IgG at 37°C in a humidified 5% carbon dioxide atmosphere. Cells were imaged in vivo at 1-hour intervals by confocal microscopy under exactly identical instrument settings for all stimuli. Samples were viewed with an EC Plan-Apochromal 63×/1.40 numerical aperture oil objective. Fragmented mitochondria were prevalent after 2 hours of APS-IgG treatment. CoQ10 pretreatment prevented mitochondrial fission and restored the mitochondrial size found in untreated or IgG-NHS–treated monocytes. (B) Percentage of cells with fragmented mitochondria at each time point is shown. (C-D) Analysis of mitochondrial morphologies by computer-assisted morphometric analyses that calculated the number of mitochondria per cell and their area. Asterisks (*) indicate significant differences (at P < .05) versus IgG-NHS–treated cells.
IgG-APS–induced mitochondrial fragmentation. (A) Monocytes were plated in glass-bottomed Petri dishes in phenol red-free RPMI 1640, pretreated for 15 minutes with 50nM MitoTracker Red (excitation 581 nm/emission 644 nm), and then incubated for 6 hours with NHS-IgG or APS-IgG at 37°C in a humidified 5% carbon dioxide atmosphere. Cells were imaged in vivo at 1-hour intervals by confocal microscopy under exactly identical instrument settings for all stimuli. Samples were viewed with an EC Plan-Apochromal 63×/1.40 numerical aperture oil objective. Fragmented mitochondria were prevalent after 2 hours of APS-IgG treatment. CoQ10 pretreatment prevented mitochondrial fission and restored the mitochondrial size found in untreated or IgG-NHS–treated monocytes. (B) Percentage of cells with fragmented mitochondria at each time point is shown. (C-D) Analysis of mitochondrial morphologies by computer-assisted morphometric analyses that calculated the number of mitochondria per cell and their area. Asterisks (*) indicate significant differences (at P < .05) versus IgG-NHS–treated cells.
Finally, to understand mechanistically the effect of IgG-APS on monocyte activation and mitochondrial damage, DyLight 488–labeled IgG-APS was added to monocytes. Neither intracellular fluorescence nor overlapping with the mitochondrial dye was detected, suggesting the occurrence of an indirect pathway of activation (supplemental Figure 7). Taken together, our structural and biochemical data are indicative that aCL antibodies affect mitochondrial dynamics toward an enhanced rate of fission.
Discussion
Our study for the first time provides evidence for a significant oxidative perturbation in APS patients leukocytes, directly related to an inflammatory and proatherothrombotic status. Moreover, those perturbations rely on the altered mitochondrial dynamics and metabolic processes, which generate free radical species.
Large in vitro and in vivo experimental evidence supports the pathogenic role of aPL in the setting of APS.36 Moreover, autoantibody titer has been suggested to be a key variable defining the eventual thrombotic risk for a given patient, so that the highest aPL levels are more predictive for the clinical manifestations.2 Accordingly, we found that patients with higher aPL-IgG titers showed a strong association with the development of thrombotic events and also with the increased IMT of the carotid arteries. The issue of early atherosclerosis development in APS patients has shown controversial data in past years. In our series, the presence of plaques in carotid arteries in a significant number of APS patients is in favor of the evidence of an accelerated atherosclerosis. Our results confirm 4 previous reports showing greater IMT in APS, related to the titer of aPL-IgG.37–39 Moreover, our data point to the existence of premature atherosclerosis as a clinical feature of thrombotic APS patients, so that in our series, 11 of 12 of the APS patients who presented increased IMT values had suffered at least 1 thrombotic event. In addition, our results agree with a recent study showing that premature atherosclerosis, as defined by IMT, occurs in thrombotic APS over 30 years.18 Premature atherosclerosis might be facilitated by the existence of an inflammatory status in APS, which seems not to be coordinated by “classic” cytokines such as TNF-α or IL-6 but by other known inflammatory mediators, including VEGF and tPA, as well as various chemokines (IL-8, MCP-1, or MIP-1α) whose main function is to recruit, eg, neutrophils, monocytes, B cells, and T helper cells to the sites of inflammation.40,41 Thrombus formation is a key event in the development of the intimal thickening considered to comprise the early stage of atherosclerosis plaque formation. Many studies have demonstrated that TF is present in atherosclerosis lesions and contributes to atherogenesis.42 TF mediates the responses that are critical for hemostasis and thrombosis, as well as inflammatory reactions. Thus TF, whose expression is also significantly increased in monocytes of APS patients, together with factors downstream of the coagulation cascade and the PAR2 activation system, would act as an additional multifactorial regulator of atherogenesis.42
A likely mechanism by which circulating WBCs may become damaged is through oxidative stress. There is substantial evidence showing oxidative damage to lipids and proteins in APS.20,23 The data from the present study showed an increased production of ROS by monocytes and neutrophils that disturbs the redox status that in turn may influence the expression of prothrombotic and proinflammatory molecules. That increase was accompanied by a significant reduction in the capacity of cells to counteract ROS, as demonstrated by the observed reduction in both the intracellular levels of GSH and the TAC of plasma in such patients. These results were in accordance with the recent report by Shah et al,40 demonstrating a significant reduction in plasma GSH in SLE. Thus, our study provides further evidence that, as reported previously,43 altered GSH concentrations may play an important role in pathologic conditions prevalently elicited and maintained by inflammatory and immunologic response mediated by oxidative stress reactions.
Nrf2 is a master regulator of cellular antioxidant defense, being a transcriptional activator of glutamate cysteine ligase catalytic subunit,44 and driving the GSH redox pair (GSH/oxidized GSH) toward a more reduced state through enhanced biosynthesis of GSH.45 In the present study, the levels of nuclear Nrf2 were repressed in monocytes from APS patients, in parallel with the reduced intracellular levels of GSH. These data might suggest a defect in the Keap1-Nrf2 pathway that prevents the nuclear translocation of Nrf2 in response to an increased oxidative status in the APS cells, thus hampering the necessary elevation in intracellular GSH under these conditions. Further experiments are needed to elucidate the role of Keap1-Nrf2 pathways in APS.
Reduced activities of CAT and GPx were found in monocytes and neutrophils of APS patients, perhaps because of the inactivation of the enzymes by overproduction of hydrogen peroxide (H2O2).46 These data further paralleled the results found in recent studies in plasma of SLE and rheumatoid arthritis patients.40,47 On the contrary, the manganese-SOD levels were found significantly increased. It seems possible that increased SOD dismutation of O2− into H2O2 may exceed the capability of GPx and CAT in that patients. Our data further agree with the results found by Zhang et al in plasma of SLE patients.48
In the present study, the overall oxidative status was mostly evaluated in WBCs, instead of plasma. Thus, our results confirm previous studies and show that oxidative stress is further promoted in circulating WBCs, including monocytes and neutrophils of APS patients. Moreover, the observed increase in the activity of the mitochondrial SOD isoform in those cells suggests the direct involvement of this organelle in the oxidative process. Accordingly, our data revealed that monocytes and neutrophils of APS patients had significant losses in Δψm, indicating that a large proportion of white blood cells contained mitochondria that have lost the capacity to function optimally. Mitochondrial perturbations were related to the autoimmune condition, as well as to the inflammatory and prothrombotic status of APS patients, as suggested by strong positive correlations with the titers of aCL antibodies of IgG isotype, as well as by the association found between the increased percentage of cells with depolarized mitochondria and the heightened occurrence of thrombotic events. Moreover, the presence of an increased CMIT in those patients was associated with that mitochondrial alteration.
The association found in vivo between the titers of aPL-IgG and various parameters related to oxidative stress, inflammation, and thrombosis in APS encouraged us to further analyze new molecular insights in the pathway triggering atherothrombosis in this autoimmune disease. Our in vitro studies indicated that the binding of IgG-APS to the monocytes elicited a redox-sensitive signaling pathway that controls the prothrombotic phenotype. The IgG-APS–induced ROS production exerted a prominent effect in the activation of a specific signaling cascade: the activation of p38 MAPK and the subsequent induction of NF-κB activation. The latter contributes to the aPL-mediated increase in TF expression,3 and the former also is involved in the induced expression of VEGF and Flt1.7 Inhibiting the rise in ROS levels by NAC and Vit C prevented both p38 MAPK and NF-κB activation, and protein up-regulation of TF, VEGF, and Flt1 in response to IgG-APS. Similar results were found in a study by Simoncini et al in endothelial cells.49 We could further demonstrate the involvement of the mitochondrial electron transport chain in the generation of peroxides induced by IgG-APS, as suggested by the significant inhibition by rotenone, antimycin A, and the mitochondrial cofactor CoQ10.
Several studies have detached the beneficial effects of CoQ10 supplementation on cardiovascular disease (reviewed in Littarru and Tiano27 ). The rationale for the use of CoQ10 as a therapeutic agent is based on its fundamental role in mitochondrial function. Our results indicated that CoQ10 not only improves the ultrastructural preservation of mitochondria and increases mitochondrial size but also prevents the IgG-APS–induced mitochondrial fission. Recent studies suggest that changes in mitochondrial morphology and function may affect a variety of aspects of cardiovascular biology (reviewed in Ames37 ), and inhibiting mitochondrial fission has been reported to be cardioprotective.50 Accordingly, our study demonstrated 2 beneficial effects of CoQ10 in vitro, namely, the prevention of mitochondrial dysfunction and oxidative stress and the suppression of the expression of prothrombotic markers relevant to the pathophysiology of APS (supplemental Figure 8). Clinical trials are required to evaluate the beneficial effects of CoQ10 supplementation in the treatment of APS patients.
In conclusion, our results support the following: (1) The binding of aPL-IgG to the monocyte membrane elicits a redox-sensitive signaling pathway that controls the procoagulant and proinflammatory phenotype of these cells in the setting of APS. (2) The occurrence of oxidative stress associated with an increased atherothrombotic risk in APS patients in vivo agrees with the induction of oxidative stress by IgG-APS in vitro. (3) Mitochondrial dysfunction is crucial in the pathophysiology of APS. The binding of aPL-IgG to the monocyte membrane compromises mitochondrial activity, and mitochondrial dynamics is altered toward enhanced rates of fission. (4) CoQ10 treatment ameliorates mitochondrial dysfunction and oxidative stress and reduces the expression of prothrombotic and proinflammatory markers. Thus, CoQ10 may be considered as a safe adjunct to standard therapies in APS patients, particularly in those suffering thrombosis.
The online version of the article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors acknowledge the excellent technical assistance of Dr Ester Peralbo with the confocal microscopy studies. They thank all patients and healthy subjects for participation in the study.
This work was supported by grants from the Junta de Andalucía (P08-CVI-04234 and PI0246/2009), the Ministry of Health (PS09/01809), and the Ministry of Science and Innovation (BFU2011-23578) of Spain. C.L.-P. was supported by a contract from the Junta de Andalucía government of Spain.
Authorship
Contribution: C.P.-S. and P.R.-L. developed the in vivo assays, performed the experiments, and solved technical problems; M.A.A., M.L.B., M.A.K., and M.J.C. followed up with patients and contributed useful discussion and suggestions; A.R.-A., J.M.V., and C.L.-P. formed the hypothesis, directed and coordinated the project, designed the experiments, analyzed the data, and wrote the manuscript; P.S. and E.C.-E. performed clinical analysis and contributed useful suggestions; N.B. and F.V. performed statistical analysis and discussed results; and H.K. and J.A.G.-R. performed some experiments and analyzed the data.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Chary López-Pedrera, IMIBIC, Hospital Reina Sofía, Avda Menéndez Pidal s/n, E-14004 Córdoba, Spain; e-mail: rosario.lopez.exts@juntadeandalucia.es.
References
Author notes
C.P.-S. and P.R.-L. contributed equally to this work.




This feature is available to Subscribers Only
Sign In or Create an Account Close Modal