Abstract
Adult T-cell leukemia/lymphoma (ATLL) is an intractable hematologic malignancy caused by human T-lymphotropic virus type 1 (HTLV-1), which infects approximately 20 million people worldwide. Here, we have explored the possible expression of cancer/testis (CT) antigens by ATLL cells, as CT antigens are widely recognized as ideal targets of cancer immunotherapy against solid tumors. A high percentage (87.7%) of ATLL cases (n = 57) expressed CT antigens at the mRNA level: NY-ESO-1 (61.4%), MAGE-A3 (31.6%), and MAGE-A4 (61.4%). CT antigen expression was confirmed by immunohistochemistry. This contrasts with other types of lymphoma or leukemia, which scarcely express these CT antigens. Humoral immune responses, particularly against NY-ESO-1, were detected in 11.6% (5 of 43) and NY-ESO-1–specific CD8+ T-cell responses were observed in 55.6% (5 of 9) of ATLL patients. NY-ESO-1–specific CD8+ T cells recognized autologous ATLL cells and produced effector cytokines. Thus, ATLL cells characteristically express CT antigens and therefore vaccination with CT antigens can be an effective immunotherapy of ATLL.
Introduction
Adult T-cell leukemia/lymphoma (ATLL) is a distinct hematologic malignancy caused by human T-lymphotropic virus type 1 (HTLV-1).1,2 HTLV-1 is endemic in southwestern Japan, Africa, South America, and the Caribbean Islands, and approximately 20 million people worldwide are infected.3 A total of 5% of the infected persons develop ATLL after a long latency period.2 ATLL cells are CD4-positive; and the majority, if not all, of them express the transcription factor FoxP3 (Forkhead Box P3), CD25, CTLA-4, and CCR4 (CC chemokine receptor 4), and are functionally immunosuppressive, thus phenotypically and functionally resembling naturally occurring regulatory T cells (Tregs).3-9 Because of its immunosuppressive property and resistance to conventional chemotherapy, aggressive ATLL has a poor prognosis with a mean survival time of less than 1 year.2,8 A recent phase 3 trial of a dose-intensified multidrug chemotherapy for untreated ATLL patients (acute, lymphoma, and unfavorable chronic types) showed a median progression-free and overall survival of only 7.0 and 12.7 months, respectively.10 This and other reports indicate that chemotherapy alone is of limited success for ATLL and mostly fails to cure the disease.10,11 Allogeneic hematopoietic stem cell transplantation has been introduced over the past decade as a potential therapy for ATLL with a long-term remission in only a small fraction of patients who are young, well controlled in disease progression, and have an appropriate stem cell source.12 More effective strategies to treat ATLL are therefore required.
Several HTLV-1 components have been explored as targets for immunotherapy of ATLL. HTLV-1 Tax, which is crucial for ATLL oncogenesis, has generally been considered to be a main target of the host's cellular immune responses. Yet, the frequency of Tax expression in HTLV-1 infected cells reduces in the course of disease progression, and Tax transcripts are detected only in approximately 40% of the established ATLL cases,13 thus limiting Tax-targeted immunotherapy to a subset of patients. HBZ (HTLV-1 bZIP factor), another HTLV-1 component, which contains an N-terminal transcriptional activation domain and a leucine zipper motif at its C-terminal, also plays an important role in the proliferation of ATLL cells and is detectable in almost all ATLL cases.2 However, CD8+ T cells specific for HBZ could only recognize peptide-pulsed target cells but not ATLL cells themselves.14 Furthermore, HTLV-1 is transmitted mainly from mothers to infants through breast milk, and such vertical infection in early life may induce tolerance to the virus and result in insufficient HTLV-1–specific T-cell responses.15,16 For these reasons, targeting the HTLV-1 components alone may be insufficient for successful immunotherapy of ATLL, necessitating identification of novel tumor-associated target antigens for the immunotherapy.
The expression of cancer/testis (CT) antigens, of which more than 100 have been identified so far, is normally limited to human germ line cells in the testis and in various types of human cancers.17,18 This restricted expression pattern in normal tissues makes them ideal cancer antigens for tumor immunotherapy. NY-ESO-1 and MAGE family antigens, a subset of CT antigens, are indeed able to elicit spontaneous humoral and cellular immune responses in cancer patients.17-19 Clinical trials of CT antigen vaccination are currently under way with several types of vaccine formulation, including peptide, protein, and DNA, and some of the treated patients have experienced clinical benefits from vaccination.19,20 This promising result of CT antigens as a target of tumor immunotherapy has prompted intensive studies of their expression in a wide range of human cancers. However, detailed analysis of CT antigen expression in hematologic disorders has been limited.21,22 In the present study, we have investigated possible expression of CT antigens by ATLL cells and possible humoral and cellular immune responses against CT antigens in ATLL patients.
Methods
Primary ATLL cells and peripheral blood
Blood or lymph node samples were obtained from ATLL patients, and mononuclear cells were isolated with Ficoll-Paque. Diagnosis and classification of clinical subtypes of ATLL were according to the criteria proposed by the Japan Lymphoma Study Group.23 All donors provided informed written consent before sampling according to the Declaration of Helsinki, and the present study was approved by the institutional ethics committees of Nagoya City University Graduate School of Medical Sciences, Osaka University, and Imamura Bun-in Hospital.
ATLL cell lines
ATN-1, ATL102, HUT102, MT-2, and MT-1 were previously described.24,25 TL-Om1 and TL-Su were kindly provided by the Cell Resource Center for Biomedical Research, Tohoku University (Sendai, Japan). MT-4 was purchased from the Health Science Research Resources Bank (Osaka, Japan). MJ was purchased from ATCC. TCL-Kan was kindly provided by Professor M. Kannagi (Tokyo Medical and Dental University, Tokyo, Japan).
Reagents
Phycoerythrin-conjugated anti–IFN-γ (4S.B3) mAb and phycoerythrin-cyanine7–conjugated anti–TNF-α (MAb11) mAb were purchased from eBioscience. Fluorescein isothiocyanate-conjugated anti–IL-2 (MQ1-17H12) mAb and allophycocyanin-cyanine7–conjugated anti-CD8 (SK1) mAb were purchased from BD Biosciences. Anti–NY-ESO-1 mAb (E978, mouse IgG1)26 and pan-MAGE mAb (57B, mouse IgG1)27 were purified from hybridoma supernatant by protein G affinity chromatography. Synthetic peptides of NY-ESO-11-20 (MQAEGRGTGGSTGDADGPGG), NY-ESO-111-30 (STGDADGPGGPGIPDGPGGN), NY-ESO-121-40 (PGIPDGPGGNAGGPGEAGAT), NY-ESO-131-50 (AGGPGEAGATGGRGPRGAGA), NY-ESO-141-60 (GGRGPRGAGAARASGPGGGA), NY-ESO-151-70 (ARASGPGGGAPRGPHGGAAS), NY-ESO-161-80 (PRGPHGGAASGL- NGCCRCGA), NY-ESO-171-90 (GLNGCCRCGARGPESRLLEF), NY- ESO-181-100 (RGPESRLLEFYLAMPFATPM), NY-ESO-191-110 (YLAMPFATPMEAELARRSLA), NY-ESO-1101-120 (EAELARRSLAQDAPPLP- VPG), NY-ESO-1111-130 (QDAPPLPVPGVLLKEFTVSG), NY-ESO-1119-143 (PGVLLKEFTVSGNILTIRLTAADHR), NY-ESO-1131-150 (NILTIRLTAADHRQLQLSIS), NY-ESO-1139-160 (AADHRQLQLSISSCLQQLSLLM), NY-ESO-1151-170 (SCLQQLSLLMWITQCFLPVF), and NY-ESO-1161-180 (WITQCFLPVFLAQPPSGQRR) were obtained from Invitrogen.
RT-PCR
Total RNA was isolated with RNeasy Mini Kit (QIAGEN). cDNA was synthesized from 0.1 μg of total RNA using SuperScript III reverse transcriptase kit (Invitrogen) and the Oligo (dT) primer in a total volume of 20 μL. cDNA was amplified in a final volume of 20 μL containing 10μM of each CT antigen primer as reported,21,28 except NY-ESO-1 (sense, 5′-AGT TCT ACC TCG CCA TGC CT-3′; antisense, 5′- TCC TCC TCC AGC GAC AAA CAA-3′) and 0.2 μL of Ex-Taq polymerase (Takara Bio) according to the instructions provided by the manufacturer.
ELISA
Patients' sera were analyzed by ELISA for seroreactivity to bacterially produced recombinant proteins NY-ESO-1/CTAG1B, MAGE-A1, MAGE-A3, MAGE-A4, MAGE-A10, CT7/MAGE-C1, CT10/MAGE-C2, SSX1, SSX2, and SSX4.29 Sera were diluted serially from 1/100 to 1/100 000 and added to low-volume 96-well plates (Corning Life Sciences) coated overnight at 4°C with 1 μg/mL antigen in 25 μL volume and blocked for 2 hours at room temperature with PBS containing 5% nonfat milk. After overnight incubation, plates were extensively washed and rinsed with PBS. Antigen-specific IgG was detected with specific mAb conjugated with alkaline phosphatase (Southern Biotechnology). After addition of ATTOPHOS substrate (Fisher Scientific), absorbance was measured using a fluorescence reader Cytofluor Series 4000 (PerSeptive Biosystems). A reciprocal titer was calculated for each sample as the maximal dilution still significantly reacting to a specific antigen. This value was extrapolated by determining the intersection of a linear trend regression with a cutoff value. The cutoff was defined as 10 times the average of optical density (OD) values from the first 4 dilutions of a negative control pool made of 5 healthy donor sera. In each assay, sera of patients with known presence or absence of specific reactivity were used as controls.
Immunohistochemistry
All tissue specimens were fixed with formalin and embedded in paraffin. Tissue sections of 3 μm thickness on charged glass slides were deparaffinized and rehydrated. Antigen retrieval was performed by autoclave (105°C for 20 minutes) using Tris-EDTA buffer (pH 9.0) as heating solution. Primary mAb for NY-ESO-1 (E978) and pan-MAGE protein (57B) were used at concentrations of 5 μg/mL and 2 μg/mL, respectively. Endogenous peroxidase activity was blocked with 3% hydrogen peroxidase and 1% sodium azide. Simple stain max-PO (Multi; Nichirei) was used for secondary detection; 3,3′-diamino-benzidine was used as chromogen. Human testicular tissue served as positive control. All histological pictures were captured by NIKON Eclipse microscope and NIKON Image software system (Version 3.22).
In vitro sensitization
NY-ESO-1–specific CD8+ and CD4+ T cells were presensitized as described previously.30,31 Briefly, CD8+ T cells and CD4+ T cells were isolated from peripheral blood mononuclear cells (PBMCs) using a CD8 Microbeads and a CD4+ T cell Isolation Kit, respectively (Miltenyi Biotec). The purity of isolated populations was confirmed to be more than 90%. The non-CD8+/CD4+ cell population was pulsed with 10μM of pooled peptides overnight and was used as antigen-presenting cells (APCs). After irradiation, 5 to 10 × 105 APCs were added to round-bottom 96-well plates (Corning Life Sciences) containing 1 to 5 × 105 CD8+ or CD4+ T cells and were fed with IL-2 (10 U/mL; Roche Diagnostics) and IL-7 (20 ng/mL; R&D Systems). Subsequently, one-half of the medium was replaced by fresh medium containing IL-2 (20 U/mL) and IL-7 (40 ng/mL) twice per week.
Intracellular cytokine staining
CD8+ T cells from PBMCs from ATLL patients were presensitized for 10 to 18 days. These presensitized CD8+ T cells were restimulated for 6 hours with peptide-pulsed T-APCs,31 and GolgiStop reagent (BD Biosciences) was added 1 hour later. Cells were stained for cell surface markers and for intracellular cytokines, such as IFN-γ and TNF-α after permeabilization. Results were analyzed by flow cytometry (FACSCanto; BD Biosciences) and FlowJo Version 7.6.5 software for Macintosh (TreeStar).
Tetramer assay
Tetramer staining was performed as previously described.31 Briefly, presensitized CD8+ T cells were stained with phycoerythrin-labeled tetramers (prepared by Drs P. Guillaume and I. Luescher at the Ludwig Institute Core Facility, Lausanne, Switzerland) for 15 minutes at 37°C before additional staining with allophycocyanin-cyanine7–conjugated anti-CD8 mAb for 15 minutes at 4°C. After washing, results were analyzed by FACSCanto and FlowJo Version 7.6.5 software.
Statistical analysis
The significance of the difference in each CT antigen expression between 2 groups was assessed by Fisher exact test. P values less than .05 were considered significant.
Results
A subset of CT antigens is highly expressed in ATLL cell lines
To examine possible expression of 11 CT antigens (NY-ESO-1, MAGE-A1, MAGE-A3, MAGE-A4, MAGE-A10, CT-7, CT-10, SSX-1, SSX-2, SSX-4, and SCP-1) by ATLL cells, we assessed mRNA expression by RT-PCR in 10 ATLL cell lines (MT-1, MT-2, MT-4, MJ, ATL102, ATN-1, TL-Om-1, TL-Su, TCL-kan, and HUT102). In sharp contrast to a previous report showing that the majority of T-cell lymphomas did not express CT antigens except SCP-1,21 a high percentage of ATLL cell lines expressed NY-ESO-1, MAGE-A3, and MAGE-A4 (90%, 50% and 70%, respectively) in the present study (supplemental Table 1, available on the Blood Web site; see the Supplemental Materials link at the top of the online article). SCP-1, another CT antigen, was also detected in 40% of ATLL cell lines, as in other T-cell lymphomas (supplemental Table 1).
NY-ESO-1, MAGE-A3, and MAGE-A4 are widely expressed in primary ATLL cells
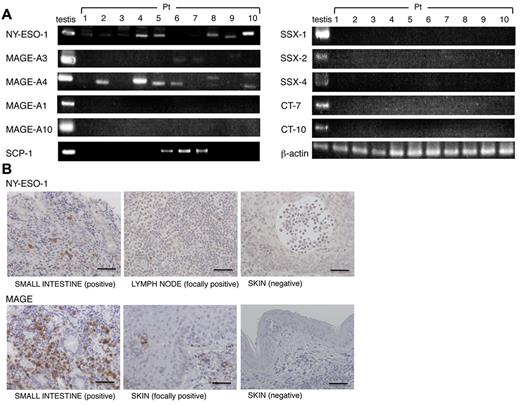
Given the high percentage of CT antigen mRNA expression in ATLL cell lines, we next examined the expression of 11 CT antigens in primary tumor cells from 57 individual ATLL patients. As shown in Figure 1A, Table 1, and supplemental Table 2, NY-ESO-1, MAGE-A3, and MAGE-A4 mRNA expression was detected in 61.4% (35 of 57), 31.6% (18 of 57), and 61.4% (35 of 57), respectively, of primary ATLL patients. SCP-1 expression was also detected in 23.2% (13 of 56). Among 4 subtypes (acute, lymphoma, chronic, and smoldering) of ATLL, the acute and lymphoma types show aggressive clinical courses (aggressive types), whereas the chronic and smoldering types progress more indolently (indolent types).2,23 There were no significant differences between the ATLL patients with aggressive and indolent types in the expression of NY-ESO-1, MAGE-A3, and MAGE-A4; yet there was a trend for more frequent expression of CT antigens in aggressive ATLL types (Table 1). Immunohistochemical analysis confirmed the expression of NY-ESO-1 and pan-MAGE at the protein level in samples available for pathologic analysis (Figure 1B). By contrast, expression of other CT antigens was limited: MAGE-A1, 8.8% (3 of 34); MAGE-A10, 0% (0 of 33); CT-7, 0% (0 of 33); CT-10, 0% (0 of 33); SSX-1, 0% (0 of 33); SSX-2, 0% (0 of 33); and SSX-4, 0% (0 of 33) by RT-PCR.
NY-ESO-1, MAGE-A3, and MAGE-A4 are widely expressed by primary ATLL cells. (A) Representative results of RT-PCR analysis for mRNA expression of NY-ESO-1, MAGE-A1, MAGE-A3, MAGE-A4, MAGE-A10, CT-7, CT-10, SSX-1, SSX-2, SSX-4, and SCP-1. (B) ATLL samples were subjected to immunohistochemical staining for NY-ESO-1 (E978) mAb and pan-MAGE (57B) mAb. Bar represents 50 μm. These experiments were performed independently at least twice with similar results.
NY-ESO-1, MAGE-A3, and MAGE-A4 are widely expressed by primary ATLL cells. (A) Representative results of RT-PCR analysis for mRNA expression of NY-ESO-1, MAGE-A1, MAGE-A3, MAGE-A4, MAGE-A10, CT-7, CT-10, SSX-1, SSX-2, SSX-4, and SCP-1. (B) ATLL samples were subjected to immunohistochemical staining for NY-ESO-1 (E978) mAb and pan-MAGE (57B) mAb. Bar represents 50 μm. These experiments were performed independently at least twice with similar results.
Summary of CT antigen expression in ATLL cells from primary ATLL patients
| . | No. of patients . | NY-ESO-1 . | MAGE . | |
|---|---|---|---|---|
| A3 . | A4 . | |||
| Age (mean, 60.6 y) | ||||
| ≥ 60 y | 29 | 20 | 12 | 20 |
| < 60 y | 28 | 15 | 6 | 15 |
| Sex | ||||
| Male | 30 | 17 | 8 | 17 |
| Female | 27 | 18 | 10 | 18 |
| Disease type | ||||
| Aggressive | 40 | 25 (62.5%) | 14 (35.0%) | 26 (65.0%) |
| Acute | 37 | 22 | 13 | 24 |
| Lymphoma | 3 | 3 | 1 | 2 |
| Indolent | 17 | 9 (52.9%) | 4 (23.5%) | 9 (52.9%) |
| Chronic | 11 | 7 | 2 | 8 |
| Smoldering | 6 | 3 | 2 | 1 |
| . | No. of patients . | NY-ESO-1 . | MAGE . | |
|---|---|---|---|---|
| A3 . | A4 . | |||
| Age (mean, 60.6 y) | ||||
| ≥ 60 y | 29 | 20 | 12 | 20 |
| < 60 y | 28 | 15 | 6 | 15 |
| Sex | ||||
| Male | 30 | 17 | 8 | 17 |
| Female | 27 | 18 | 10 | 18 |
| Disease type | ||||
| Aggressive | 40 | 25 (62.5%) | 14 (35.0%) | 26 (65.0%) |
| Acute | 37 | 22 | 13 | 24 |
| Lymphoma | 3 | 3 | 1 | 2 |
| Indolent | 17 | 9 (52.9%) | 4 (23.5%) | 9 (52.9%) |
| Chronic | 11 | 7 | 2 | 8 |
| Smoldering | 6 | 3 | 2 | 1 |
mRNA expression of NY-ESO-1, MAGE-A3, and MAGE-A4 in ATLL cells from primary ATLL patients was analyzed with RT-PCR. CT antigen expression was summarized based on several clinical parameters.
Taken together, CT antigens, such as NY-ESO-1, MAGE-A3 and MAGE-A4, are expressed in a significant fraction of primary ATLL cases, and 87.7% (50 of 57) of ATLL patients expressed at least one of these 3 CT antigens.
Humoral immune responses against NY-ESO-1 are detected in a subset of ATLL patients
We next asked whether ATLL patients spontaneously developed humoral and cellular immune responses specific for CT antigens. Serum samples from 43 primary ATLL patients were assessed by ELISA for the reactivity to 10 CT antigens (NY-ESO-1, MAGE-A1, MAGE-A3, MAGE-A4, MAGE-A10, CT-7, CT-10, SSX-1, SSX-2, and SSX-4). Significant antibody titers were detected against NY-ESO-1 in 5 of 43 (11.6%) patients and against MAGE-A1, MAGE-A3, and MAGE-A4 in 0% (0 of 43), 2.3% (1 of 43), and 0% (0 of 43), respectively (Figure 2). Humoral immune responses against CT antigens whose expression was not detected by RT-PCR (MAGE-A10, CT-7, CT-10, SSX-1, SSX-2, and SSX-4) were limited (Figure 2). These data collectively indicate that NY-ESO-1 expressed in primary ATLL cells elicits spontaneous antibody responses in ATLL patients as in patients with NY-ESO-1 expressing solid tumors.19
Humoral immune responses against NY-ESO-1 are detected in a subset of patients with ATLL. Sera were collected from 43 primary ATLL patients, and antibody responses against 10 CT antigens (NY-ESO-1, MAGE-A1, MAGE-A3, MAGE-A4, MAGE-A10, CT-7, CT-10, SSX-1, SSX-2, and SSX-4) were analyzed by ELISA as described in “ELISA.” This experiment was performed at least twice with similar results.
Humoral immune responses against NY-ESO-1 are detected in a subset of patients with ATLL. Sera were collected from 43 primary ATLL patients, and antibody responses against 10 CT antigens (NY-ESO-1, MAGE-A1, MAGE-A3, MAGE-A4, MAGE-A10, CT-7, CT-10, SSX-1, SSX-2, and SSX-4) were analyzed by ELISA as described in “ELISA.” This experiment was performed at least twice with similar results.
Cellular immune responses against NY-ESO-1 in ATLL patients
We then assessed CT antigen-specific cellular immune responses in ATLL patients. As the majority of ATLL patients are in a severe anemic state as a characteristic of the disease and also because of intensive chemotherapy, we collected PBMCs from patients in partial or complete remission, except patient 8 with an indolent ATLL type. Considering this limitation of available sample sizes and predominant humoral immune responses against NY-ESO-1, we focused on NY-ESO-1 as a parameter of cellular immune responses. With sufficient amounts of PBMCs from 9 ATLL patients (patients 1, 2, 4, 8, 13, 14, 19, 27, and 43), NY-ESO-1 expression by ATLL cells was confirmed by RT-PCR in each patient, except for patient 13 (no detection) and patient 43 (unavailability of sample; supplemental Table 2). CD8+ T cells were presensitized with autologous CD4−CD8− PBMCs pulsed with a pool of NY-ESO-1 peptides, and antigen-specific CD8+ T cells were analyzed with NY-ESO-1/HLA tetramers corresponding to the HLA allele of each patient. NY-ESO-1–specific CD8+ T cells were detected in ATLL patients 2, 4, 14, and 43 (Figure 3A). The results indicate that NY-ESO-1–specific CD8+ T-cell responses spontaneously develop in a subset of patients harboring NY-ESO-1 expressing ATLL.
NY-ESO-1–specific CD8+ T cells are detected in ATLL patients. CD8+ T cells derived from PBMCs of patients 1, 2, 4, 8, 13, 14, 19, 27, and 43 were presensitized by CD4− CD8− PBMCs pulsed with NY-ESO-1 peptides covering the entire sequence of NY-ESO-1 as described in “In vitro sensitization.” (A) Induction of specific CD8+ T cells was analyzed by staining with NY-ESO-1/HLA tetramers indicated. Cytokine (IFN-γ and TNF-α) secreting capacity of NY-ESO-1–specific CD8+ T cells was analyzed by intracellular cytokine staining for recognition of (B) autologous activated T-cell APCs pulsed with NY-ESO-1 peptides or (C) autologous ATLL cells. These experiments were performed independently at least twice with similar results.
NY-ESO-1–specific CD8+ T cells are detected in ATLL patients. CD8+ T cells derived from PBMCs of patients 1, 2, 4, 8, 13, 14, 19, 27, and 43 were presensitized by CD4− CD8− PBMCs pulsed with NY-ESO-1 peptides covering the entire sequence of NY-ESO-1 as described in “In vitro sensitization.” (A) Induction of specific CD8+ T cells was analyzed by staining with NY-ESO-1/HLA tetramers indicated. Cytokine (IFN-γ and TNF-α) secreting capacity of NY-ESO-1–specific CD8+ T cells was analyzed by intracellular cytokine staining for recognition of (B) autologous activated T-cell APCs pulsed with NY-ESO-1 peptides or (C) autologous ATLL cells. These experiments were performed independently at least twice with similar results.
NY-ESO-1–specific CD8+ T cells produce cytokines and recognize an autologous ATLL cell line
With the presence of NY-ESO-1–specific CD8+ T cells in ATLL patients, we further analyzed their cytokine production in response to a pool of NY-ESO-1 peptides or autologous tumor cells. Sufficient amounts of PBMCs for the cytokine analysis were available from 3 ATLL patients (patients 4, 14, and 19), in which NY-ESO-1 expression was confirmed by RT-RCR (supplemental Table 2). NY-ESO-1–specific CD8+ T cells were detected with NY-ESO-1/MHC tetramers in 2 of them (patients 4 and 14), but relevant tetramers were not available for another patient (patient 19). NY-ESO-1–specific CD8+ T cells prepared from these 3 patients by presensitization with NY-ESO-1 peptide-pulsed CD4−CD8− PBMCs produced IFN-γ and/or TNF-α by intracellular cytokine staining (Figure 3B). In patient 14, the frequency of NY-ESO-1–specific CD8+ T cells producing IFN-γ was much higher than NY-ESO-1–specific CD8+ T cells detected by NY-ESO-1/HLA-Cw*0304 tetramer, suggesting that this patient may have CD8+ T cells recognizing other epitopes of NY-ESO-1 (Figure 3A-B). Taken together, NY-ESO-1–specific CD8+ T cells were detected in 5 of 9 (55.6%) ATLL patients.
We also examined whether NY-ESO-1–specific CD8+ T cells from patient 4 recognized autologous ATLL cells. They produced IFN-γ and TNF-α against autologous ATLL cells expressing NY-ESO-1 but not against a control HLA-matched ATLL cell line (ATL-102) without NY-ESO-1 expression (Figure 3C). Collectively, these data indicate that NY-ESO-1–specific CD8+ T cells are present in ATLL patients and are able to recognize and kill autologous leukemic cells.
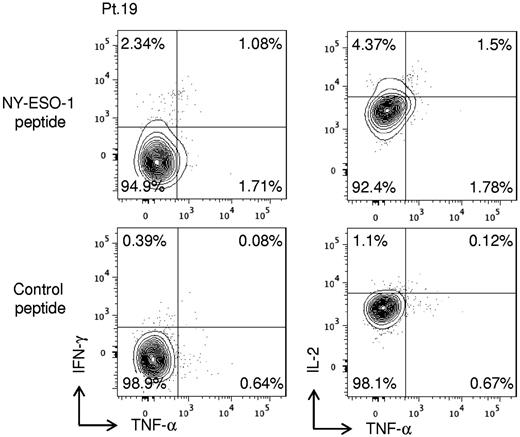
CD4+ T-cell responses against NY-ESO-1 in ATLL patients
To determine whether NY-ESO-1–specific CD4+ T cells were present in these ATLL patients, CD4+ T cells derived from PBMCs obtained from ATLL patients (patients 1, 2, 4, 8, 13, 14, 19, 27, and 43) were presensitized by CD4−CD8− PBMCs pulsed with a pool of NY-ESO-1 peptides, and assessed for cytokine production by intracellular cytokine staining. Of 9 patients, NY-ESO-1–specific CD4+ T cells were detected only in one patient (patient 19), who was in complete remission after receiving allogeneic hematopoietic stem cell transplantation (Figure 4). Thus, NY-ESO-1–specific CD4+ T cells are present in a subset of ATLL patients, but a much lower frequency than CD8+ T-cell responses, partly because the presence of ATLL cells, which are CD4+, may make the detection difficult and possibly because CD25+CD4+ Tregs are present in the CD4+ T-cell fraction.
NY-ESO-1–specific CD4+ T cells are present in an ATLL patient (patient 19) receiving an allogeneic hematopoietic stem cell transplantation. CD4+ T cells were presensitized by CD4− CD8− PBMCs pulsed with NY-ESO-1 peptide covering the entire sequence of NY-ESO-1 as described in “In vitro sensitization.” Induction of NY-ESO-1–specific CD4+ T cells was analyzed by intracellular cytokine staining using autologous activated T-cell APCs pulsed with NY-ESO-1 peptides. These experiments were performed independently twice with similar results.
NY-ESO-1–specific CD4+ T cells are present in an ATLL patient (patient 19) receiving an allogeneic hematopoietic stem cell transplantation. CD4+ T cells were presensitized by CD4− CD8− PBMCs pulsed with NY-ESO-1 peptide covering the entire sequence of NY-ESO-1 as described in “In vitro sensitization.” Induction of NY-ESO-1–specific CD4+ T cells was analyzed by intracellular cytokine staining using autologous activated T-cell APCs pulsed with NY-ESO-1 peptides. These experiments were performed independently twice with similar results.
Discussion
Since the initial description of ATLL as a unique type of T-cell leukemia/lymphoma,1 various therapeutic attempts have been made. Yet, the prognosis of ATLL is still poor despite advances in our knowledge regarding the oncogenic process of the disease.10,23 Here, we have examined CT antigen expression and its immunogenicity in ATLL patients to explore the potential for immunotherapy of ATLL by targeting CT antigens. We found that CT antigens, such as NY-ESO-1, MAGE-A3, and MAGE-A4, were highly expressed in ATLL. In particular, the frequencies of NY-ESO-1 and MAGE-A4 expression (61.4% and 61.4%, respectively) at the mRNA level were higher than or comparable to those in other malignancies. For example, the frequency of NY-ESO-1 and MAGE-A4 expression was 32% to 45% and 28%, respectively, in malignant melanoma, 24% to 33% and 63% to 90.2% in esophageal cancer, 30% to 43% and 57% in ovarian cancer, and 18% to 35% and 33% in bladder cancer.19,32,33 In addition, we have revealed that NY-ESO-1 was immunogenic in ATLL patients and elicited specific humoral and cellular immune responses in a subset of patients. These data strongly support CT antigens as novel targets for ATLL immunotherapy.
The frequency of humoral immune responses in ATLL patients was much higher against NY-ESO-1 compared with other CT antigens, such as MAGE-A3 and MAGE-A4. Although NY-ESO-1 expression by ATLL cells is presumably required for antibody induction, the level of NY-ESO-1 mRNA expression did not reflect the induction of humoral immune responses (supplemental Table 2). This lack of correlation appears in part to be the result of immunologic properties of NY-ESO-1 antigen itself.19,26 It has been shown that polymeric structures of NY-ESO-1 through disulfide bonds and their interaction with calreticulin-TLR4 on immature dendritic cell surface are required to induce phagocytosis of NY-ESO-1 protein and deliver danger signals for making the protein immunogenic.34 In addition, some non-MAGE-A members of the MAGE family are ubiquitously expressed and therefore possibly in more stable tolerance compared with NY-ESO-1. These properties of NY-ESO-1 and MAGE proteins might make the former more immunogenic than the latter.
Despite high immunogenicity of NY-ESO-1, the frequency (13.6%, 3 of 22) of primary ATLL patients who spontaneously developed NY-ESO-1 antibody responses against NY-ESO-1 expressing leukemic cells was lower compared with the frequencies in patients with malignant melanoma or non-small-cell lung cancers expressing NY-ESO-1 (∼ 50%).19,26 This may reflect the feature of ATLL that tumor cells from the majority of ATLL patients express Foxp3, a key transcription factor for CD25+CD4+ Tregs.6,9,35-37 ATLL cells from a subset of patients indeed appear to function as Tregs and contribute to profound immunosuppression that hampers the host's immune responses.6,36 Alternatively or additionally, the chemokine CCL22 produced by ATLL cells might enhance the migration of CCR4-expressing CD25+CD4+ Tregs to tumor sites.38 It remains to be determined whether Tregs in ATLL patients or ATLL cells themselves suppress NY-ESO-1–specific immune responses. Yet, it has been shown that helper T-cell responses against NY-ESO-1 are subject to active suppression by Tregs in patients with solid tumors and healthy persons.30,37 Further studies are required to understand immunosuppressive property of ATLL to enhance immune responses against CT antigens in ATLL patients.
NY-ESO-1–specific cellular immune responses were detected in a significant number (5 of 9, 55.6%) of ATLL patients in partial or complete remission. This indicates that reducing the number of ATLL cells before CT antigen-targeted immunotherapy may be a crucial component to successfully induce/augment antigen–specific CD8+ T cells. We have recently reported that humanized anti-CCR4 mAb, KW-0761, showed clinically significant antitumor activity as a salvage therapy for patients with relapsed ATLL.8,39 Patients 2, 4, and 14, from whom we detected NY-ESO-1–specific CD8+ T cells, were in complete or partial remission after anti-CCR4 mAb treatment.8,39 As CCR4 is expressed on ATLL cells as well as CD25+CD4+FOXP3+ Tregs, in addition to T-helper type 2 cells,8,40,41 anti-CCR4 mAb treatment can reduce not only ATLL cells but also endogenous CD25+CD4+FOXP3+ cells,42 thereby contributing to evoking NY-ESO-1–specific CD8+ T-cell responses. Indeed, the high frequency of NY-ESO-1–specific CD8+ T cells detectable in vitro in ATLL patients could be the result in part of the absence of Tregs. Thus, combining CT antigen-targeted immunotherapy after reduction of endogenous Tregs as well as ATLL cells by anti-CCR4 mAb treatment would be an ideal strategy for ATLL immunotherapy.
NY-ESO-1–specific CD4+ and CD8+ T-cell responses observed in patient 19 who was in a complete remission after allogeneic hematopoietic stem cell transplantation suggest an association of immune responses against CT antigens with a graft-versus-ATLL effect. This indicates that CT antigen-targeted immunotherapy combined with allogeneic stem cell transplantation may augment the efficacy of the current allogeneic hematopoietic stem cell transplantation for treating ATLL. In addition, as HTLV-1 Tax-specific CD8+ T cells reportedly contribute to graft-versus-ATLL effects,43 a combination immunotherapy with CT antigen and Tax after stem cell transplantation might also be therapeutically effective. Further, considering the reported high efficacy of NY-ESO-1–targeted adoptive T-cell therapy against malignant melanoma and synovial cell sarcoma,44,45 similar adoptive T-cell therapy for ATLL could also be effective.
ATLL is, to our knowledge, the first example of high expression of CT antigens in lymphomas or leukemia, as detailed analyses of CT antigen expression in other hematologic disorders have been limited.21,22 It contrasted with a previous report showing that T-cell lymphoma lacks expression of CT antigens, except SCP-1. As a probable mechanism for transcriptional activation of the CT antigen genes in malignant cells, it has been suggested that the expression of CT antigen is induced by CpG island hypomethylation at the promoter regions.18 An inflammatory environment created by infection may also trigger NY-ESO-1 expression. It cannot be excluded that viral components may promote this hypomethylation at the promoter regions or elicit inflammatory environment, thereby inducing CT antigen expression. Yet, we failed to observe any correlation between viral gene expression, such as Tax and HBZ and CT antigen expression (supplemental Table 2). In addition, high titers of HTLV-1 Gag/Env antibody responses were not associated with the induction of humoral immune responses against CT antigens (supplemental Table 2). Peripheral T-cell lymphomas, not otherwise specified (PTCL-NOS) are particularly heterogeneous; yet, the CCR4-positive subset of PTCL-NOS might be a distinct disease entity whose clinicopathologic features and genomic profiles were reportedly very similar to the lymphoma type of ATLL.24,46,47 PTCL-NOS, especially the CCR4-positive subset, have a very poor prognosis like ATLL, and no standard treatment strategies are available.48 Notably, we have found that CCR4-positive PTCL-NOS also expressed NY-ESO-1 at a high frequency (H.N., T.I., R.U. and S.S., unpublished data, August 2011). These data, when taken together, indicate that the frequent expression of CT antigens in ATLL may not be induced by HTLV-1 infection itself, but rather it may constitute a novel subtype of T-cell leukemia/lymphoma that expresses CCR4 and CT antigens regardless of HTLV-1 infection.
A small population (∼ 5%) of HTLV-1–infected persons progresses to ATLL after a long latency period of approximately 50 to 70 years.2 Although the detailed mechanisms of this leukemogenesis from HTLV-1 infection to ATLL have not yet been well elucidated, host immune responses against HTLV-1–infected cells have been suspected to play an important role.8,16,49 Interestingly, some of HTLV-1–infected asymptomatic HTLV-1 carriers harbored significant titers of antibody against NY-ESO-1, MAGE-A3, and MAGE-A4, despite that CT antigens, including NY-ESO-1, MAGE-A3, and MAGE-A4, were not detected at the mRNA level in their PBMCs (supplemental Figure 1). This discrepancy raises several possibilities; for example, the number or the frequency of HTLV-1–infected cells expressing CT antigens in circulating PBMCs may be too low to detect the antigen. Alternatively, it is possible that HTLV-1–infected cells expressing CT antigens may be eliminated in HTLV-1–infected asymptomatic carriers by anti-CT antigen-specific immune responses as tumor immunosurveillance,50 whereas antibody responses may linger on. Future studies with a large cohort of HTLV-1–infected asymptomatic carriers need to address the kinetics of their CT antigen expression during a long latency period and their immune responses against the antigen in the course of ATLL development. The studies will not only provide a rationale for including CT antigens as possible targets of ATLL immunotherapy but also contribute to our understanding of the multistep oncogenesis of ATLL and devising preventive strategies for ATLL by targeting CT antigens.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Dr J. B. Wing for helpful discussion and critical reading of this manuscript, Ms Y. Tada and Ms C. Sedrak for technical assistance, and Dr G. C. Spagnoli, Department of Surgery, University Hospital Basel, Basel, Switzerland, for the generous gift of 57B.
This article is dedicated to the memory of Dr Lloyd J. Old.
This work was supported by Grant-in-Aid for Specially Promoted Research (20002007, S.S.); Grants-in-Aid for Scientific Research (B: 23300354, H.N.; and 22300333, R.U.); Grants-in-Aid for Young Scientists (A: 22689029, T.I.); Scientific Support Programs for Cancer Research (221S0001, T.I.) from the Ministry of Education, Culture, Sports, Science and Technology of Japan; Grants-in-Aid for National Cancer Center Research and Development Fund (21-6-3, T.I.); Health and Labor Sciences Research (grants H22-Clinical Cancer Research-general-028, T.I.; H23-Third Term Comprehensive Control Research for Cancer-general-011, H.N., T.I., H.I., and A.U.) from the Ministry of Health, Labor and Welfare, Japan; the Cancer Research Institute Investigator Award (H.N.); Cancer Vaccine Collaborative Grant for Immunologic Monitoring (S.G. and L.J.O.); Cancer Research Grant from Foundation of Cancer Research Promotion (H.N.); the Sagawa Foundation for Promotion of Cancer Research (H.N.); and Senri Life Science Foundation (H.N. and S.S.).
Authorship
Contribution: H.N., T.I., S.G., L.J.O., R.U., and S.S. designed the research; H.N., Y.M., T.I., S.G., E.S., F.M., D.S., A.I., and Y.F. performed experiments; T.I., F.M., A.I, A.U., H.I., and R.U. collected samples and obtained clinical data; H.N., Y.M., T.I., S.G., E.S., Y.F., R.U., and S.S. analyzed data; and H.N., Y.M., T.I., S.G., E.S., R.U., and S.S. wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Shimon Sakaguchi, Experimental Immunology, Immunology Frontier Research Center, Osaka University, 3-1 Yamadaoka, Suita, Osaka 565-0871, Japan; e-mail: shimon@ifrec.osaka-u.ac.jp; and Ryuzo Ueda, Department of Medical Oncology and Immunology, Nagoya City University Graduate School of Medical Sciences, 1Kawasumi, Mizuho-cho, Mizuho-ku, Nagoya, Aichi, 467-8601, Japan; e-mail: ueda@med.nagoya-cu.ac.jp.
References
Author notes
H.N., Y.M., and T.I. contributed equally to this study.