Abstract
STEAP3/TSAP6 encodes a ferrireductase that is involved in the acquisition of iron by developing erythroblasts and steap3/tsap6 null-mice display severe microcytic anemia. We report a family in which 3 siblings born to healthy parents display transfusion-dependent hypochromic anemia. A nonsense STEAP3/TSAP6 was identified in the siblings at the heterozygous state. This mutation was inherited from their father while no mutation was found in their mother. A large variability of expression was found between normal alleles in a control population, confirming a previous report that STEAP3/TSAPS6 is an expressed quantitative trait locus (e-QTL). Determination of the relative allele expression showed that the “normal” allele was expressed at a significantly higher level in the father than in the affected siblings relative to the shared mutated allele. The blood level of STEAP3/TSAP6 mRNA was severely reduced in the siblings, while both parents were in the lower range of normal controls. The STEAP3/TSAP6 protein was also reduced in lymphocytic cell lines from the patients. Collectively, our data support the hypothesis that STEAP3/TSAP6 deficiency leads to severe anemia in the affected siblings and results from the combination of a mutated allele inherited from their father and a weakly expressed allele inherited from their mother.
Introduction
STEAP3/TSAP6 was primarily identified as a gene implicated in tumor reversion and a direct transcriptional target of p53.1 It encodes a 6-transmembrane domain protein that is involved in the regulation of the cell cycle, apoptosis2,3 and the secretion of proteins via the nonclassic pathway including the exosomes.4-7 Recently, Fleming and colleagues identified steap3/tsap6 as the gene responsible for anemia in nm1054 mutant mice.8 Hitherto, STEAP3/TSAP6 had not been shown to be associated with any human disease other than liver cancer.9 Inherited hypochromic anemia constitutes a genetically heterogeneous group of disorders resulting either from a defect in globin synthesis, as in thalassemias, or from a defect in heme synthesis. In the latter case, the genes currently known to be involved account for only a fraction of the cases, and include genes encoding enzymes of the heme biosynthesis pathway, and proteins controlling the availability of iron to the erythroid precursors.10
The dominant pathway for iron uptake11 in developing erythroblasts involves the transferrin cycle. The iron-loaded transferrin binds to transferrin receptor 1, inducing internalization of the complex by endocytosis. In the endocytic vesicle, ferric iron is released from transferrin by endosomal acidification and reduced to ferrous iron by the STEAP3/TSAP6 reductase before being transported to the cytoplasm by the divalent metal transporter DMT1.11 Hypochromic anemia5,12 and abnormal reticulocyte maturation, with impaired secretion of the transferrin receptor caused by a decreased production and secretion of exosomes5 have been documented in steap3/tsap6 deficient mouse strains.
Here we studied 3 siblings, 2 boys and a girl, born to healthy, unrelated parents of Pakistani origin. The siblings all had transfusion-dependent, poorly regenerative anemia and iron overload. By sequencing STEAP3/TSAP6 as a candidate gene, we found a heterozygous nonsense mutation in the 3 affected siblings. This mutation was inherited from their healthy father, and no mutation was found in their mother. Studies of STEAP3/TSAP6 expression in blood cells and immortalized lymphocytic cell lines of family members and normal controls were undertaken to test the hypothesis that the expression of the non mutated allele was lower in the affected children than in their father, thus accounting for the difference of phenotype.
Patients and methods
The study was approved by an Institutional Ethics Committee (Comité de Protection des Personnes). Informed consent was obtained from all the participants after a full explanation of the study in accordance with the Declaration of Helsinki.
Description of the family
The propositus II.1, born in 1985, is the first son of a couple who emigrated from Pakistan to Germany. No consanguinity was known. The parents originated from different cities in Pakistan, and met after they had immigrated independently to Germany. Development and growth were reported to be normal, but the boy had been pale since infancy. Anemia was first documented at the age of 7.5 years, with 3.6 × 1012 /L RBC and an initial hemoglobin (Hb) concentration of 98 g/L. Subsequent check-ups revealed chronic hypochromic anemia, and when the child was aged 12.6 years, a first attempt was made to classify his anemia. Physical examination was normal, except for distinct pallor of the skin and mucous membranes. The hemoglobin was 90 g/L, with a mean corpuscular volume (MCV) of 84 fL in the lower range of normal, and low mean corpuscular hemoglobin (MCH) of 25 pg. Reticulocytes were normal or inadequately increased up to 90 × 109 /L. Total bilirubin was not increased, with a value of 19 μM. Biochemical data suggested the onset of iron overload, with serum ferritin of 409 μg/L and transferrin saturation of 51%. Osmotic fragility and hemoglobin electrophoresis were normal; red cell enzyme activities (hexokinase, glucophosphate isomerase, triosephosphate isomerase, pyruvate kinase, glucose-6-phosphate dehydrogenase, glutathione reductase), were normal or increased. At this time there was no hepatosplenomegaly, but the spleen became palpable at the age of 19.
The patient was first seen by one of us (C. Balser) for increasing fatigue and pallor when he was 19 years old. His hemoglobin had dropped to 67 g/L and his MCV to 77 fL. Regular transfusions were given, maintaining Hb levels between 86 and 105 g/L, which permitted normal physical activity. Ferritin rose to a maximum of 1552 μg/L. After initiating treatment with erythropoietin-ζ (30 000 IU per week), the transfusion intervals extended to approximately 3 months, serum ferritin fell to 900-1000 μg/L, and then remained stable under continuous treatment with deferasirox. Additional data are shown in Table 1.
Clinical and laboratory data of the 3 siblings
| Identity . | Proband . | Sister . | Brother . | Mother . | Father . | ||||
|---|---|---|---|---|---|---|---|---|---|
| Age at first transfusion, y | 19.1 | 14.9 | 6.8 | ||||||
| Age at last transfusion, y | 24.5 | 23.3 | 18.1 | ||||||
| Total number of transfusions | 115 | 106 | 301 | ||||||
| Number of transfusions/y | 21.5 | 12.6 | 26.7 | ||||||
| Reference values | BFT | BLT | BFT | BLT | BFT | BLT | |||
| Hemoglobin, g/L | 120-150 | 67 | 88 | 60 | 92 | 46 | 94 | 125 | 146 |
| Erythrocytes, ×1012/L | 3.8-4.5 | 2.9 | 3.7 | 2.4 | 3.5 | 1.9 | 3.5 | ||
| Mean corpuscular volume, fL | 82-100 | 77 | 81 | 83 | 82 | 80 | 80 | 83 | 81 |
| Mean corpuscular Hb, pg | 27-32 | 23 | 24 | 25 | 26 | 24 | 26 | 28 | 28 |
| Reticulocytes, ×109/L | 50-100 | 38 | 37 | 14 | 35 | 19 | 21 | ||
| WBCs, ×109/L | 4.0-10 | 5.5 | 5.7 | 3.4 | 5.8 | 3.9 | 4.2 | 7.1 | 6.9 |
| Platelets, ×109/L | 150-400 | 301 | 183 | 307 | 197 | 247 | 152 | 239 | 319 |
| Bilirubin total, μmol/L | 5-20 | 19 | 23.6 | 8.6 | 12.3 | 8.6* | 9.2 | ||
| Lactate dehydrogenase, U/L | < 250 | 142 | 127 | 196 | 111 | 223 | 151 | ||
| GPT (ALT), U/L | < 45 | 35 | 100 | 6 | 77 | 19 | 92 | ||
| Serum iron, μmol/L | 11-36 | 244 | 36† | 46* | 38 | 37 | 34 | 5.5 | 19 |
| Serum ferritin, μg/L | 18-200 | 308 | 1552* | 258* | 2816 | 902 | 3157 | 14 | 160 |
| Serum transferrin, g/L | 2.0-3.7 | 1.8* | NA | 2.1* | 1.8 | 1.7 | 1.7 | ||
| Serum transferrin saturation, % | 20-50 | 83* | NA | 88* | 83 | 87 | 77 | ||
| Liver iron concentration, mg/g wet weight‡ | 0.1-0.5 | 2.3 | 2.9 | 4.4 | |||||
| Zinc protoporphyrin, μmol/mol heme | < 40 | ND | 90 | ND | 89 | ND | 44 | ||
| Serum hepcidin, μg/L | Males, 29-254; females, 16-288 | 64 | 405 | 284 | |||||
| Identity . | Proband . | Sister . | Brother . | Mother . | Father . | ||||
|---|---|---|---|---|---|---|---|---|---|
| Age at first transfusion, y | 19.1 | 14.9 | 6.8 | ||||||
| Age at last transfusion, y | 24.5 | 23.3 | 18.1 | ||||||
| Total number of transfusions | 115 | 106 | 301 | ||||||
| Number of transfusions/y | 21.5 | 12.6 | 26.7 | ||||||
| Reference values | BFT | BLT | BFT | BLT | BFT | BLT | |||
| Hemoglobin, g/L | 120-150 | 67 | 88 | 60 | 92 | 46 | 94 | 125 | 146 |
| Erythrocytes, ×1012/L | 3.8-4.5 | 2.9 | 3.7 | 2.4 | 3.5 | 1.9 | 3.5 | ||
| Mean corpuscular volume, fL | 82-100 | 77 | 81 | 83 | 82 | 80 | 80 | 83 | 81 |
| Mean corpuscular Hb, pg | 27-32 | 23 | 24 | 25 | 26 | 24 | 26 | 28 | 28 |
| Reticulocytes, ×109/L | 50-100 | 38 | 37 | 14 | 35 | 19 | 21 | ||
| WBCs, ×109/L | 4.0-10 | 5.5 | 5.7 | 3.4 | 5.8 | 3.9 | 4.2 | 7.1 | 6.9 |
| Platelets, ×109/L | 150-400 | 301 | 183 | 307 | 197 | 247 | 152 | 239 | 319 |
| Bilirubin total, μmol/L | 5-20 | 19 | 23.6 | 8.6 | 12.3 | 8.6* | 9.2 | ||
| Lactate dehydrogenase, U/L | < 250 | 142 | 127 | 196 | 111 | 223 | 151 | ||
| GPT (ALT), U/L | < 45 | 35 | 100 | 6 | 77 | 19 | 92 | ||
| Serum iron, μmol/L | 11-36 | 244 | 36† | 46* | 38 | 37 | 34 | 5.5 | 19 |
| Serum ferritin, μg/L | 18-200 | 308 | 1552* | 258* | 2816 | 902 | 3157 | 14 | 160 |
| Serum transferrin, g/L | 2.0-3.7 | 1.8* | NA | 2.1* | 1.8 | 1.7 | 1.7 | ||
| Serum transferrin saturation, % | 20-50 | 83* | NA | 88* | 83 | 87 | 77 | ||
| Liver iron concentration, mg/g wet weight‡ | 0.1-0.5 | 2.3 | 2.9 | 4.4 | |||||
| Zinc protoporphyrin, μmol/mol heme | < 40 | ND | 90 | ND | 89 | ND | 44 | ||
| Serum hepcidin, μg/L | Males, 29-254; females, 16-288 | 64 | 405 | 284 | |||||
BFT indicates before first transfusion; BLT, before last transfusion; GPT, glutamate pyruvate transaminase; ALT, alanine aminotransferase; NA, not available; ND, not determined.
More than 11 months before first transfusion.
More than 29 months before last transfusion.
Measured by biomagnetometry (SQUID).
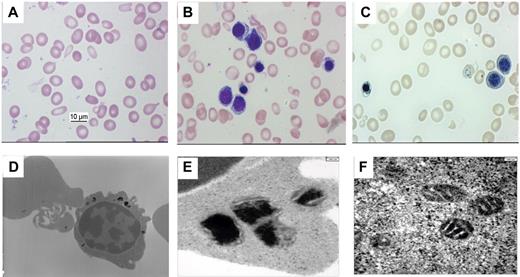
Blood smears (Figure 1A) revealed distinct aniso-poikilocytosis with hypochromasia, ovalocytes, a few target cells and basophilic, stippled cells. Single, mature nucleated red cells were present. There was moderate erythropoietic hyperplasia of the bone marrow, with dysplastic features in < 3% erythroblasts. Late basophilic and polychromatophilic erythroblasts had a small rim of poorly hemoglobinized cytoplasm, with small inclusions in some cells (Figure 1B). Perls' stain showed iron positive inclusions in most red cell precursors, with 40% ringed sideroblasts, and Pappenheimer bodies in a few red cells (Figure 1C). Under transmission electron microscopy, deposits of iron could be seen inside as well outside the mitochondria (Figure 1D-F).
Morphologic analysis of blood and bone marrow smears. (A) Morphology of red blood cells of the Propositus in peripheral blood smears shows distinct aniso-poikilocytosis, microcytosis, and hypochromasia. (B) Morphology of erythroblasts in bone marrow smears shows poor hemoglobinization with a ragged appearance of the cytoplasm (panoptic stain). (C) Perls' staining of bone marrow smears shows 2 basophilic erythroblasts without and 1 mature erythroblast with abnormally large siderotic granules, some of them clustered around the nucleus. One mature erythrocyte also displays multiple blue granules. (D) Transition electron micrograph of a polychromatophilic erythroblast (× 8000) showing many large siderotic granules. Top left: siderocyte. (E) Transition electron micrograph of an erythroblast (× 25 000) showing amorphous electron-dense material within structures suggestive of a lysosome or degenerative mitochondria. (F) Transition electron micrograph of an erythroblast (× 25 000) showing iron loaded mitochondria with retained cristae.
Morphologic analysis of blood and bone marrow smears. (A) Morphology of red blood cells of the Propositus in peripheral blood smears shows distinct aniso-poikilocytosis, microcytosis, and hypochromasia. (B) Morphology of erythroblasts in bone marrow smears shows poor hemoglobinization with a ragged appearance of the cytoplasm (panoptic stain). (C) Perls' staining of bone marrow smears shows 2 basophilic erythroblasts without and 1 mature erythroblast with abnormally large siderotic granules, some of them clustered around the nucleus. One mature erythrocyte also displays multiple blue granules. (D) Transition electron micrograph of a polychromatophilic erythroblast (× 8000) showing many large siderotic granules. Top left: siderocyte. (E) Transition electron micrograph of an erythroblast (× 25 000) showing amorphous electron-dense material within structures suggestive of a lysosome or degenerative mitochondria. (F) Transition electron micrograph of an erythroblast (× 25 000) showing iron loaded mitochondria with retained cristae.
The propositus has 2 younger siblings (Figure 2) with chronic hypochromic anemia and similar clinical, biochemical (Table 1) and morphologic data. His younger sister, II.2, born in 1987, had only mild symptoms of anemia and had her first menstruation at age 14. Menstruation stopped after 6 months. Her anemia became more severe, with a minimal hemoglobin level of 60 g/L, and regular transfusions were started when she reached the age of 15.
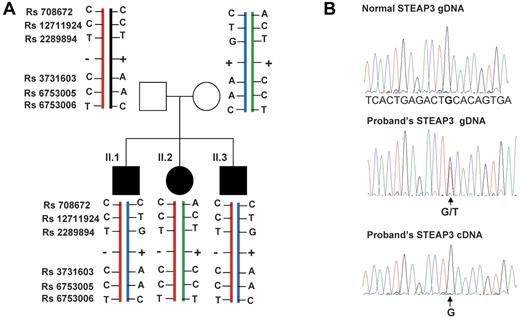
Pedigree of the family and transmission of the STEAP3/TSAP6 alleles. (A) The nonsense mutation p.C100X (−) was found in the heterozygous state in the 3 affected siblings and in their healthy father. + symbolizes the normal allele. Genotyping results of several common polymorphisms indicated that the mother transmitted the same STEAP3/TSAP6 haplotype to both her sons and the other haplotype to her daughter. Rs708672 and Rs12711924 are located in the promoter region and upstream of the gene, Rs2289894 is located in the first intron, Rs3731603, Rs6753005 and Rs3753006 are located in the 3′untranslated region. (B) Representative electrophoregrams of the normal and proband's genomic (gDNA) sequences, and the patients' cDNA sequence (sequence of the negative strand is shown). The arrow indicates the position of the heterozygous nucleotide substitution. The proband's cDNA sequence shows that only the normal allele is present at the cDNA level. The same results were obtained for the 3 affected sibling and for their father.
Pedigree of the family and transmission of the STEAP3/TSAP6 alleles. (A) The nonsense mutation p.C100X (−) was found in the heterozygous state in the 3 affected siblings and in their healthy father. + symbolizes the normal allele. Genotyping results of several common polymorphisms indicated that the mother transmitted the same STEAP3/TSAP6 haplotype to both her sons and the other haplotype to her daughter. Rs708672 and Rs12711924 are located in the promoter region and upstream of the gene, Rs2289894 is located in the first intron, Rs3731603, Rs6753005 and Rs3753006 are located in the 3′untranslated region. (B) Representative electrophoregrams of the normal and proband's genomic (gDNA) sequences, and the patients' cDNA sequence (sequence of the negative strand is shown). The arrow indicates the position of the heterozygous nucleotide substitution. The proband's cDNA sequence shows that only the normal allele is present at the cDNA level. The same results were obtained for the 3 affected sibling and for their father.
The younger brother, II.3, born in 1992, had a more severe form of anemia since infancy. In contrast to the older siblings, he displayed definite growth retardation. The minimum hemoglobin level was 51 g/L. With red cell transfusions, started when he was 7 years old, he was able to go to school and to take part in light sports. At age 18, he had massive hepatosplenomegaly, and high iron overload with a maximum ferritin value of 3157 μg/L. Café au lait blotches were visible on his skin.
The father was healthy, with normal blood counts and iron data. The mother had mild microcytic anemia with a low serum ferritin, which responded to iron supplementation. She had had 2 miscarriages in addition to her live births.
Hemoglobinopathies were excluded in the siblings by hemoglobin analyses including α and β multiplex ligation-dependent probe amplification (MLPA) and sequencing of the α and β globin genes.
Biochemical data suggested that iron overloading occurred before any transfusions had been given. Pyridoxine supplements were of no benefit. At the last follow-up, all 3 displayed high serum ferritin and low transferrin values as well as distinctly increased transferrin saturation despite regular treatment with deferasirox. They all had hypogonadism, with azoospermia in the males, and atrophy of the gonads in the girl. A complex dysfunction of the hypothalamo-pituitary-gonadal axis was seen in all 3, suggesting a primary defect of the gonads in addition to secondary hypogonadism. Latent adrenal and thyroid failure was detected in patient II 3. His pancreatic function was still normal, and there was no overt heart failure or pulmonary hypertension.
Oligonucleotides
All oligonucleotides sequences are listed in supplemental Table 1 (available on the Blood Web site; see the Supplemental Materials link at the top of the online article).
Immortalized cell lines
Lymphocytic cell lines from the patients and from their parents were established by transforming isolated peripheral lymphocytes with Epstein-Barr virus. To prevent nonsense-mediated mRNA decay, cells were cultured in the presence of α emetin for 24h as previously described13 before harvesting cells for mRNA analysis. RNA was extracted using RNAzol (Molecular Research Center), and treated with DNAse I to eliminate contaminating DNA.
Analysis of the STEAP3/TSAP6 gene and cDNA
Genomic DNA was extracted from peripheral blood using the QIAamp DNA blood Mini Kit (QIAGEN). Analysis of the STEAP3/TSAP6 gene (GenBank mRNA: NM_018234, UniprotKB protein: Q658P3) was performed by bidirectional direct sequencing. The exons of STEAP3/TSAP6, the promoter region from −896 relative to the transcriptional start point and the exon-intron junctions were amplified by PCR. After purification of the PCR products (PCR purification kit; QIAGEN), both strands were sequenced using a Big Dye Terminator Cycle Sequencing kit (Applied Biosystems, Life Technologies). Sequencing products were purified (Sephadex G50; GE Healthcare), and then analyzed using a 3130xl Genetic Analyzer and the Seqscape analysis software (v2.6.0; Applied Biosystems). Analysis of the entire cDNA was performed on reverse-transcribed mRNA extracted from emetin-treated lymphocytic cells (see preceding paragraph). Overlapping fragments were obtained by PCR, and the sizes of amplified products were verified by agarose gel electrophoresis before the fragments were purified and sequenced as described for genomic DNA.
Quantitative RT-PCR from blood cells
Blood was withdrawn into a Paxgene tube (QIAGEN), and the total RNA was extracted using a Paxgene kit (QIAGEN). After reverse transcription of 1 μg of total RNA with random hexamers, quantitative PCR was performed for STEAP3/TSAP6 cDNA using an ABI 7500 thermocycler. Beta2-microglobulin (B2M) was used as a reference mRNA. Real time quantitative PCR was carried out in triplicate, and mean values of STEAP3/TSAP6 and B2M were used for calculation of the ratio in each cDNA sample. The ratio of STEAP3/TSAP6 to B2M was calculated using the 2−ΔΔCT method.14
Quantification of relative allele expression
Relative expression of normal and mutated STEAP3/TSAP6 alleles.
To determine the ratio of mutated to normal STEAP3/TSAP6 allele expression in the siblings and in their unaffected father, a fragment of 420 nucleotides containing the heterozygous mutation was amplified from lymphocytic cell mRNA using the OneStep RT-PCR Kit (QIAGEN). Amplified products from genomic DNA and cDNA were sequenced, and the allele expression ratio was quantified using the “peak picker” software as described15 allowing for normalization of the mRNA allele ratio with the corresponding genomic DNA.
Allele expression ratio of STEAP3/TSAP6 in blood from normal controls.
Two fragments of the 3′UTR region of STEAP3/TSAP6 containing 2 different common SNPs (Rs6753006 and Rs3731603) were studied. RT-PCR was performed on mRNA from blood cells using the OneStep RT-PCR Kit (QIAGEN), and amplification of the corresponding fragments were carried out using genomic DNA from the same control subjects. Amplified products from genomic DNA and cDNA were sequenced, and the allele expression ratio was quantified as described in the preceding paragraph.
Immunoprecipitation
STEAP3/TSAP6 protein expression in lymphocytic cell lines.
Lymphocytic cells from controls, patients and their parents were treated with lysis buffer (PBS, 5mM EDTA, 0.5% Triton X-100) containing a cocktail of protease inhibitors (Roche Diagnostics). For each immunoprecipitation, cell lysates containing 3.7 mg proteins were incubated in the presence of 11.4 μg of anti-mSTEAP3/TSAP6 antibodies5 overnight at 4°C, followed by a 2-hour incubation with 20 μL protein A sepharose beads (GE Healthcare). The immunocomplexes were washed 3 times with lysis buffer, and then analyzed by Western blot using anti-mSTEAP3/TSAP6 antibodies.5
Results
Several candidate genes were sequenced from the proband's DNA (ALAS2, DMT1, SLC25A37, SLC25A38, SEC15L1, STEAP3/TSAP6, STEAP4). In addition to known common polymorphisms, the only sequence variation was a nonsense mutation in exon 3 of the STEAP3/TSAP6 gene: c.300 C > A, p.Cys100Stop (isoform b, Uniprot Q658P3) in the heterozygous state. This mutation was not present in the 1000 Genomes project database (http://browser.1000genomes.org/index.html), and we confirmed that it was also absent from 200 control chromosomes, which made it clear that this is not a common polymorphism. A family study showed that the same mutation was present in the heterozygous state in both the affected siblings and their unaffected father (Figure 2A). We sequenced a cDNA fragment containing exon 3 from blood mRNA of the affected siblings and of their unaffected father. In each of them, only the cDNA corresponding to the normal allele was detected (Figure 2B). This observation was not unexpected, and probably results from nonsense-mediated mRNA decay of the mutated mRNA.16 Sequence analysis of the mother's genomic DNA only detected heterozygosity for several common polymorphisms, and segregation analysis revealed that she had transmitted 1 STEAP3/TSAP6 allele to her daughter and the other allele to both her sons (Figure 2A). This ruled out the possibility that the mother had transmitted to her children a mutated allele that had not been identified by the sequencing analysis.
Recent studies indicate that a significant fraction of genes (5%-20%) display monoallelic expression or preferential expression of 1 of the 2 alleles.15,17-19 Interestingly, a literature search revealed that the STEAP3/TSAP6 gene had been identified as an expressed QTL showing an allele-specific level of expression associated with cis-linked polymorphisms.17 We therefore formulated the hypothesis that the difference in phenotype between the father and the 3 affected siblings, who all share the same nonsense mutation at the heterozygous state, may be explained by a difference in the expression level of the normal allele.
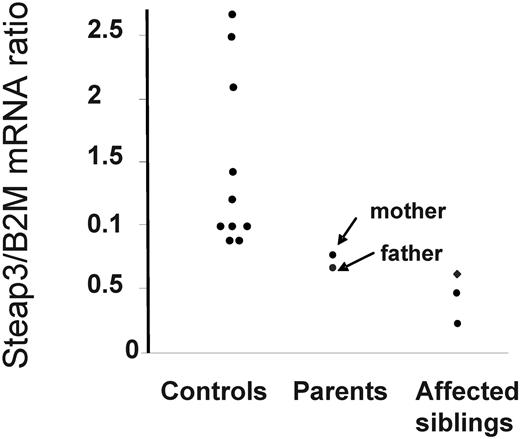
Quantitative RT-PCR from blood mRNA of all 5 family members and 10 normal controls revealed that the STEAP3/TSAP6 mRNA level was considerably lower in the 3 patients, while both parents had a level of STEAP3/TSAP6 mRNA corresponding to the lower range found in the normal controls (Figure 3).
Quantitative RT-PCR of STEAP3/TSAP6 mRNA from blood cells. The results of STEAP3/TSAP6 mRNA quantification are expressed in arbitrary units as the ratio of STEAP3/TSAP6 mRNA to B2M mRNA (STEAP3/B2M). Quantitative PCR was carried out for each cDNA sample, and the ratios of STEAP3 to the control gene B2M were calculated as the mean of triplicate determinations. A wide range of variation for 10 normal control subjects was observed (3-fold) and both parents were in the lower range of the controls. Note that in the father and in his 3 affected children, only the normal allele was detected by sequencing of RT-PCR products because of degradation of the mutated allele (Figure 2B).
Quantitative RT-PCR of STEAP3/TSAP6 mRNA from blood cells. The results of STEAP3/TSAP6 mRNA quantification are expressed in arbitrary units as the ratio of STEAP3/TSAP6 mRNA to B2M mRNA (STEAP3/B2M). Quantitative PCR was carried out for each cDNA sample, and the ratios of STEAP3 to the control gene B2M were calculated as the mean of triplicate determinations. A wide range of variation for 10 normal control subjects was observed (3-fold) and both parents were in the lower range of the controls. Note that in the father and in his 3 affected children, only the normal allele was detected by sequencing of RT-PCR products because of degradation of the mutated allele (Figure 2B).
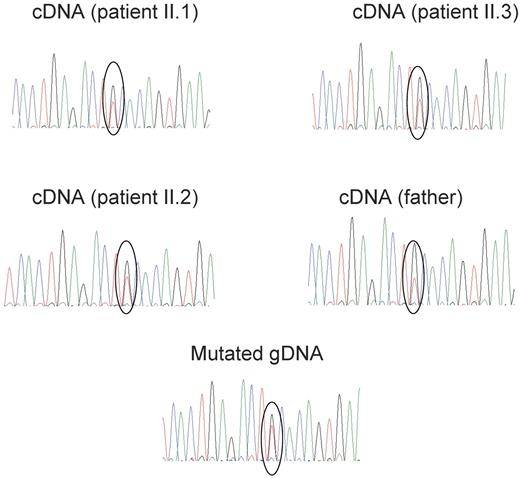
The relative allele expression in family members who are heterozygous for the p.Cys100Stop mutation could not be studied from blood mRNA, because the mutated mRNA was degraded. To circumvent this difficulty, B lymphocyte-cell lines established from the family members were treated with emetin for 24 hours before harvesting to prevent the degradation of the mutated allele resulting from nonsense mediated mRNA decay.13 Quantitative sequencing of a cDNA fragment encompassing the mutated nucleotide showed that the expression of the normal allele relative to that of the mutated allele was significantly higher in the father than in the 3 siblings (Figure 4). This finding was consistent with our hypothesis that the normal allele of the father is expressed at a higher level that either of the alleles from the mother.
Expression of normal and mutated STEAP3/TSAP6 alleles in lymphocytic cell lines from the father and the 3 affected children. Lymphocytic cell lines were cultured in the presence of emetin for 24 hours before being harvested, to prevent nonsense-mediated mRNA decay of the mutated mRNA. Electrophoregrams show that the ratio of the C (normal) to the A (mutated) allele is higher in the unaffected father than in his 3 affected offspring. Quantification of this expression ratio normalized for the C to A ratio in the mutated genomic DNA was performed using the “peak picker” software. Sequencing replicates from 3 independent RT-PCR were used to calculate the allelic ratios. The allelic ratios were 1.72 ± 0.05 in the father and 1.19 ± 0.03, 1.14 ± 0.027, 1.27 ± 0.032 in the affected children (mean ± SD). The difference between the father and each of his children was highly significant (P < .001, Student t test).
Expression of normal and mutated STEAP3/TSAP6 alleles in lymphocytic cell lines from the father and the 3 affected children. Lymphocytic cell lines were cultured in the presence of emetin for 24 hours before being harvested, to prevent nonsense-mediated mRNA decay of the mutated mRNA. Electrophoregrams show that the ratio of the C (normal) to the A (mutated) allele is higher in the unaffected father than in his 3 affected offspring. Quantification of this expression ratio normalized for the C to A ratio in the mutated genomic DNA was performed using the “peak picker” software. Sequencing replicates from 3 independent RT-PCR were used to calculate the allelic ratios. The allelic ratios were 1.72 ± 0.05 in the father and 1.19 ± 0.03, 1.14 ± 0.027, 1.27 ± 0.032 in the affected children (mean ± SD). The difference between the father and each of his children was highly significant (P < .001, Student t test).
We attempted to identify the cause of this differential expression in several ways. Firstly, the entire cDNA from family members was amplified by RT-PCR from emetin-treated lymphocytic cells to yield overlapping fragments that were analyzed by agarose gel electrophoresis and sequencing. These analyses indicated that only isoform b of STEAP3/TSAP6 was expressed, and did not reveal any qualitative transcript variation between family members, thus ruling out the possibility that differential alternative splicing could modulate STEAP3/TSAP6 allele expression, as previously shown for ferrochelatase.13 Furthermore, sequencing of cDNA from the mother revealed that several common polymorphisms were equally represented at the mRNA level. The absence of any abnormal transcript eliminates the possibility that some exon deletion at the heterozygous state could have escaped detection by sequencing genomic DNA. Secondly, the 3′untranslated region was entirely sequenced to exclude any sequence variation that could possibly modify the binding of miRNA, but only common polymorphisms were found that do not modify the potential predicted sites for miRNA binding. Thirdly, no sequence variation was found in the promoter region including 896 nucleotides upstream from the initiation of transcription.
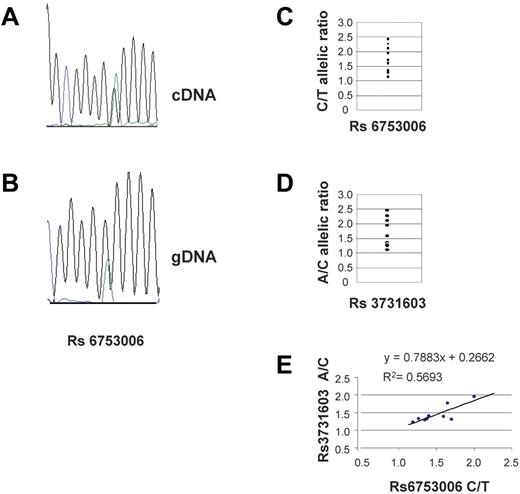
To confirm the variability of STEAP3/TSAP6 allele expression in the general population,17 we used 2 3′UTR common polymorphisms in high linkage disequilibrium as markers to perform quantitative sequencing of cDNA from blood using genomic DNA to normalize the results15 (Figure 5 A-B). Thus, the A/C and C/T allele ratios were determined for Rs 6753006 and Rs 3731603 from blood of 20 controls. The results indicated a 2.5 fold variation of these ratios among 17 individuals informative for Rs6753006 (Figure 5C) and 12 individuals informative for Rs 3731603 (Figure 5D). The results obtained from these 2 SNPs were in fair agreement in individuals heterozygous for both markers (r = 0.75; Figure 5E).
Relative expression of the STEAP3/TSAP6 alleles in normal controls. Electrophoregrams of sequencing reactions for cDNA (A) and genomic DNA (B) of a heterozygous control showing preferential allelic expression using the Rs6753006 SNP as a marker. The relative expression of the 2 alleles was calculated using the peak picker software for “quantitative” sequencing. The allelic expression ratio is indicated for 17 heterozygous controls for Rs6753006 (C) and for 12 heterozygous controls (D) for Rs3731603 (D). The correlation between the results obtained with the 2 markers is indicated for 9 controls who were heterozygous for both SNPs (E).
Relative expression of the STEAP3/TSAP6 alleles in normal controls. Electrophoregrams of sequencing reactions for cDNA (A) and genomic DNA (B) of a heterozygous control showing preferential allelic expression using the Rs6753006 SNP as a marker. The relative expression of the 2 alleles was calculated using the peak picker software for “quantitative” sequencing. The allelic expression ratio is indicated for 17 heterozygous controls for Rs6753006 (C) and for 12 heterozygous controls (D) for Rs3731603 (D). The correlation between the results obtained with the 2 markers is indicated for 9 controls who were heterozygous for both SNPs (E).
We investigated whether the preferential allele expression was subject to a parental effect by studying the parental origin of the alleles from 10 control trios (2 parents and 1 offspring), and we found that the higher expressed allele was not related to its parental origin (data not shown), thus ruling out the hypothesis of an imprinting effect.
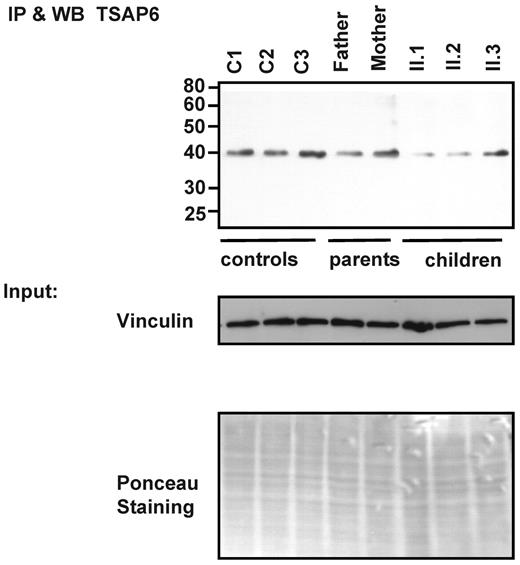
STEAP3/TSAP6 protein expression was also assessed in the B-lymphocyte cell lines from the patients and from their parents by immunoprecipitation and Western blot analysis. The anti-STEAP3/TSAP6 antibodies recognize a specific band of about 48 Kd. The STEAP3/TSAP6 protein was severely reduced in the siblings (Figure 6 and supplemental Figure 1).
STEAP3/TSAP6 protein expression in B-lymphocytic cell lines. Immunoprecipitation followed by Western blot analysis of the STEAP3/TSAP6 protein using anti-mSTEAP3/TSAP6 antibodies. STEAP3/TSAP6 is expressed in both parents but clearly decreased in the derived lymphocytic cell lines of the II.1 and II.2 siblings. Vinculin expression and Ponceau staining are shown for equal loading.
STEAP3/TSAP6 protein expression in B-lymphocytic cell lines. Immunoprecipitation followed by Western blot analysis of the STEAP3/TSAP6 protein using anti-mSTEAP3/TSAP6 antibodies. STEAP3/TSAP6 is expressed in both parents but clearly decreased in the derived lymphocytic cell lines of the II.1 and II.2 siblings. Vinculin expression and Ponceau staining are shown for equal loading.
All these findings are consistent with the hypothesis that the father is heterozygous with 1 null allele and 1 normal “highly expressed” allele, whereas the mother has 2 “weakly expressed alleles.” Each affected offspring had inherited the mutated allele from the father, and 1 of the “weakly expressed” alleles from the mother.
Discussion
Here, we report the first study of a family with a novel genetic form of severe hypochromic anemia associated with a nonsense mutation of the STEAP3/TSAP6 gene, a gene which encodes an iron reductase involved in iron acquisition by developing red blood cells. Although 3 affected siblings were born to healthy parents, suggesting a recessive mode of transmission, the STEAP3/TSAP6 nonsense mutation found in their DNA was in fact heterozygous, and inherited from the healthy father. Several lines of evidence support our current hypothesis that the anemia results from the coinheritance of a mutated allele from the father and a weakly expressed normal allele from the mother. First, we observed that the level of expression of the normal allele relative to that of the mutated one was higher in the unaffected father than in the 3 affected siblings; second, both the mother and the father had a STEAP3/TSAP6 mRNA level in blood cells that was in the lower range of the normal controls. Because the expression of the mutated allele is not detectable in blood mRNA from the father, this observation indicates that the expression of both the alleles from the mother produce an amount of mRNA that is roughly equivalent to the expression products from the single normal allele of the father. In agreement with expectations, the STEAP3/TSAP6 mRNA level in blood from the affected siblings was much lower than those of their parents, and this discrepancy was even more marked when the siblings were compared with normal controls. Protein expression, as estimated from lymphocytic cell lines from family members using a specific antibody, was in general agreement with mRNA expression.
Wide variability of STEAP3/TSAP6 expression was found in normal controls, thus confirming a previously published observation that the mRNA level of STEAP3/TSAP6 is strongly associated with cis-linked single nucleotide polymorphisms (SNPs) located in the 3′ region of the gene.17 Specific or preferential expression of a particular allele resulting from DNA sequence variations has recently been well documented by several studies at the level of the whole genome.18 There are many examples of this phenomenon, and in most cases, the level of allele expression was found to be linked to cis sequences (e-QTLs).18 The underlying mechanisms are potentially diverse. The causal polymorphism may affect regulatory sequences that are important for the transcription, splicing or stability of mRNA and in some cases it may be located in regulatory regions far from the gene itself.20 Furthermore, a recent study has shown that a SNP may cause differential methylation of 1 allele and consequently preferential allele expression resulting from a global change of the chromatin at the locus of interest.19 However, we were unsuccessful in our attempts to identify the molecular basis of the allelic variability of STEAP3/TSAP6 allele expression, and further work is required to clarify this point.
There are similarities between the biologic and clinical symptoms found in the 3 affected patients and the phenotype observed in mouse models with STEAP3/TSAP6 inactivation,5,8,12 including abnormal morphology and hypochromia of the red blood cells, and a spontaneous tendency to iron overload. Indeed, elevated serum ferritin levels were recorded before the onset of transfusions, although they were greatly increased by the transfusions. It is also possible that the STEAP3/TSAP6 deficiency accounts for the hypogonadism seen in our patients in addition to the effects of iron overload, in analogy to mouse models with steap3/tsap6 inactivation.5,8,12
The biologic and clinical phenotype of the patients described here resembles some aspects of cases of nonsyndromic congenital sideroblastic anemia (CSA; sideroblasts, iron overload). However, erythrocyte protoporphyrin was increased in our family, while it is normal or even low in CSA linked to either ALAS2 or SLC25A38 mutations.21 The observation of an increased protoporphyrin level is in keeping with the idea that STEAP3/TSAP6 deficiency limits the availability of ferrous iron for incorporation into protoporphyrin by ferrochelatase. Electron microscopy demonstrated the accumulation of iron in both siderosomic granules and mitochondria. In a context of deficient ferrireductase function, one would expect iron to accumulate in cytosolic vesicles, but mitochondrial iron accumulation can also be seen in conditions other than CSA, such as congenital dyserythropoietic anemia.22 No bone marrow specimens were available before severe transfusional iron overload had occurred.
There are numerous unexplained sporadic cases of CSA in the literature, as well as reports of families with CSA consistent with autosomal recessive inheritance,3 and it will be interesting to look for STEAP3/TSAP6 mutations in such families.
The coinheritance of a mutated and of a weakly expressed “normal” allele has previously been reported in hereditary spherocytosis23 and in erythropoietic protoporphyria.13 Both diseases are usually thought to be transmitted as autosomal dominant traits with incomplete penetrance (protoporphyria) or variable expressivity (dominant spherocytosis) although, recessive forms with biallelic mutations have been documented in both diseases.24,25
Such a mechanism could be relevant in other genetic diseases. Indeed, it is not uncommon in a recessive disease for a mutation to be identified in only 1 of the 2 alleles in a fraction of the patients. We suggest that in some cases this could be explained by genetic variations in allele expression, such as in the cases reported here.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors would like to thank the patients and all family members for kindly agreeing to participate in this study. Rosi Leichtle collected the clinical and biologic data. Barbara Schütz and Holger Christiansen kindly helped to retrieve all the data from the University Hospital in Marburg. Rainer Martin (Ulm) took the EM photographs, and Hans-Eckart Schaefer reviewed the EM photographs. Cells lines were established at the “banque des cellules” cell bank at Cochin hospital, Paris. Caroline Silve is thanked for providing helpful discussion and critical review of the manuscript.
The research was funded by a grant from the European rare disease project (ERARE-115, HMA-IRON) to C. Beaumont and B.G. A.T. and R.A. are supported by the European Union Conticanet Network of Excellence and the ANR Program Blanc (ANR-09-BLAN-0292-01).
This paper is dedicated to the memory of Gilles Hetet, who sadly died before the completion of this study.
Authorship
Contribution: B.G. designed the research, analyzed the data, and wrote the manuscript; G.H. and C.O. performed the research and analyzed the results; C.K. performed molecular diagnosis; C. Beaumont analyzed the data and wrote the manuscript; S.R.-F. and P.N. performed the research; R.A. and A.T. analyzed the data and wrote the manuscript; E.K. performed the globin studies; C. Balser and H.H. are involved in the clinical care of the patients; and H.H. made the conditional diagnoses, analyzed the data and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Bernard Grandchamp, Inserm U773, 16 rue Huchard, 75018 Paris, France; e-mail: bernard.grandchamp@bch.aphp.fr.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal